Summary Card
Wound Healing
Wound healing occurs in four distinct phases: Hemostasis (Day 1-3), Inflammation (Day 3-7), Proliferation (Day 3-21), and Maturation (Week 3 to 1 year).
Classification of Wound Dressings
Wound dressings can be categorized into non-occlusive, semi-occlusive, and occlusive dressings, depending on their permeability and function.
Non-Occlusive & Semi-Occlusive Dressings
Non-occlusive dressings, like gauze and tulle, cover wounds without sealing them, while semi-occlusive dressings, such as Tegaderm, trap exudate while allowing air and moisture vapor to pass through.
Occlusive Dressings
Occlusive dressings keep wounds moist and shield them from trauma. Types include hydrogels, hydrocolloids (e.g., Duoderm), foams, and alginates.
Antimicrobial Dressings
Antimicrobial dressings, found across various dressing categories, are impregnated with agents like silver, bismuth, and chlorhexidine to help prevent infection.
Choice of Wound Dressing
Ideal wound dressing selection depends on local factors (e.g., exudate, tissue condition) and patient factors (e.g., allergies, compliance), which may change as conditions evolve.
Other Adjuncts to Wound Healing
Wound healing adjuncts include biophysical therapies (e.g., NPWT, electrical stimulation) and biological products (e.g., hyperbaric oxygen, growth factors, and stem cells) to speed and enhance healing.
Primary Contributor: Dr Waruguru Wanjau, Educational Fellow.
Reviewer: Dr Suzanne Thomson, Educational Fellow.
Wound Healing
Wound healing occurs in four distinct phases: Hemostasis (Day 1-3), Inflammation (Day 3-7), Proliferation (Day 3-21), and Maturation (Week 3 to 1 year).
The wound healing process is sequential and highly organized, involving four distinct phases, each with specific cellular and molecular activities.
Hemostasis (Day 1-3)
The first stage focuses on controlling bleeding and laying the groundwork for cellular migration.
- Vasoconstriction: Reduces blood flow to minimize bleeding.
- Coagulation: Platelets degranulate, releasing thromboxane A2 to initiate clot formation.
- Growth Factors: Platelet-derived growth factor (PDGF) acts as a chemotactic signal for fibroblasts and macrophages.
- Thrombus Formation: Stabilizes the wound and forms a provisional matrix.
Inflammation (Day 3-7)
The inflammatory phase initiates the body's defense and cleanup response, recruiting immune cells to the wound.
- Vasodilation & Increased Permeability: Enables white blood cell (WBC) migration into the wound area.
- Cellular Response:
- Neutrophils: Arrive within 24 hours as initial responders.
- Macrophages: Become predominant by days 2-3, releasing cytokines and growth factors (e.g., PDGF, TGF-β1) to attract fibroblasts and support healing.
Proliferation (Day 3-21)
During the proliferative phase, cells focus on forming new tissue, restoring blood supply, and strengthening the wound.
- Fibroblasts: Convert into myofibroblasts by days 3-5, facilitating wound contraction and ECM formation.
- Extracellular Matrix (ECM): Composed of proteoglycans, fibronectin, and type III collagen.
- Collagen Synthesis: High rates of type III and type I collagen production provide initial tensile strength from days 4-5.
- Keratinocyte Migration: Re-epithelializes the wound surface.
- Neovascularization: Driven by vascular endothelial growth factor (VEGF), providing a blood supply for new tissue.
Maturation/Remodeling (Week 3 to 1 Year)
This final phase focuses on collagen reorganization, strength restoration, and long-term remodeling.
- Collagen Remodeling: Collagen replaces proteoglycans and fibronectin, with type I collagen forming cross-links for strength.
- Matrix Metalloproteinases (MMPs) and Tissue Inhibitors of Metalloproteinases (TIMPs) regulate this remodeling process, ultimately achieving a type I collagen ratio of 4:1.
- Epithelialization: Re-establishes the skin barrier from the basal layer to the stratum corneum.
- Contraction: Occurs in full-thickness wounds as fibroblasts transform into myofibroblasts, peaking between days 10-21.
