Summary Card
Anatomy of Flexor Tenosynovitis
The fibrous flexor sheath surrounds the flexor tendons and facilitates tendon gliding within a small volume of synovial fluid
Diagnosis of Flexor Tenosynovitis
The four pathognomonic signs according to Kanavel are fusiform swelling, pain along the flexor sheath, digit held in slight flexion, and pain on passive extension.
Flexor Tenosynovitis Treatment
A surgical emergency requiring admission, elevation, and IV antibiotics. A closed washout through a limited incision may be used, although it is prudent to keep a low threshold for subsequent open washout.
Complications of Flexor Tenosynovitis
Stiffness, adhesions, amputation, and skin loss are the primary complications.
Primary Contributor:
Dr Suzanne Thomson, Plastic Surgeon, Scotland.
Reviewer:
Dr Kurt Lee Chircop, Plastic Surgery Trainee, Malta.
Anatomy of Flexor Tenosynovitis
The fibrous flexor sheath surrounds the flexor tendons and facilitates tendon gliding within a small volume of synovial fluid. Infection can rapidly and proximally spread within these restricted spaces.
The flexor sheaths are a double-walled structure beginning at the metacarpal neck in the palm and extending just proximal to the distal interphalangeal joint. The thumb and little finger have bursae extensions, providing a route for proximal spread of infection, as illustrated below.
