Summary Card
Definition of Basal Thumb Osteoarthritis
The destruction of hyaline articular cartilage. It refers carpometacarpal joint (CMCJ) and STT joint
Anatomy of the Thumb
Thumb base osteoarthritis management hinges on the unique saddle joint's stability, provided by crucial ligaments like the volar beak and posterior oblique, and its articulation with adjacent bones.
Pathophysiology of Basal Thumb Arthritis
Osteoarthritis results in cartilage loss, bone changes, and ligament instability, causing joint narrowing, deformities, and finger nodules.
Clinical Picture of Basal Thumb Osteoarthritis
Diagnosis of basal thumb OA involves pinpointing grip pain and differentiating it from other wrist conditions via history and physical exams.
Classification of Basal Thumb Osteoarthritis
The Eaton and Glickel classification for thumb osteoarthritis spans from normal to severe, involving the scaphotrapezial joint, but may not correlate with pain or function.
Management of Basal Thumb Arthritis
Thumb osteoarthritis treatment ranges from pharmacotherapy and splinting to surgical options like trapeziectomy and arthroplasty for pain relief and functional improvement.
Author: Dr Suzanne Thompson
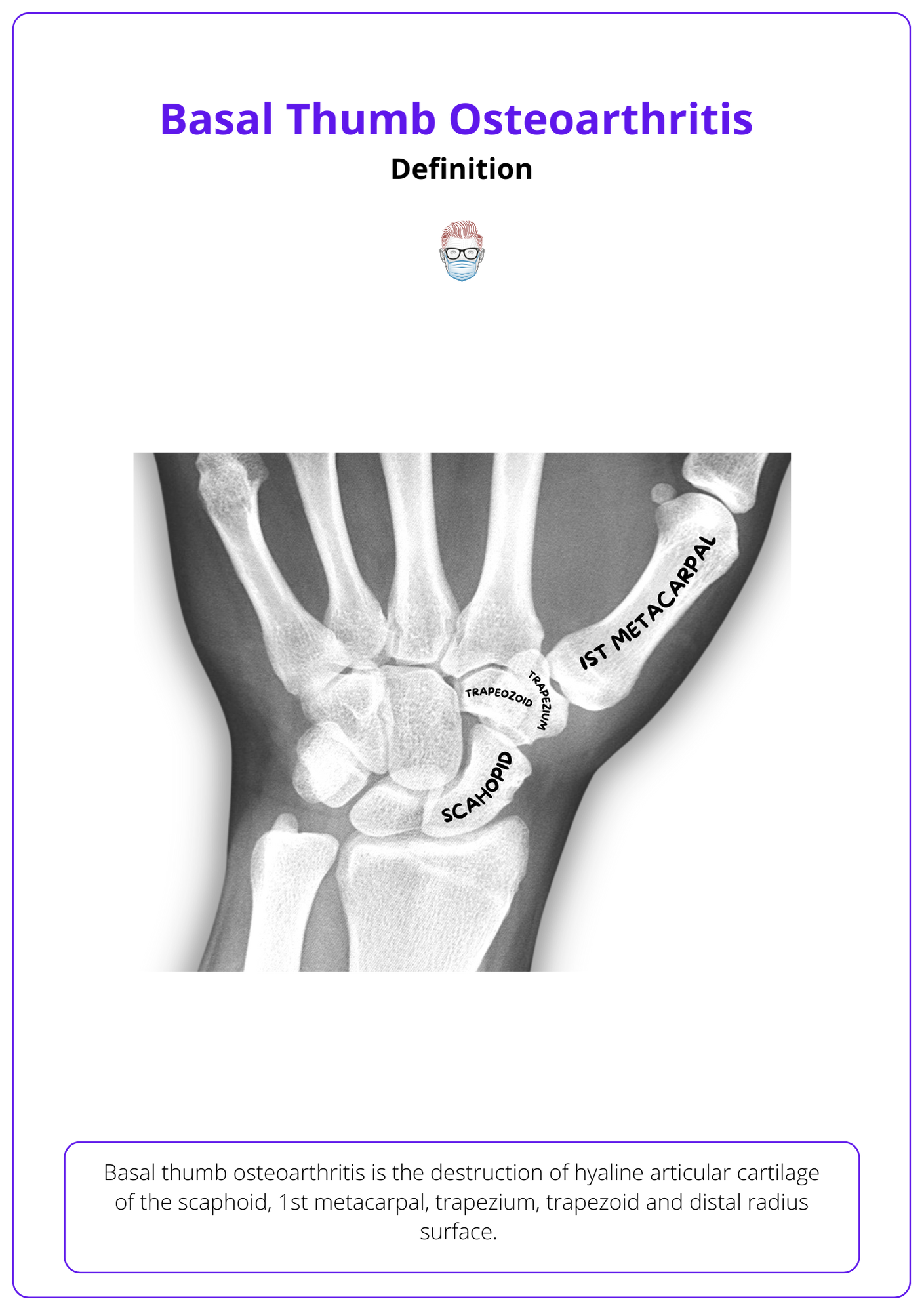
Definition of Basal Thumb Osteoarthritis
Basal thumb osteoarthritis is the destruction of hyaline articular cartilage. It refers carpometacarpal joint (CMCJ) and STT joint. This includes the scaphoid, 1st metacarpal, trapezium, trapezoid. It can be subclassified into:
- Primary: ligament laxity and attenuation over time
- Secondary from previous trauma/injury.