A wound reaches 5% tensile strength at 1 week, 20% at 3 weeks, 50% at 4 weeks, and 80% by 6 weeks to 1 year, maxing at 80% of uninjured skin strength (Brown, 2023).
Classification of Wound Dressings
Wound dressings can be categorized into non-occlusive, semi-occlusive, and occlusive dressings, depending on their permeability and function.
Wound dressings are categorized by permeability—non-occlusive, semi-occlusive, and occlusive—each designed to create an environment that best supports wound healing (Shi, 2020).
- Non-Occlusive Dressings (e.g., gauze, cotton pads): Traditional dressings that cover and protect but lack moisture retention, potentially delaying healing and risking trauma if adhered.
- Semi-Occlusive Dressings: Impermeable to fluids but permit gas exchange, balancing moisture to reduce drying and prevent fluid buildup.
- Occlusive Dressings: Fully seal the wound, retaining moisture, supporting autolysis, and protecting new tissue. These dressings stabilize temperature and humidity, promoting faster healing by encouraging cell growth and migration.
Traditional vs. Modern Dressings
Modern wound dressings address the limitations of traditional options, offering enhanced wound stability and reduced risk of reinjury, particularly beneficial in complex or slow-healing wounds.
- Traditional Dressings (Inert): Gauze, cotton pads, and bandages offer basic protection but lack moisture retention, risking wound adherence and disruption of healing tissue.
- Modern Dressings: Designed to maintain a moist environment, modern dressings support faster healing by promoting autolysis and reducing necrotic tissue. They provide a stable temperature and humidity, prevent trauma to new granulation tissue, and encourage cell proliferation and epithelial migration.
The amount of secondary contraction depends on the dermal content of the wound — more dermis results in less contraction (Brown, 2023).
Non-Occlusive and Semi-Occlusive Dressings
Non-occlusive dressings, such as gauze and tulle, cover wounds without sealing them, while semi-occlusive dressings, like Tegaderm, retain moisture by trapping exudate while allowing air and moisture vapor to pass through.
In wound care, dressing choice is guided by the need to balance protection, moisture retention, and infection prevention. Non-occlusive and semi-occlusive dressings each offer unique benefits depending on the wound's requirements for healing.
Non-Occlusive Dressings
Passive dressings primarily used for wound coverage and protection.
- Examples: Gauze, tulle.
- Function: Provide basic wound coverage without maintaining a moist environment, which can delay healing.
Semi-Occlusive Dressings
Designed to maintain moisture by trapping exudate while permitting air and moisture vapor exchange, supporting optimal wound healing.
- Examples: Biofilm, Bioclusive, Hydrofilm, Mepilex Film, OpSite, and OpSite Flexifix Gentle.
- Function: Impermeable to bacteria and fluids, these dressings create a moist, protective barrier while allowing gas exchange to reduce the risk of infection.
Silver ions (Ag+) play a critical role in wound care by killing pathogens and disrupting biofilms. They work by binding to tissue proteins and bacterial cell walls, causing cell lysis and inhibiting bacterial DNA and RNA synthesis, which halts bacterial replication (May, 2022).
Occlusive Dressings
Occlusive dressings maintain a moist environment and protect wounds from trauma, aiding in faster healing. Types include hydrogels, hydrocolloids (e.g., Duoderm), foams, and alginates.
Occlusive dressings are crucial for wounds that benefit from a stable, moisture-rich environment. By maintaining moisture, these dressings accelerate healing, protect new tissue from trauma, and reduce the risk of infection.
How Occlusive Dressings Work
Occlusive dressings preserve moisture at the wound site, promoting faster healing and providing a protective barrier. Typically available in sheet form, these dressings can be cut to fit the wound. In some cases, a secondary dressing may be needed for complete sealing.
Benefits
- Accelerates Re-Epithelialization: Can increase healing rates by up to 40% in partial-thickness wounds (Mir, 2018).
- Promotes Healing Factors: Maintains exposure to proteinases, growth factors, and chemotactic agents.
- Encourages Collagen Synthesis and Angiogenesis: Creates a mildly hypoxic, low-pH environment that supports collagen formation and new blood vessel growth, reducing infection risk.