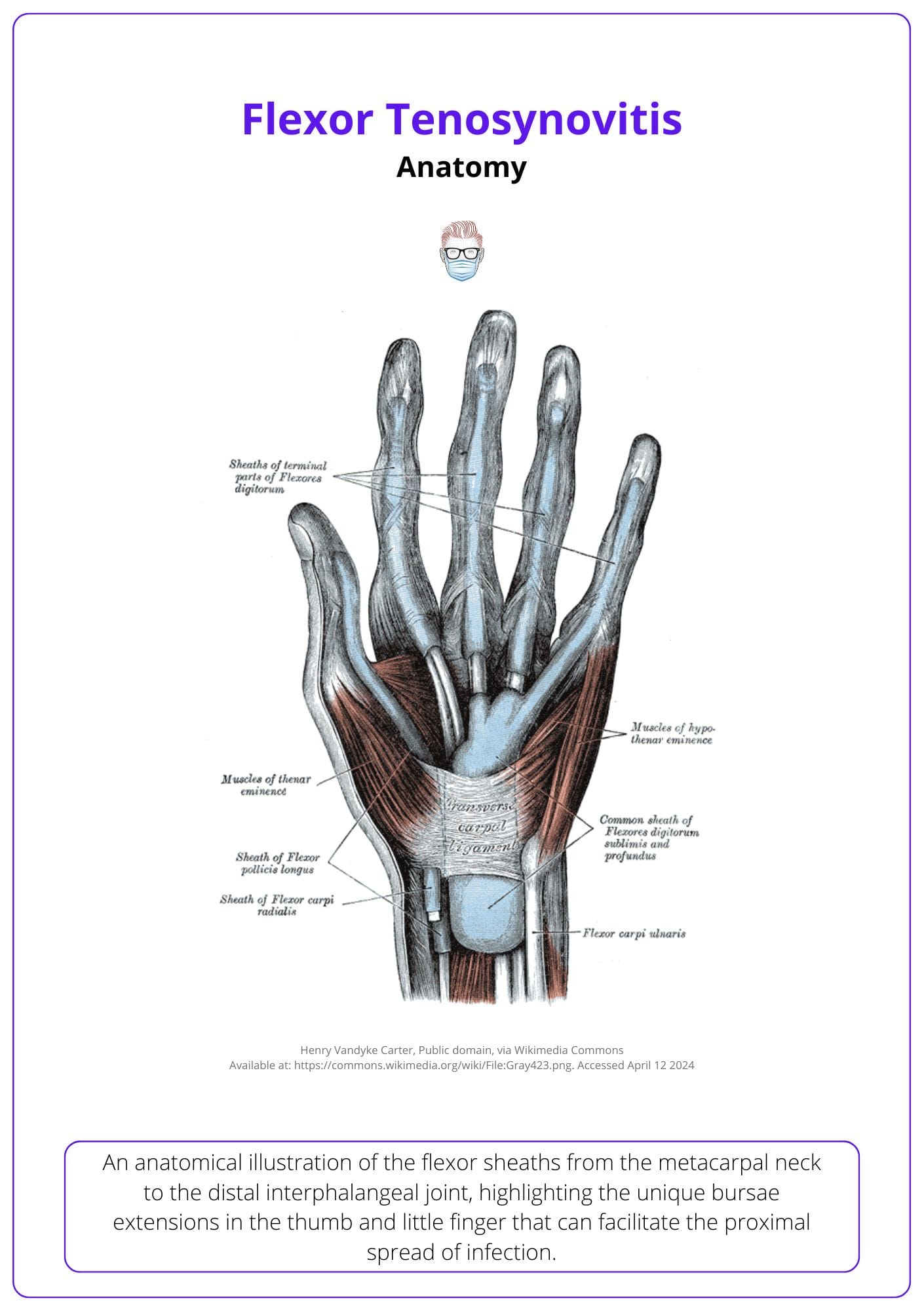
An anatomical study of 367 hands by Scheldrup, 1951 demonstrated that in the majority of cases these connect via the potential space of Parona (the space between pronator quadratus and FDP tendon sheath).
Read more about the anatomy of the flexor tendons and deep spaces of the hand in our zones of the hand article.
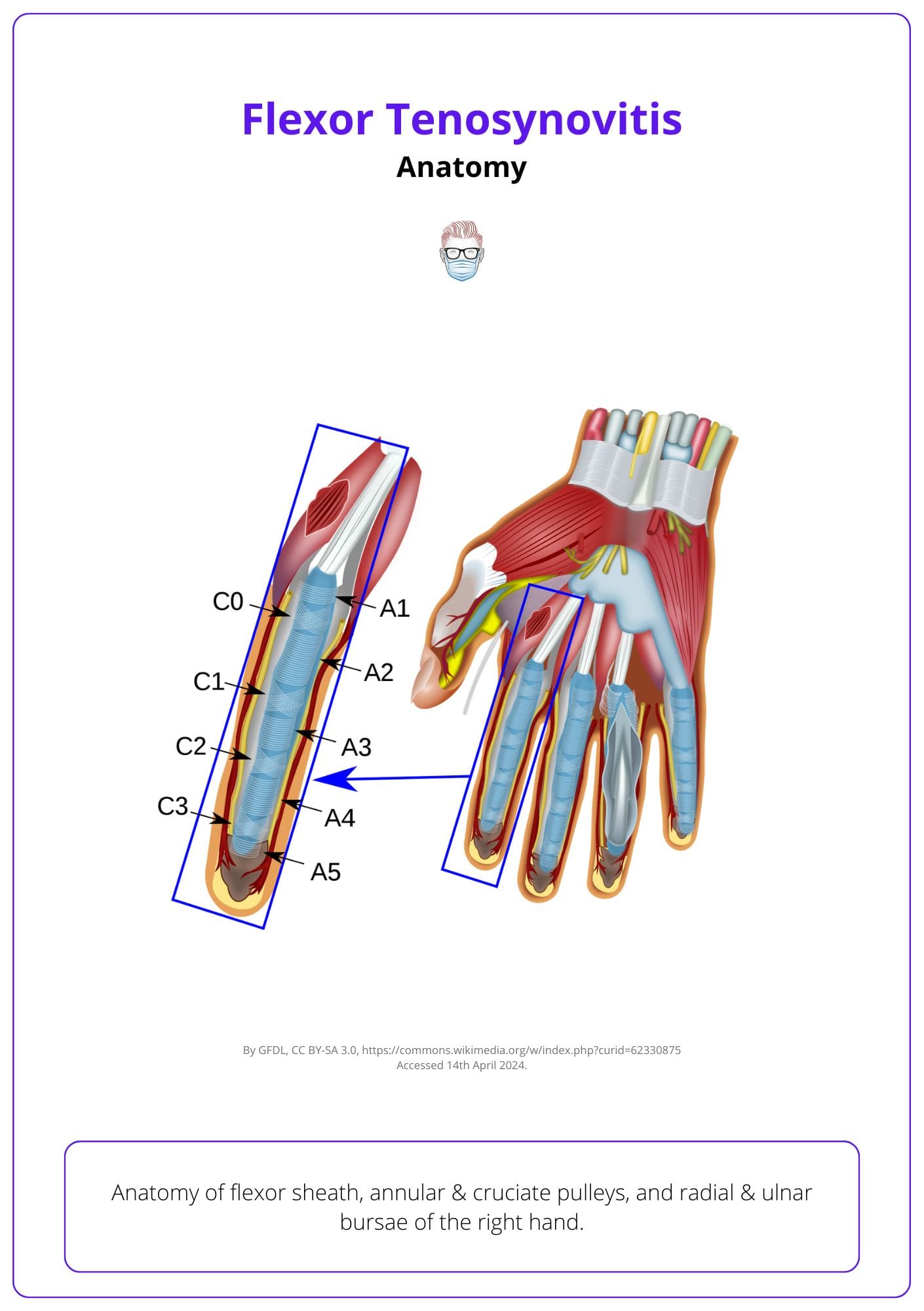
The image below illustrates the anatomy of the flexor sheath of the right hand.
Infections in the little finger or thumb can spread to the wrist via the radial and ulnar bursa, potentially causing a "horseshoe abscess" that may compromise the median nerve and require surgical decompression.
Diagnosis of Flexor Tenosynovitis
The classic presentation of pyogenic flexor tenosynovitis is Kanavel's signs: pain exacerbated on passive flexion, fusiform swelling & fixed position. Bloods (WCC, CRP, cultures) and imaging may support this diagnosis.
Signs and Symptoms
A classical history of penetrating trauma followed by increasing pain over the flexor aspect of the digit, swelling and reduced function in the days following are all red flags for potential pyogenic flexor tenosynovitis.