Anatomy of the Thumb
The base of the thumb features a unique saddle joint stabilized by key ligaments, notably the volar beak and posterior oblique, with its articulation with surrounding bones crucial for managing osteoarthritis
The base of the thumb features a complex anatomical structure crucial for its function and involvement in osteoarthritis (OA) development:
- Joint: A biconcave trapezeiometacarpal saddle joint, allowing versatile movement.
- Ligament: Stabilized by over 16 ligaments, with the volar beak ligament and posterior oblique ligaments being paramount in OA progression.
- Articulations: The trapezium bone connects with the trapezoid and scaphoid bones.
Pathophysiology of Basal Thumb Arthritis
Osteoarthritis leads to joint degeneration, characterized by cartilage degradation, bone changes, and ligament instability, which results in reduced joint space, bone deformities, and characteristic finger nodes.
Osteoarthritis manifests through a cascade of joint alterations, including matrix breakdown, cartilage wear, and bone changes, leading to distinctive symptoms and structural deformities. The progression entails:
- Initial Changes: Matrix destruction, cartilage issues (dehydration, erosion), and bony alterations (cysts, osteoporosis, sclerosis).
- TM Joint Impact: Eburnation in the TM joint prompts ligament instability, notably in the beak ligament, shrinking joint space evident in radiographs.
- Advanced Symptoms: Progression is marked by bone density shifts, growth of osteophytes, deformities, and specific nodes (Heberden’s and Bouchard's) at finger joints, occasionally with cysts.
- Ligament Effects: Compromised posterior oblique and volar beak ligaments cause the metacarpal to shift, leading to notable joint deformities such as subluxation.
Clinical Picture of Basal Thumb Osteoarthritis
Diagnosis of thumb osteoarthritis hinges on identifying grip pain, assessing joint tenderness. It is important to differentiate it from other radial-sided wrist pain aetiology.
In evaluating thumb osteoarthritis, it's crucial to discern its typical symptoms, such as pain during grip movements, from those of other hand conditions through careful examination and consideration of the patient's history.
Symptoms
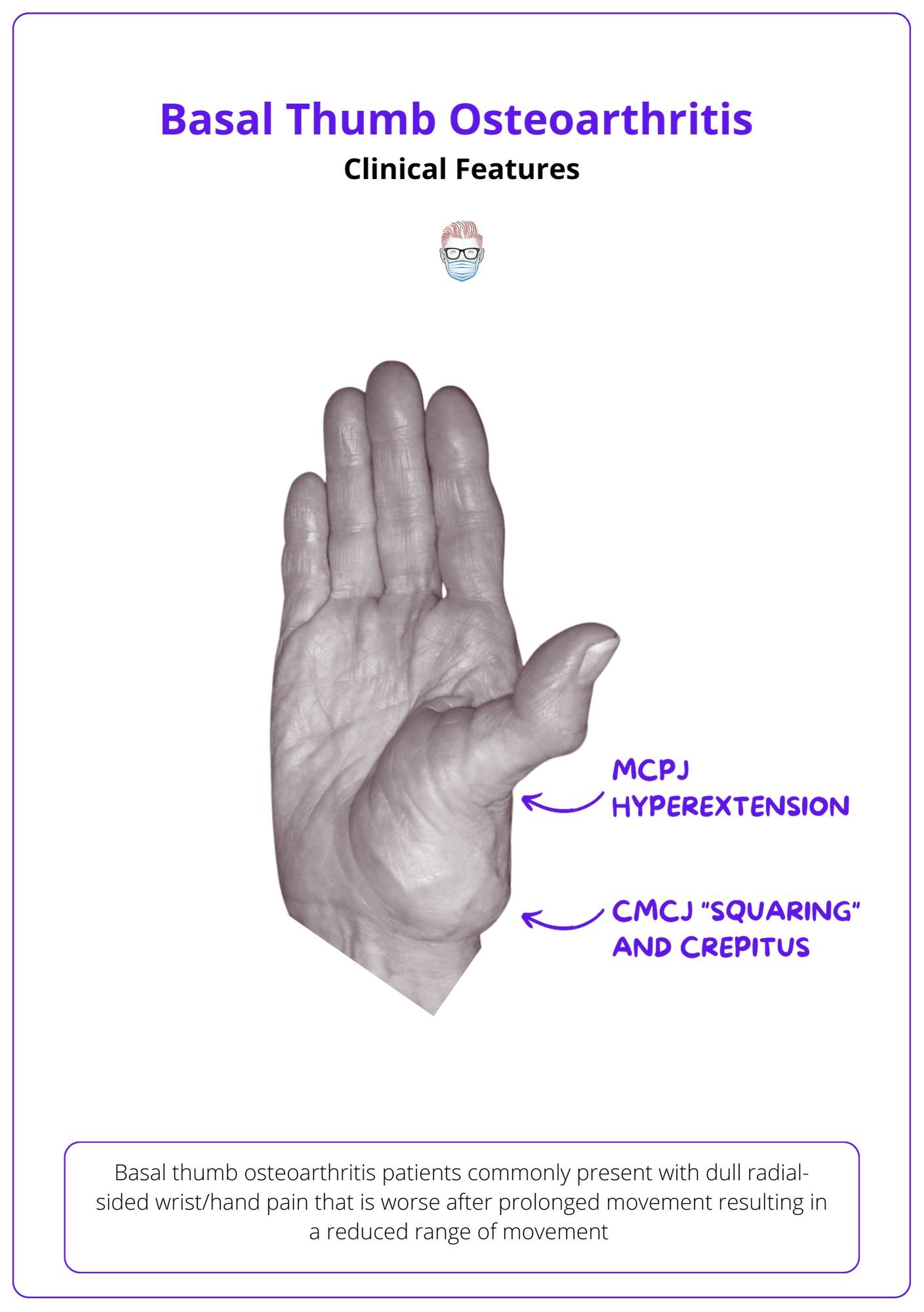
Basal thumb osteoarthritis patients commonly present with the following symptoms.