Contraindications
Occlusive dressings should be avoided in:
- Macerated Skin: Excess moisture can worsen skin damage.
- Infected Wounds: Traps bacteria, potentially worsening infection.
The table below summarises the types of occlusive dressings and their characteristics.
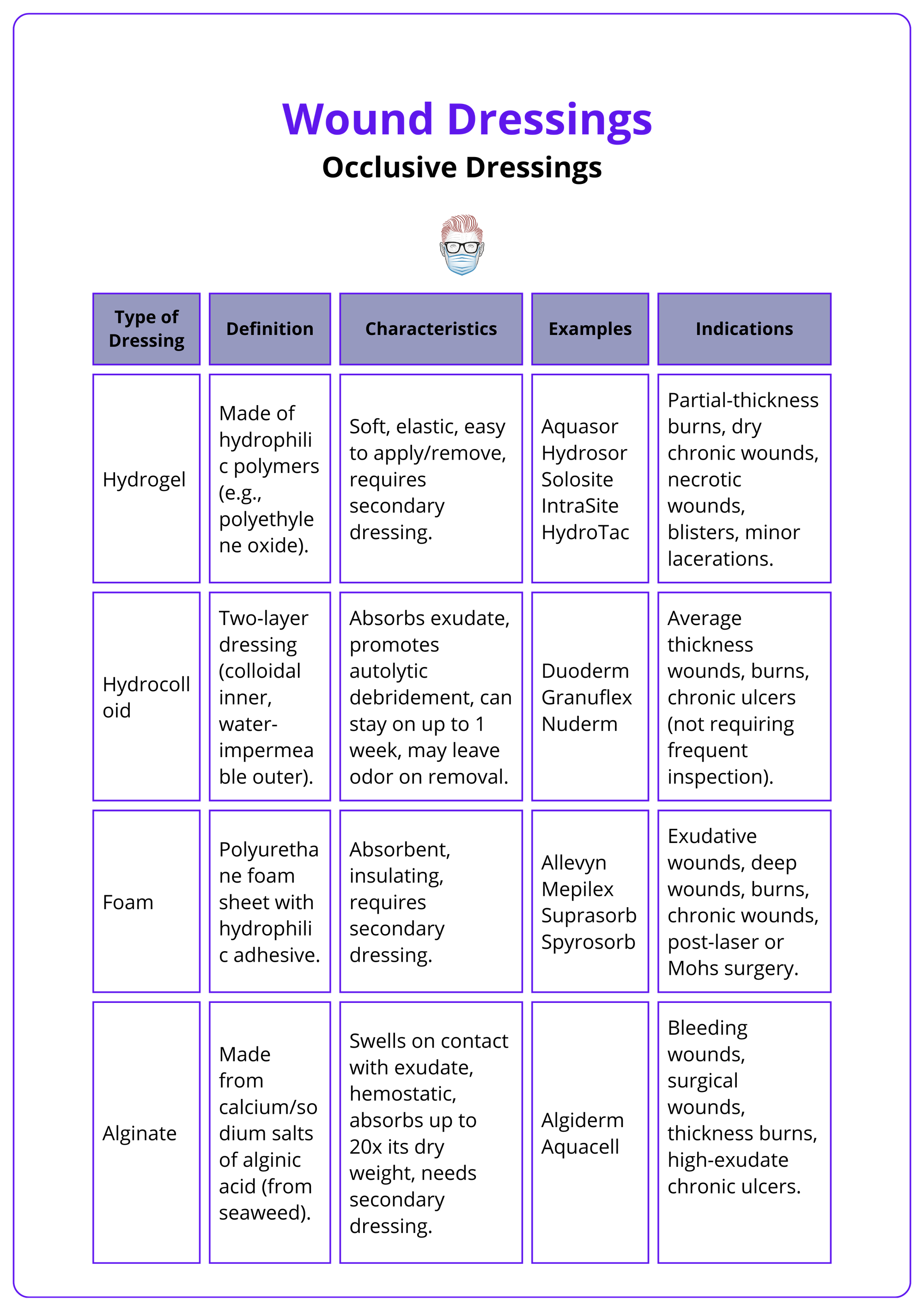
Contrary to past beliefs, occlusive dressings have been shown to lower infection rates by maintaining a moist environment (Tan, 2019).