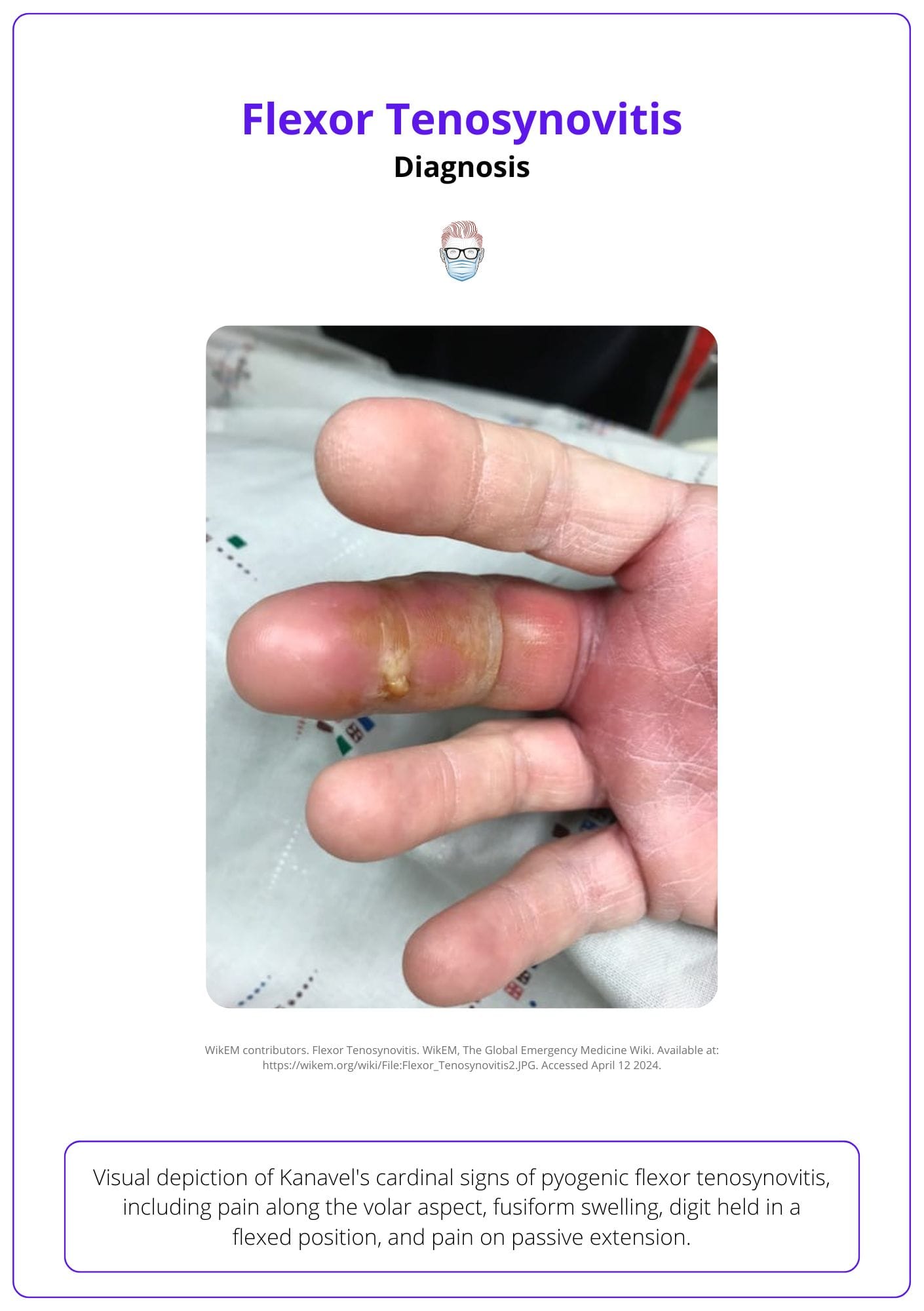
These features are commonly described as Kanavel's cardinal signs:
- Pain along the volar aspect of the digit
- Fusiform swelling
- Digit held in flexed position
- Pain on passive extension
Importantly, Kanavel’s signs are not uniformly present in children. Semiflexion of the digit being the least commonly observed sign (Brusalis, 2017).
Diagnosis may be complicated by co-morbid conditions, such as carpal tunnel syndrome or peripheral neuropathy, masking the classical symptoms and signs (Clements, 2019).
These clinical features of flexor tenosynovitis are illustrated in the image below.
Increasing age, polymicrobial infection, poorly controlled diabetes, immunosuppression, and peripheral vascular disease are risk factors for flexor tenosynovitis.
There may be no preceding traumatic injury, as cases of spontaneous PFT have been described.
Grading
There is a 3-point pre-operative severity grading system. The higher the grade of PFT, the worse the outcome (Pang, 2007). This is described below:
- Grade One: the presence of Kanavel’s signs
- Grade Two: Kanavel’s signs & subcutaneous purulence
- Grade Three: digital ischaemia.
Investigations
Pyogenic flexor tenosynovitis is primarily a clinical diagnosis. The following investigations may support the diagnosis:
- Inflammatory markers: raised CRP and WCC are suggestive of bacterial infection
- Blood cultures: the most common organisms are Staphylococcus & Strep. Vibrio species and anaerobes from animal bites, polymicrobial infection, or tetanus from human bites
- X-Ray: 3 views, excluding foreign bodies, soft tissue oedemia. Osteomyelitis/bone changes are not routinely seen in an acute presentation.
- Ultrasound: may demonstrate fluid in the flexor sheath and tendon changes and exclude other pathologies (eg: septic arthritis).
Differential Diagnosis
Flexor tenosynovitis has a classic presentation. If an atypical presentation, then please consider:
- Felon
- Paronychia
- Septic Arthritis
- Subcutaneous/Soft Tissue collection
- Collar button abscesses.
A Lund study indicated that purulent flexor tenosynovitis often suggests diabetes, as 23% of 39 patients had abnormal glucose tolerance, compared to 5% generally (Leden, 2009).
Flexor Tenosynovitis Treatment
Flexor tenosynovitis is a surgical emergency requiring admission, elevation, and IV antibiotics. Early aggressive surgical management is standard.