- Dull radial-sided wrist/hand pain exacerbated by prolonged movement
- Temporary morning stiffness
- Reduced range of movement
Important questions to ask in the history:
- Symptoms: where, when and exacerbating factors
- Function: impact on ADLs, ROM
- Expectations
Signs
On examination, key clinical findings include:
Look:
- CMCJ adducted and subluxed to create a "square appearance" (severe cases)
- MCPJ Compensatoryhyperextension
- IPJs has Heberden's (DIPJ) or Bouchard (PIPJ) nodes.
Feel:
- Tenderness at anatomical snuffbox.
Move:
- Crepitus and pain on movement of CMCJ
- CMCJ subluxation when force applied
- Grind test +: pain on axial load and rotation of the thumb metacarpal.
- Weak lateral pinch, pincer grip and key pinch.
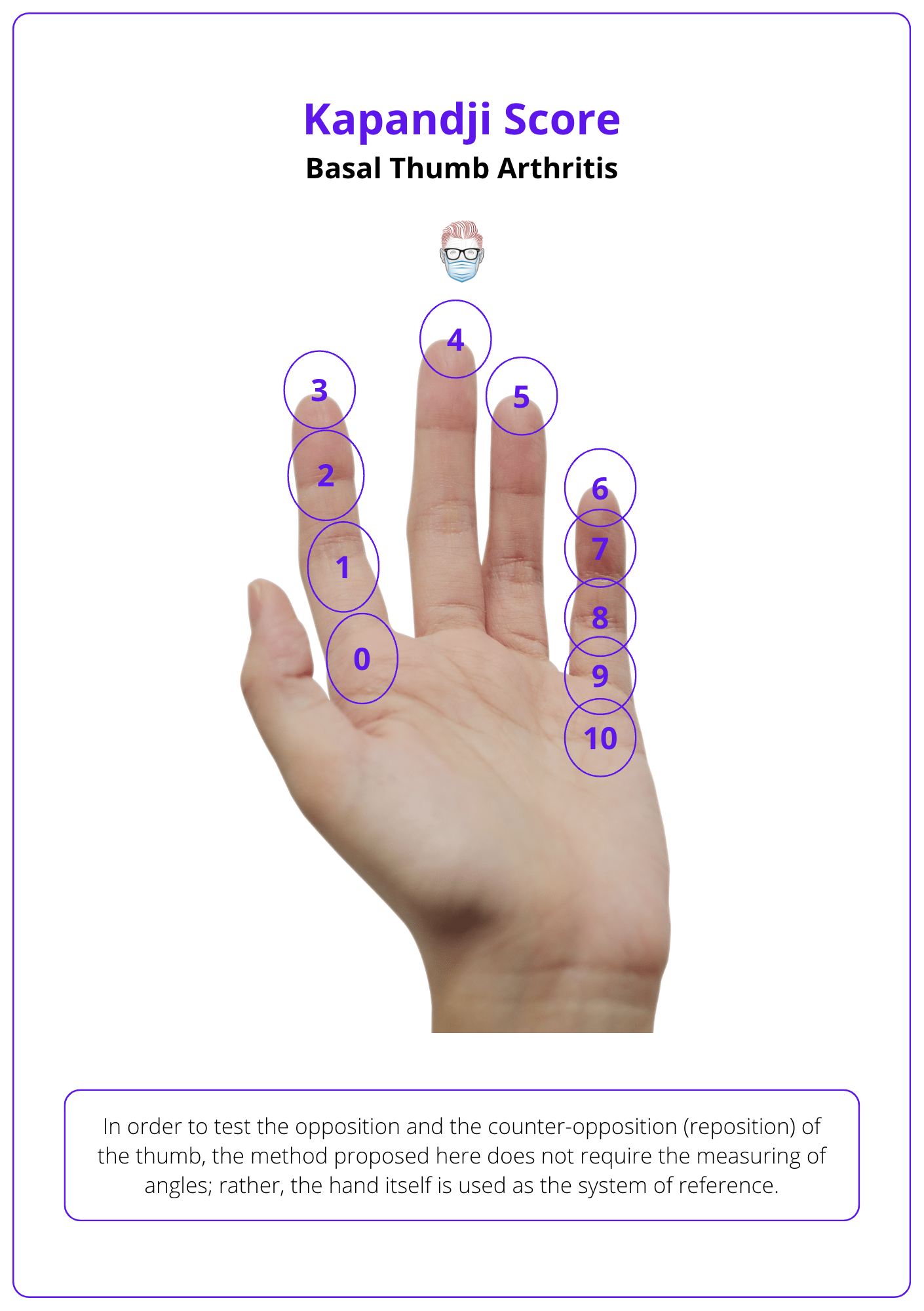
The Kapandji score (1986), a prevalent tool for thumb opposition, offers an alternative to angular measurements. This method uses the hand as its reference, eliminating the need for angle measurements. The scoring system is visualised below.