Antimicrobial Dressings
Antimicrobial dressings are available across dressing categories and are impregnated with agents like silver, bismuth, and chlorhexidine to prevent infection.
Antimicrobial dressings exist in both occlusive and non-occlusive forms, categorized broadly as silver-impregnated and non-silver-impregnated dressings.
Silver-Impregnated Dressings
Silver-based dressings are favored for their broad-spectrum antimicrobial properties and can be either non-occlusive or occlusive.
- Non-Occlusive Silver Dressings: These can be sheets (Acticoat, Urgotu) or Bandages (Silverlon)
- Occlusive Silver Dressings can be Alginate Dressings (Aquacel Ag) or Foam Dressings (Mepilex Ag)
Non-Silver Antimicrobial Dressings
These dressings incorporate agents like bismuth, chlorhexidine, or honey to provide antimicrobial coverage without silver.
Non-Occlusive Non-Silver Dressings:
- Xeroform: Gauze with bismuth and petroleum.
- Bactigras: Gauze with paraffin and chlorhexidine.
- Inadine: Fabric with polyethylene glycol.
Occlusive Non-Silver Dressings:
- Honey-Based and Other Agents: Honey or other antimicrobial agents can be applied under an occlusive dressing to help prevent infection.
Acute wounds generally heal within 8–12 weeks with minimal scarring, while chronic wounds often take longer than 12 weeks and have a higher risk of recurrence (Tan, 2023).
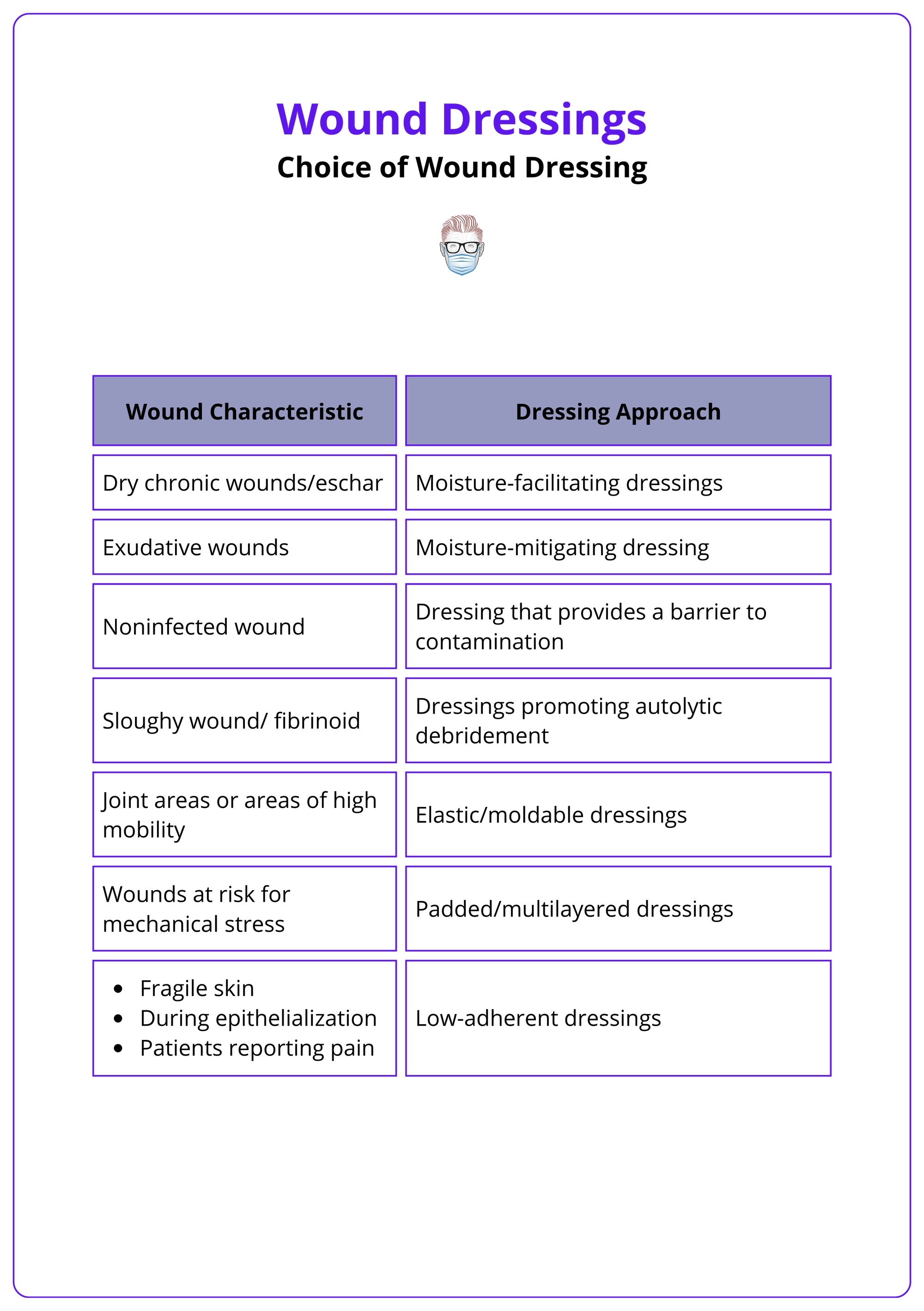
Choice of Wound Dressing
Selecting an ideal wound dressing requires consideration of local wound factors (e.g., exudate level, tissue health) and patient-specific factors (e.g., allergies, compliance). These needs may shift as healing progresses.
Factors to Consider in Dressing Selection
An ideal dressing should meet the following criteria (Degreef, 1998):
- Healing Support: Maintain a moist environment, enhance epidermal migration for faster regeneration, and promote angiogenesis and connective tissue synthesis.
- Trauma Prevention: Avoid disrupting new tissue during dressing changes and be non-adherent to prevent trauma on removal.