Pre-Operative
Early diagnosis should be made and the patient admitted for hand elevation, splinting in a safe position to reduce pain and stiffness, and empirical antibiotics.
- Antibiotics: Staphylococcus and streptococcus species should be covered in all cases, with the addition of gram-negative rods and anaerobes in immunocompromised patients (BSSH trauma guidance, 2024).
- Consent for subsequent washouts and also the potential for complications.
Please note: early presentations or where there is diagnostic uncertainty a trial of antibiotics may be used, however, early (within 24 hours) surgical washout is recommended in most cases.
With timely antibiotics and surgery 80% - 90% of individuals will recover full range of movement.
Intra-Operative
Prep:
- General, regional, and local anaesthetic techniques have been described for surgical decompression and washout.
- Tourniquet and Loupes are recommended.
Incisions:
- Open access via a Bruner's or midlateral incision or
- Limited incisions, like a chevron at the A1 pulley and a horizontal cut at the distal interphalangeal crease, should be designed for possible enlargement.
This intra-operative treatment strategy for Flexor Tenosynovitis is illustrated below.
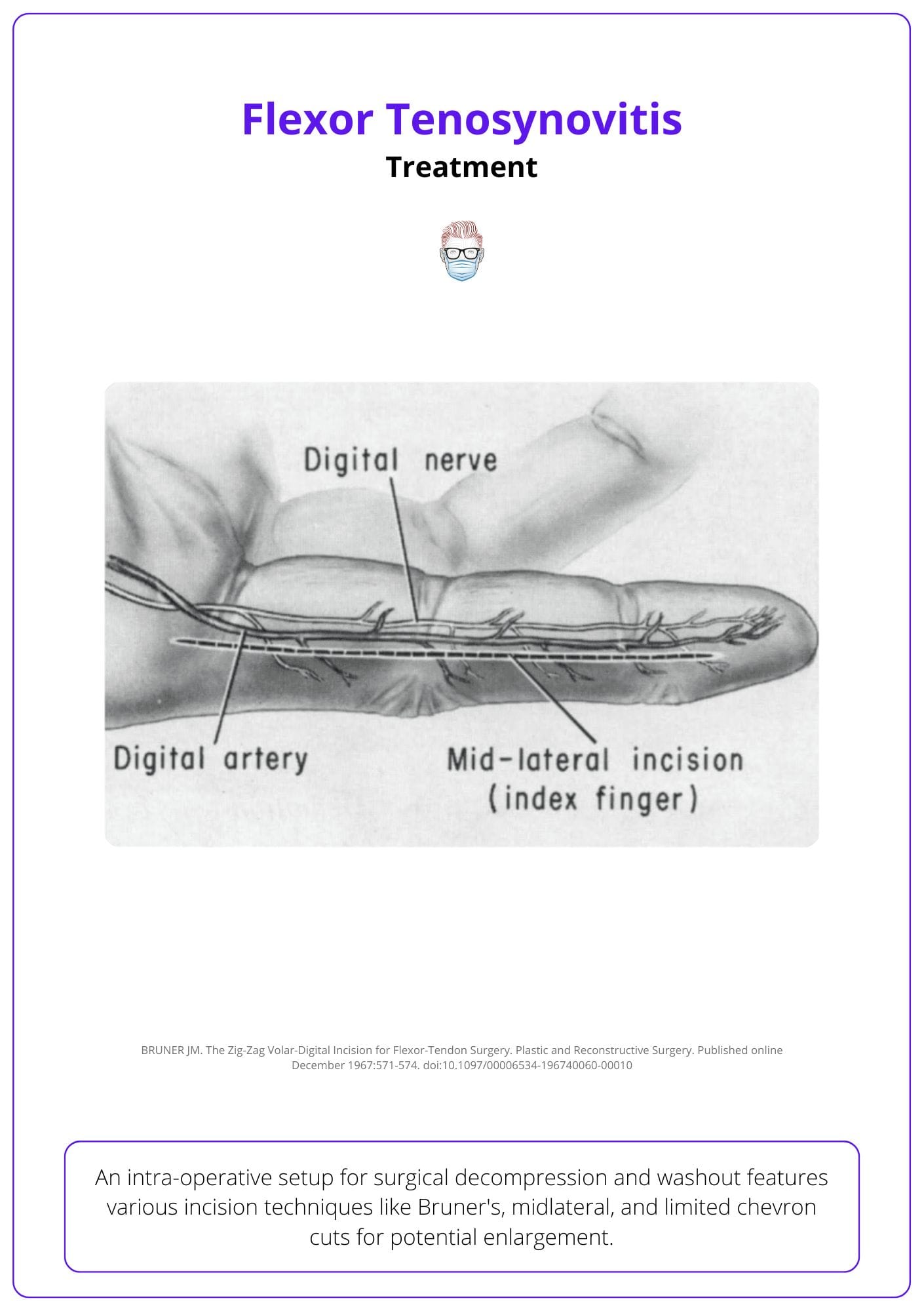
Extending the incision in a mid-lateral pattern protects the neurovascular bundles in the dorsal flap, provides complete access to the flexor sheath, and prevents tip necrosis associated with other flap pattern.