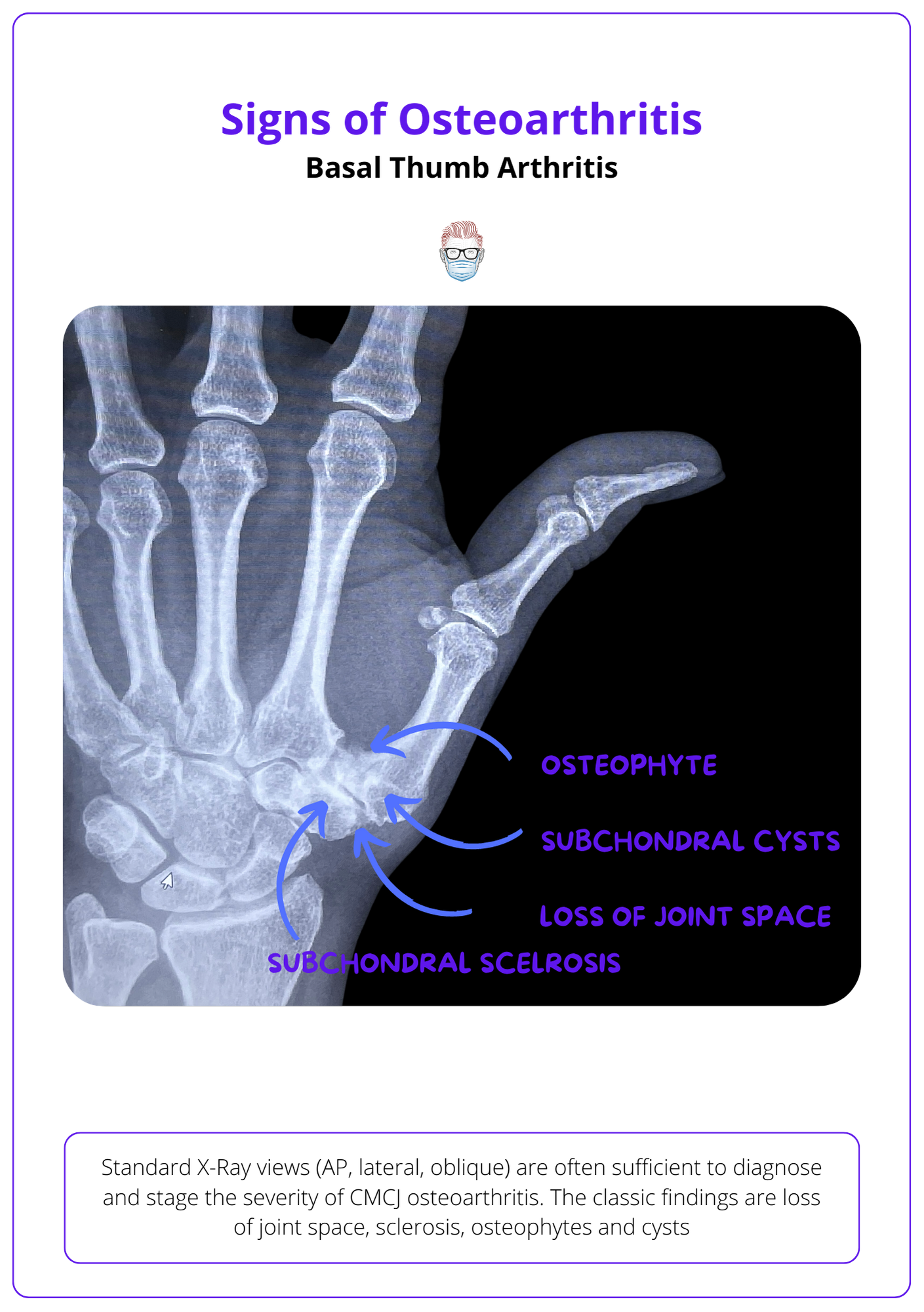
XRay Classification of Basal Thumb Osteoarthritis
The Eaton and Glickel classification of thumb osteoarthritis ranges from normal to advanced scaphotrapezial joint involvement, not always reflecting pain or functional loss.
Standard X-Ray views (AP, lateral, oblique) are often sufficient to diagnose and stage the severity of CMCJ osteoarthritis. The classic findings are loss of joint space, sclerosis, osteophytes and cysts. Some of these osteoarthritic findings at the CMCJ/basal thumb are illustrated below:
The Eaton classification describes the severity of radiological changes in basal thumb arthritis. Eaton and Littler described it in 1987:
- Stage I: The joint appears normal, though there may be slight widening due to synovitis.