- Protection: Allow gas exchange, protect against bacterial infection, and maintain temperature to encourage blood flow.
- Safety: Be sterile, non-toxic, and non-allergenic to avoid adverse reactions.
Factors in Dressing Selection
As wound and patient conditions evolve, dressing adjustments may be necessary.
- Local Wound Factors: Dressing choice should match the wound’s exudate level, infection risk, and healing phase.
- Systemic Patient Factors: Consider the patient’s allergies, compliance with dressing changes, access to resources, and dressing change frequency needs.
The table below summarises dressing approaches for different wounds (Chung, 2024).
Other Adjuncts to Wound Healing
Wound healing adjuncts include biophysical therapies (e.g., NPWT, electrical stimulation) and biological products (e.g., hyperbaric oxygen, growth factors, and stem cells) to speed and enhance healing.
Multiple adjuncts to wound healing are available (Chung, 2024). These can be categorised as,
Biophysical Therapies
- Negative Pressure Wound Therapy (NPWT): Applies negative pressure to the wound bed, promoting granulation tissue formation.
- Transcutaneous Electrical Nerve Stimulation (TENS): Uses non-invasive electrical stimulation to promote healing, such as epithelialization, fibroblast migration, and angiogenesis.
- Extracorporeal Shock Wave Therapy (ESWT): Uses high-energy acoustic pulses to stimulate cell proliferation, angiogenesis, and cavitation of necrotic tissue.
- Photobiomodulation (PBM): Utilises light to stimulate angiogenesis, ECM deposition, and reduce inflammation, enhancing wound healing.
- Photodynamic Therapy (PDT): Combines a photosensitizer with external light to produce an antibacterial effect, particularly against biofilm.
- Electromagnetic Fields: Low-frequency pulsed electromagnetic fields support collagen deposition, angiogenesis, and the release of nitric oxide.
Biological Products
- Hyperbaric Oxygen Therapy (HBOT): Administers enriched oxygen in a pressurised environment, improving oxygenation and promoting healing.
- Growth Factors (GFs): GFs help stimulate cell growth and tissue repair, aiding wound healing.