Washout and Cultures
- Cultures: Wound swabs should be sent for microbiology tests.
- Washout: large volume irrigation in a proximal to distal fashion.
Decompression of the carpal tunnel and washout of deep space of Parona is required in horseshoe abscesses.
Severity
Severity can be assessed during surgery using the Michon Classification system, which determines the necessary extent of surgical washout—limited washout for grade one—and predicts postoperative function, with higher scores indicating worse outcome).
The Michon Classification is as follows:
- Grade 1: increased serous fluid in the flexor sheath
- Grade 2: purulent fluid
- Grade 3: frank pus +/- tendon necrosis
Post-Operative
- Dressings: loosely dressed, and a resting splint may be used for comfort for the first 24 hours.
- Microbiology: targeted IV antibiotics should be provided.
- Hand Therapy: early physiotherapy to improve post-operative range of movement.
Please note: elevation may be combined with a closed irrigation catheter under the A1 pulley with a small drain sutured to the distal incision. The results of a randomized control trial assessing the utility of this are awaited (Göransson, 2015).
Complications of Flexor Tenosynovitis
Complications and post-operative function are related to severity at presentation, co-morbidity, and time from onset to surgical management, and should be discussed pre-operatively.
Flexor Tenosynovitis results in major soft tissue complications. Albeit, reports of outcomes are varied (Bolton, 2019). This can range from skin loss, fat necrosis to tendon adhesions, and collateral ligament contractures. These are detailed below:
- Skin Loss: Major soft tissue infection can result in volar skin loss. This may require delayed skin graft or flap reconstruction
- Range of Movement: Tendon damage, adhesions, and inflammation. Secondary Tenolysis may be required following intensive physiotherapy.
- Amputation: Purulence and ischaemia in addition to Kanavel’s signs is associated with a 59% amputation rate (Pang, 2007)
In severe cases, it can also result in deep abscesses, septic arthritis, and osteomyelitis (Canella, 2013).
Delayed presentation or management results in increased morbidity due to interruption of tendon gliding, tendon necrosis, and adhesion formation.
Conclusion
1. Anatomical Complexity: Understanding the detailed anatomy of the flexor sheath to recognize the pathways an infection can spread and complicate, underscoring the necessity for timely and precise interventions.
2. Clinical Presentations: Identifying the four Kanavel’s signs pathognomonic of PFT, thereby facilitating early diagnosis and management to prevent severe outcomes.
3. Management Strategies: Recognizing PFT as a surgical emergency that necessitates hospital admission, initiation of IV antibiotics, and often surgical intervention to prevent irreversible damage to the flexor tendons.
4. Treatment Modalities: Familiarity with surgical approaches from closed to open washouts, and recognizing the scenarios where each is applicable based on the severity and progression of the infection.
5. Potential Complications: Knowing the potential complications such as stiffness, adhesions, and even amputation, and understanding how these are influenced by the severity at presentation, co-morbidities, and timeliness of surgical intervention.
Further Reading
- Flexor Sheath Infection. The British Society for Surgery of the Hand. Accessed 23/4/2024.