- Stage II: Features joint space narrowing with the presence of debris and osteophytes smaller than 2mm.
- Stage III: Characterized by further joint space narrowing, debris, and larger osteophytes exceeding 2mm.
- Stage IV: Involves the scaphotrapezial joint, indicating advanced disease.
This can be visualised in the image below
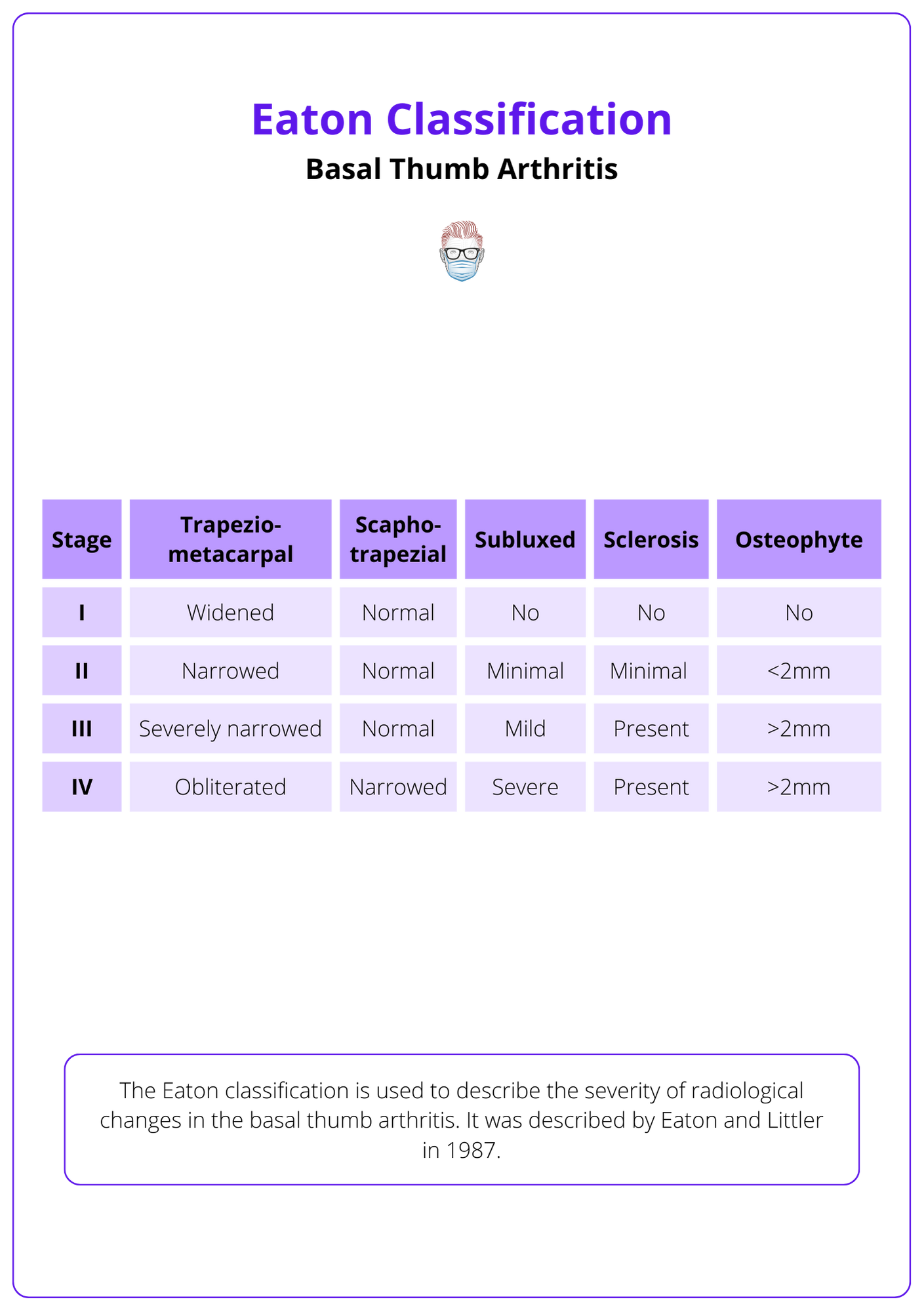
Tips to remember this classification include:
- If the trapezio-metacarpal joint is widened: stage is ≥1
- If the trapezio-metacarpal joint is narrowed: stage is ≥2
- If osteophytes are >2mm: stage is ≥ 3
- If scapho-trapezial joint is narrowed: stage is ≥ 4
MRI or CT are rare neccessary for operative procedures or surgical decision making. Other views quotes in the literature include:
- Gedda: superior but require accurate positioning of the thumb,
- Roberts: beam centered on trapezium and metacarpal with thumb flat and hyperpronated. This is considered a true PA view of the joint
- Stress views demonstrate joint laxity but cannot differentiate between painless constitutional laxity and painful pathologic laxity.
Management of Basal Thumb Arthritis
Management of thumb osteoarthritis encompasses non-operative strategies, such as pharmacotherapy and splinting, and surgical interventions like trapeziectomy and arthroplasty, aimed at pain relief and functional restoration in affected patients.