- Platelet Rich Plasma (PRP): PRP contains high concentrations of platelets, growth factors, and cytokines that promote epithelial cell proliferation, angiogenesis, collagen deposition, and wound closure.
- Stem Cells: Stem cells from various sources release growth factors that promote healing. Their use remains experimental due to concerns about safety in humans.
- Exosomes: Exosomes are extracellular vesicles that mediate communication between cells, delivering a mixture of growth factors and cytokines. Exosome-based therapies mimic stem cell effects without the challenges of cell-based treatments.
The mechanism of NPWT is debated. Some suggest it doesn’t increase perfusion but raises tissue pressure, altering mechanical properties (Young's modulus), which may drive its regenerative effect (Kairinos, 2013).
Conclusion
1. Phases of Wound Healing: Hemostasis immediately post-injury promotes clot formation; the Inflammation phase follows with immune activation; the Proliferation phase rebuilds the wound with new tissue and collagen; Maturation strengthens and remodels the wound over time.
2. Wound Dressings: Dressings are categorized by their interaction with the wound: Non-occlusive dressings like gauze allow air exposure; semi-occlusive dressings like Tegaderm manage moisture; occlusive dressings maintain a moist environment to facilitate healing.
3. Antimicrobial Dressings: These dressings, including silver-impregnated varieties, are used to prevent infections by disrupting pathogens and promoting a conducive healing environment.
4. Adjuncts to Wound Healing: Incorporates biophysical therapies like Negative Pressure Wound Therapy (NPWT) and biological products like hyperbaric oxygen therapy, which enhance cellular repair and reduce healing time.
5. Importance of Moist Environment: Effective modern dressings maintain a moist wound environment, essential for faster healing by promoting autolysis and tissue regeneration.
6. Innovations in Wound Care: Advances include technologies and treatments that improve healing rates, minimize complications, and enhance patient outcomes for complex wounds.
Further Reading
- Shi C, Wang C, Liu H, Li Q, Li R, Zhang Y, Liu Y, Shao Y, Wang J. Selection of Appropriate Wound Dressing for Various Wounds. Front Bioeng Biotechnol. 2020 Mar 19;8:182. doi: 10.3389/fbioe.2020.00182. PMID: 32266224; PMCID: PMC7096556.
- Theplasticsfella Wound healing April 2022. Accessed on 12th October 2024
- Brown D. Michigan Manual of Plastic Surgery 3rd edition 2023 Oct page 3-4
- Guo S, Dipietro LA. Factors affecting wound healing. J Dent Res. 2010 Mar;89(3):219-29. doi: 10.1177/0022034509359125. Epub 2010 Feb 5. PMID: 20139336; PMCID: PMC2903966.
- Tan, S.T., Winarto, N., Dosan, R. and Aisyah, P.B., 2019. The benefits of occlusive dressings in wound healing. The Open Dermatology Journal, 13(1).
- Chung 2024 Grabb and Smith's Plastic Surgery: 9th Edition September 2024 page 8-13
- Kairinos N, Holmes WJM, Solomons M, Hudson DA, Kahn D. Does a zone of increased perfusion exist around negative-pressure dressings? Plast Reconstr Surg. 2013 Oct;132(4):978-987. doi: 10.1097/PRS.0b013e31829f4ad9. PMID: 23783056.
- Degreef HJ. How to heal a wound fast. Dermatol Clin. 1998 Apr;16(2):365-75. doi: 10.1016/s0733-8635(05)70019-x. PMID: 9589210.
- May A, Kopecki Z, Carney B, Cowin A. Antimicrobial silver dressings: a review of emerging issues for modern wound care. ANZ J Surg. 2022 Mar;92(3):379-384. doi: 10.1111/ans.17382. Epub 2021 Nov 21. PMID: 34806300.\
- Mir M, Ali MN, Barakullah A, Gulzar A, Arshad M, Fatima S, Asad M. Synthetic polymeric biomaterials for wound healing: a review. Prog Biomater. 2018 Mar;7(1):1-21. doi: 10.1007/s40204-018-0083-4. Epub 2018 Feb 14. PMID: 29446015; PMCID: PMC5823812.