- SCHELDRUP EW. Tendon sheath patterns in the hand; an anatomical study based on 367 hand dissections. Surg Gynecol Obstet. 1951 Jul;93(1):16-22. PMID: 14855245.
- Bolton LE, Bainbridge C. Current opinions regarding the management of pyogenic flexor tenosynovitis: a survey of Pulvertaft Hand Trauma Symposium attendees. Infection. 2019 Apr;47(2):225-231. doi: 10.1007/s15010-018-1236-z. Epub 2018 Nov 1. PMID: 30387044.
- Pang HN, Teoh LC, Yam AK, Lee JY, Puhaindran ME, Tan AB. Factors affecting the prognosis of pyogenic flexor tenosynovitis. J Bone Joint Surg Am. 2007 Aug;89(8):1742-8. doi: 10.2106/JBJS.F.01356. PMID: 17671013.
- Clements JM, O'Neill T, Hill C. Challenging Kanavel's cardinal signs of pyogenic flexor tenosynovitis of the hand. J Plast Reconstr Aesthet Surg. 2019 Jul;72(7):1219-1243. doi: 10.1016/j.bjps.2019.02.011. Epub 2019 Mar 2. PMID: 30871940.
- Brusalis CM, Thibaudeau S, Carrigan RB, Lin IC, Chang B, Shah AS. Clinical Characteristics of Pyogenic Flexor Tenosynovitis in Pediatric Patients. J Hand Surg Am. 2017 May;42(5):388.e1-388.e5. doi: 10.1016/j.jhsa.2017.02.007. Epub 2017 Mar 22. PMID: 28341068.
- Rico AA, Holguín PH, González IG, Coba JM. Flexor tendon synovial sheath haemangioma mimicking subacute tenosynovitis. J Hand Surg Br. 1994 Dec;19(6):704-5. doi: 10.1016/0266-7681(94)90239-9. PMID: 7706868.
- Leden I, Jonsson G, Larsen S, Rank F, Scherstén B, Svensson B, Thorngren KG. Flexor tenosynovitis (FTS): a risk indicator of abnormal glucose tolerance. Scand J Rheumatol. 1985;14(3):293-7. doi: 10.3109/03009748509100409. PMID: 4048877.
- Leppänen OV, Jokihaara J, Kaivorinne A, Havulinna J, Göransson H. Protocol for an investigator-blinded, randomized, 3-month, parallel-group study to compare the efficacy of intraoperative tendon sheath irrigation only with both intraoperative and postoperative irrigation in the treatment of purulent flexor tenosynovitis. BMJ Open. 2015 Dec 15;5(12):e008824. doi: 10.1136/bmjopen-2015-008824. PMID: 26671952; PMCID: PMC4679920.
- Michon J. Le phlegmon des gaines [Phlegmon of the tendon sheaths]. Ann Chir. 1974 Apr;28(4):277-80. French. PMID: 4839194.
- Kanavel A: Infections of the hand, 7th ed. Philadelphia, Lea & Febiger, 1939.
- Grinnell RS. ACUTE SUPPURATIVE TENOSYNOVITIS OF THE FLEXOR TENDON SHEATHS OF THE HAND: A REVIEW OF ONE HUNDRED AND TWENTY-FIVE CASES. Ann Surg. 1937 Jan;105(1):97-119. doi: 10.1097/00000658-193701000-00010. PMID: 17856913; PMCID: PMC1390296.
- Sharma KS, Rao K, Hobson MI. Space of Parona infections: experience in management and outcomes in a regional hand centre. J Plast Reconstr Aesthet Surg. 2013 Jul;66(7):968-72. doi: 10.1016/j.bjps.2013.03.020. Epub 2013 Apr 6. PMID: 23571016.
- Stevanovic, M. V., and F. Sharpe. "Acute infections in the hand." Green’s operative hand surgery 1 (2005): 77-81.
- Canella C, Pacheco M, Costa F, Marchiori E. Infectious tenosynovitis in a patient with dermatopolymyositis and vasculitis. J Rheumatol. 2013 Jun;40(6):949. doi: 10.3899/jrheum.121434. PMID: 23728188.