The management of basal thumb arthritis integrates a spectrum of strategies aimed at alleviating pain and restoring function for those affected. The approaches include non-operative and surgical treatments as discussed below.
Treatment includes:
- Lifestyle modifications and education
- Therapy: Splinting and exercises, ideally mobilising the IPJ.
- Analgesia: Topical and oral remedies, with intermittent pain challenges
- Surveillance: Monitoring hand function
- Injections: Steroid injections with potential imaging guidance (X-Ray or USS)
- Reassurance: Surgery is viable even at late disease stages.
The following video shows a technique for CMCJ steroid injection.
CMCJ Steroid Injection
In addressing thumb osteoarthritis surgically, the goal is to mitigate pain, restore function, and halt joint deterioration. The choice of technique is pivotal, tailored to the individual's disease stage and overall health profile.
Surgical Techniques
Surgical management ranges from minimally invasive procedures to more comprehensive reconstructive techniques, each with specific indications and outcomes.
Surgical correction of basal thumb arthritis focuses on two anatomical points - bone & soft tissue. This is listed below:
- Bone: trapeziectomy, arthroplasty, arthrodesis, osteotomy, implant.
- Soft Tissue: ligament reconstruction, tendon interposition, nerve denervation
Trapeziectomy:
An excisional arthroplasty has often been considered the 'gold standard' for treating basal thumb arthritis. It is the most commonly performed procedure for osteoarthritis in the upper limb. Since Gervis' intital description in 1948, variations have been published.
This procedure, pivotal in the surgical treatment of thumb osteoarthritis, involves the removal of the trapezium bone. It can be performed as:
- En bloc: Removing the trapezium in one piece.
- Piecemal: Taking out the trapezium in smaller sections.
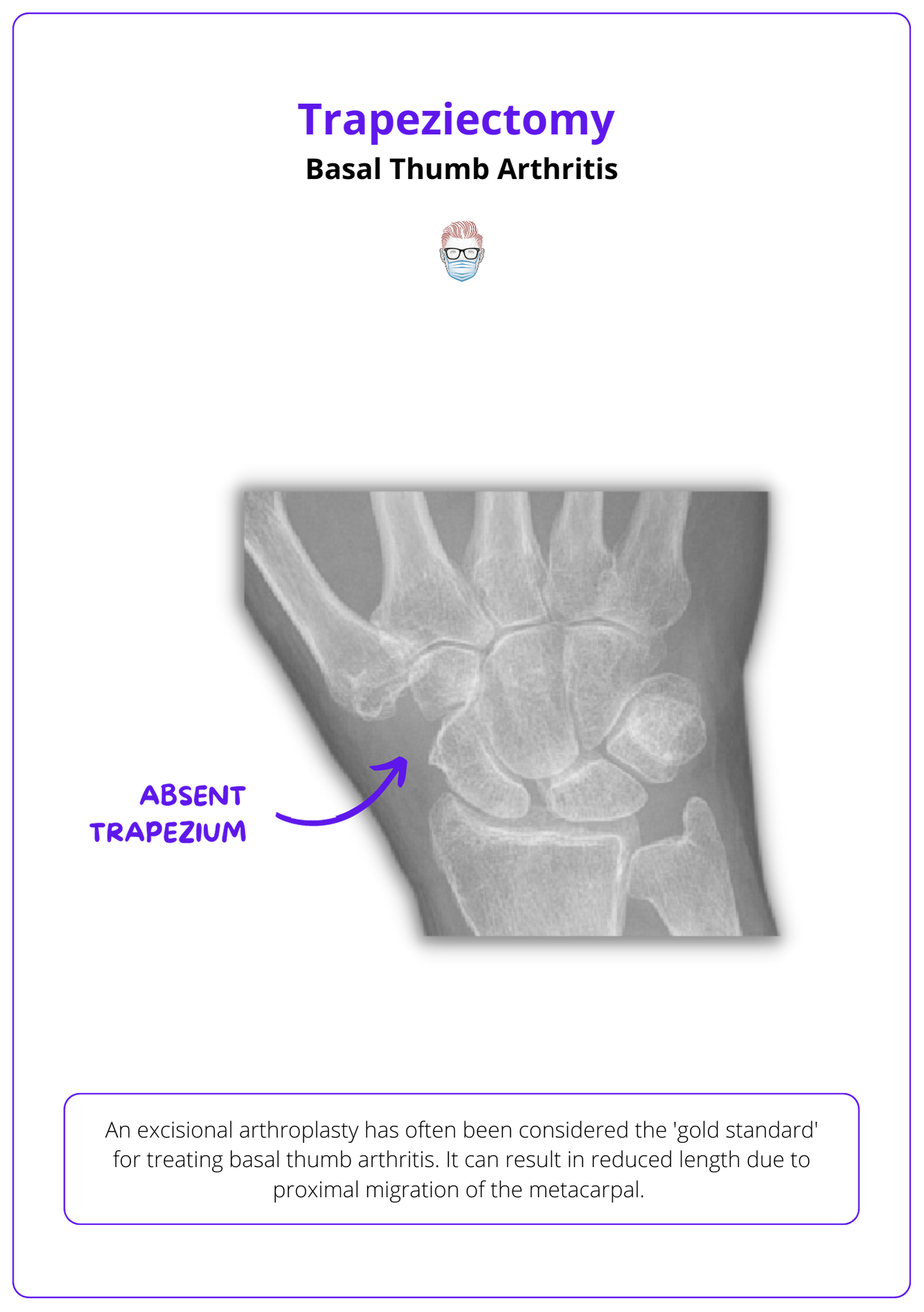
Following trapeziectomy, suspension techniques are often employed to prevent the thumb metacarpal from shifting. These include a tendon interposition with:
- Abductor pollicis longus (APL)
- Flexor carpi radialis (FCR) tendon following methodologies by Burton, Pelligrini, or Tomaino.
- The palmaris longus tendon, as described by Brunelli and Iwasaki, serves as an alternative for ligament reconstruction.
- Optionally reinforced with k-wires.
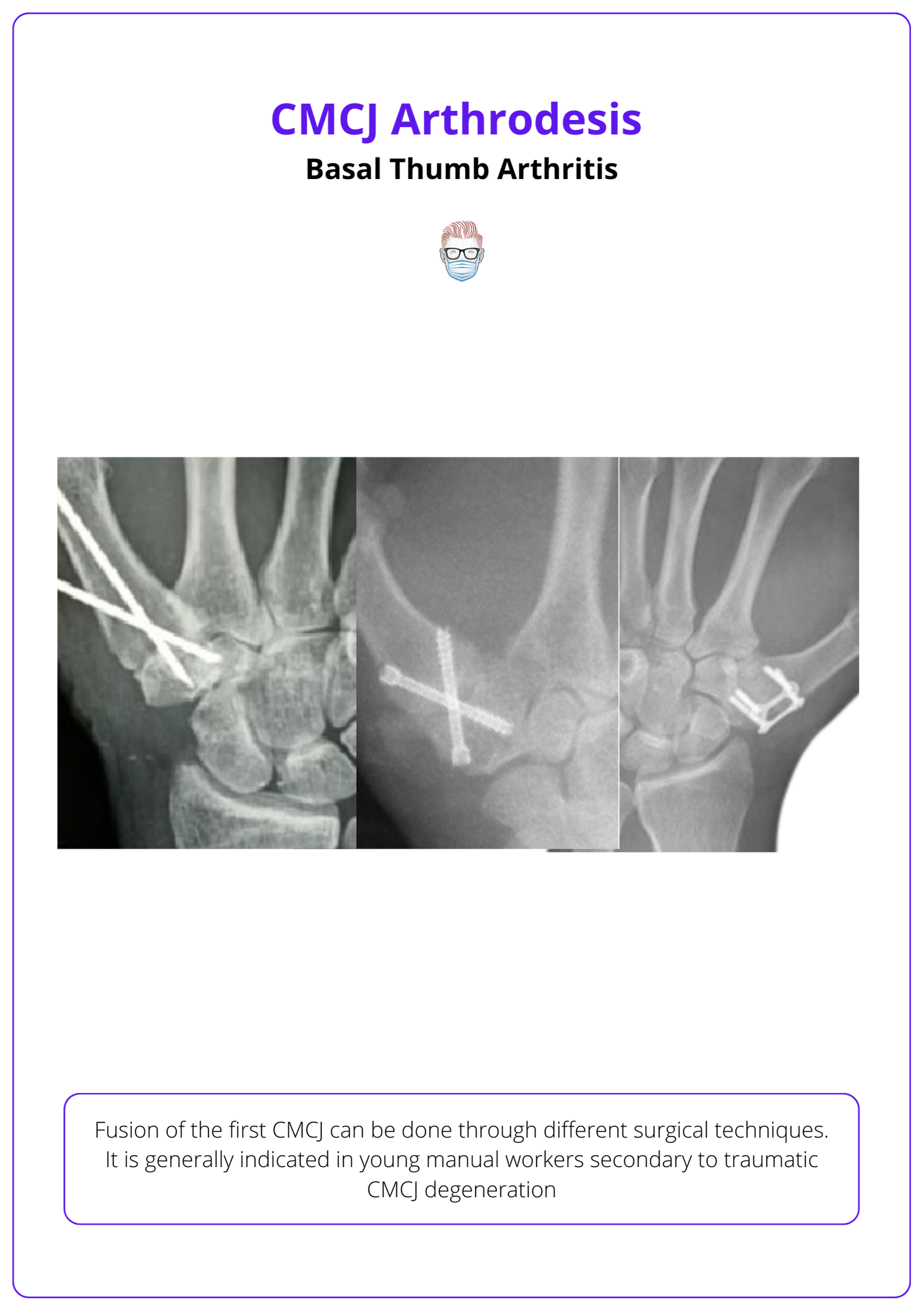
Arthrodesis
This is a fusion of the CMCJ (the trapeziometacarpal joint) into a functional plane to provide pain relief, stability and length preservation. This can be a potential option:
- young manual labourers
- secondary osteoarthritis from trauma
- patient prefers strength over mobility
- isolated TMC OA
This should be considered a less suitable option if scaphotrapezial joint involvement as fusion of the CMCJ will increase the force on the scaphoid.
CMCJ Denervation
Joint denervation offers a surgical option to alleviate pain in thumb osteoarthritis, focusing on the carpometacarpal (CMC) joint. While this procedure can significantly reduce pain, it does not prevent the progression of joint deformity. The CMC joint's complex innervation involves several nerves, necessitating a precise approach for effective denervation.
Nerve Supply:
- Dorsally: the posterior interosseous nerve and terminal branches of the superior radial nerve.
- Volarly: the lateral antebrachial cutaneous nerve and the palmar branch of the median nerve.
Surgical Approaches:
- A single incision volar approach, such as the Wagner incision, is traditionally used but associated with higher re-operation rates due to persistent pain.
- Some surgeons opt for a two-incision approach to address this issue more comprehensively.
An anatomical study has pointed out the potential role of the median motor branch (post-innervation to the opponens muscle) contributing to the trapezium. Failure to divide this branch may result in ongoing pain post-denervation.
Osteotomy
An abduction-extension osteotomy can be used to change the pressure angle of the first metacarpal to the palmar surface of the CMCJ.
This can be considered in patients with minimal osteoarthritis at the CMCJ but not considered if hypermobility or fixed subluxation of the CMC joint.
Conclusion
1. Anatomy of the Thumb Base: Acquired a thorough understanding of the thumb base's anatomical structure, focusing on its unique saddle joint and essential ligaments like the volar beak and posterior oblique. This knowledge is vital for the effective management of osteoarthritis.
2. Pathophysiology of Basal Thumb Arthritis: Enhanced your insight into the degenerative processes leading to basal thumb arthritis, including cartilage wear, bone changes, and the critical role of ligament instability in disease progression.
3. Clinical Diagnosis and Differentiation: Enhanced your ability to diagnose basal thumb osteoarthritis by distinguishing its symptoms from other radial-sided wrist pain causes, utilizing patient history and specific examination techniques.
4. Classification and Staging of Thumb OA: Learned about the Eaton and Glickel classification system for thumb OA, understanding its stages from normal to advanced disease, and recognizing the discrepancy that may occur between radiographic findings and patient-reported symptoms.
5. Management Strategies for Basal Thumb Arthritis: Gained insights into the comprehensive management approaches for thumb OA, from non-operative treatments aimed at pain relief and functional support to various surgical interventions designed to restore function and halt disease progression, including the detailed considerations for selecting appropriate surgical techniques based on individual patient needs.
Further Reading
- Myohanen M, Waris E, Nordback PH, Mattila S, Aspinen S. Substantial Increase in the Incidence of Surgery for Osteoarthritis of the Base of the Thumb Between 1997 and 2019 in Finland. In Vivo. 2022 Mar-Apr;36(2):833-838. doi: 10.21873/invivo.12770. PMID: 35241539; PMCID: PMC8931894.
- Eaton RG, Glickel SZ. Trapeziometacarpal osteoarthritis. Staging as a rationale for treatment. Hand Clin. 1987 Nov;3(4):455-71. PMID: 3693416.
- Tsujii M, Iida R, Oshima Y, Odake K, Satonaka H, Kokubu N, Sudo A. Arthroscopic ligamentoplasty for osteoarthritis of the thumb carpometacarpal joints: Clinical and radiological outcomes with a minimum 2-year follow-up. J Orthop Sci. 2020 Mar;25(2):241-246. doi: 10.1016/j.jos.2019.03.012. Epub 2019 Apr 6. PMID: 30962096.
- Kawamura D, Funakoshi T, Iwasaki N. Trapeziectomy with Ligament Reconstruction and Interposition Arthroplasty Using the Palmaris Longus Tendon: An Average 5-Year Follow-up. Clin Orthop Surg. 2019 Dec;11(4):453-458. doi: 10.4055/cios.2019.11.4.453. Epub 2019 Nov 12. PMID: 31788169; PMCID: PMC6867923.
- Burton RI, Pellegrini VD Jr. Surgical management of basal joint arthritis of the thumb. Part II. Ligament reconstruction with tendon interposition arthroplasty. J Hand Surg Am. 1986 May;11(3):324-32. doi: 10.1016/s0363-5023(86)80137-x. PMID: 3711604.
- Tomaino MM, Pellegrini VD Jr, Burton RI. Arthroplasty of the basal joint of the thumb. Long-term follow-up after ligament reconstruction with tendon interposition. J Bone Joint Surg Am. 1995 Mar;77(3):346-55. doi: 10.2106/00004623-199503000-00003. PMID: 7890782.
- van der Meulen C, van de Stadt LA, Claassen A, Kroon FPB, Ritt MJPF, Rosendaal FR, Terpstra SES, Vochteloo AJH, Kloppenburg M. Surgical denervation as a treatment strategy for pain in hand osteoarthritis: a systematic literature review. RMD Open. 2023 Aug;9(3):e003134. doi: 10.1136/rmdopen-2023-003134. PMID: 37532467; PMCID: PMC10401234.
- Weber AE, Bolia IK, Trasolini NA. Biological strategies for osteoarthritis: from early diagnosis to treatment. Int Orthop. 2021 Feb;45(2):335-344. doi: 10.1007/s00264-020-04838-w. Epub 2020 Oct 19. PMID: 33078204.


