In this Article
1. VRAM is a Type III Mathes and Nahai Flap
2. The most common indication is for pelvic reconstruction
3. Dominant supply is from Deep Superior & Inferior Epigastric Arteries
4. Can be raised as muscle-only, myocutaneous, osseomyocutaneous (rare)
5. It obliterates dead space but results in a weakened abdominal wall.
Indications for a VRAM Flap
The VRAM flap is versatile to be used in breast, head & neck, and pelvic reconstruction3. Pelvic reconstruction is its primary use and indications are listed below:
- Post-pelvic exenteration
- Abdominoperineal resection
- Vaginal wall reconstruction
- Radiation-induced necrosis
Chest reconstruction uses the superior pedicle whilst pelvic reconstruction uses the inferior pedicle.
VRAM Flap Anatomy
Rectus Abdominis Muscles
The rectus abdominis muscles are paired, thin and flat muscle separated by the avascular line alba. It has a triangular-like shape as the base (6cm) is wider than the insertion (3cm).
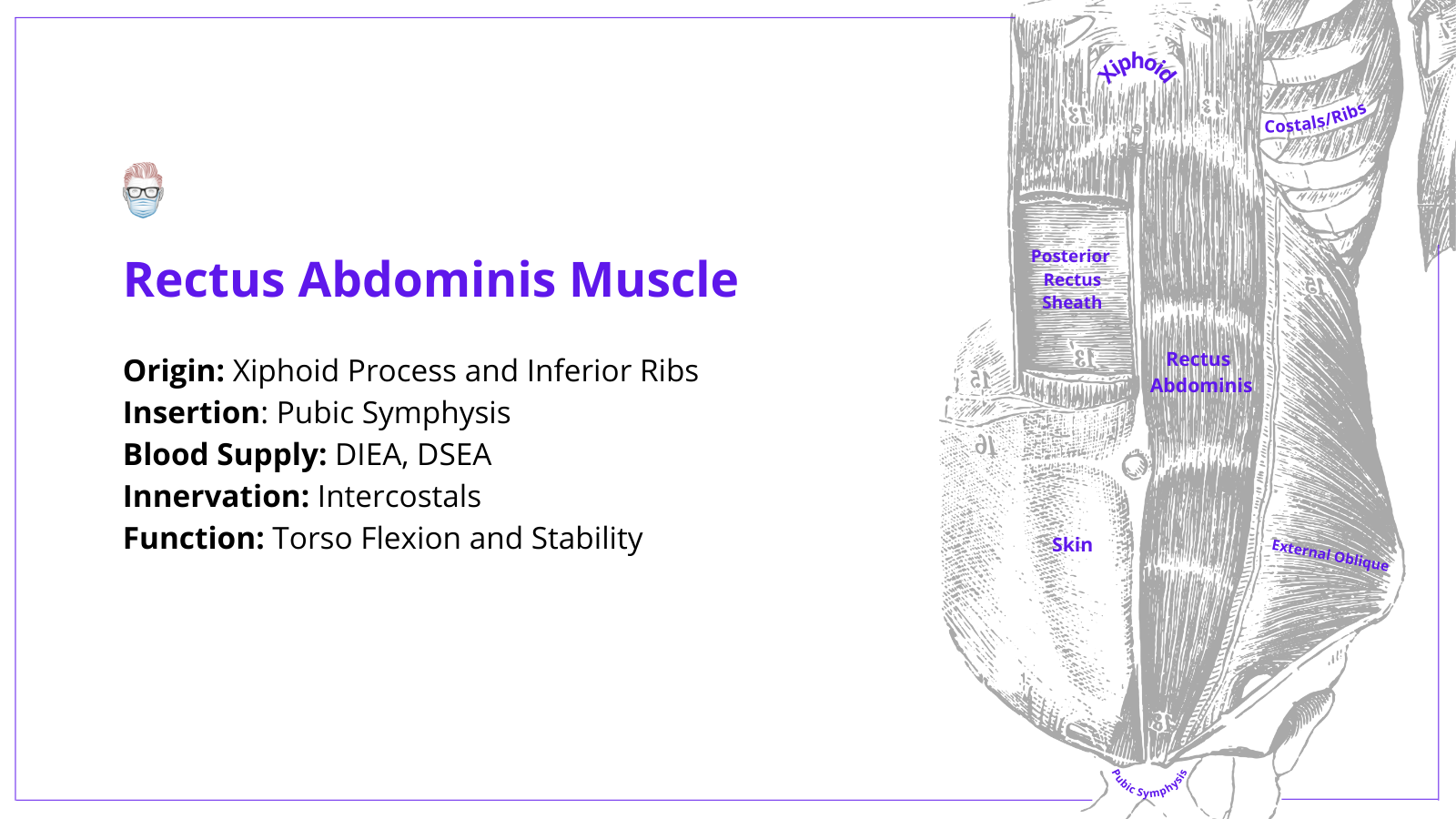
Key points are:
- Origin: anterior costal cartilages VI-VIII and xiphoid process.
- Insertion: pubic symphysis and body.
- Innervation: intercostal nerves (segmental supply reduces its role in functional muscle transfer)
- Function: tension, restrict abdominal contents, and 30° of a sit-up/crunch.
Rectus Sheath
The anterior and posterior rectus sheath can be confusing in relation to the arcuate line. To understand it, it's important to understand the 3 types of structures involved:
- 1 arcuate line: posterior sheath & transversalis fascia junction at level of ASIS
- 2 sheaths: anterior and posterior sheath
- 3 muscles: external (EO) & internal oblique (IO), transversus abdominis (TA)
There is also the transversalis fascia (TF), preperitoneal fat and peritoneum deep to the posterior sheath.
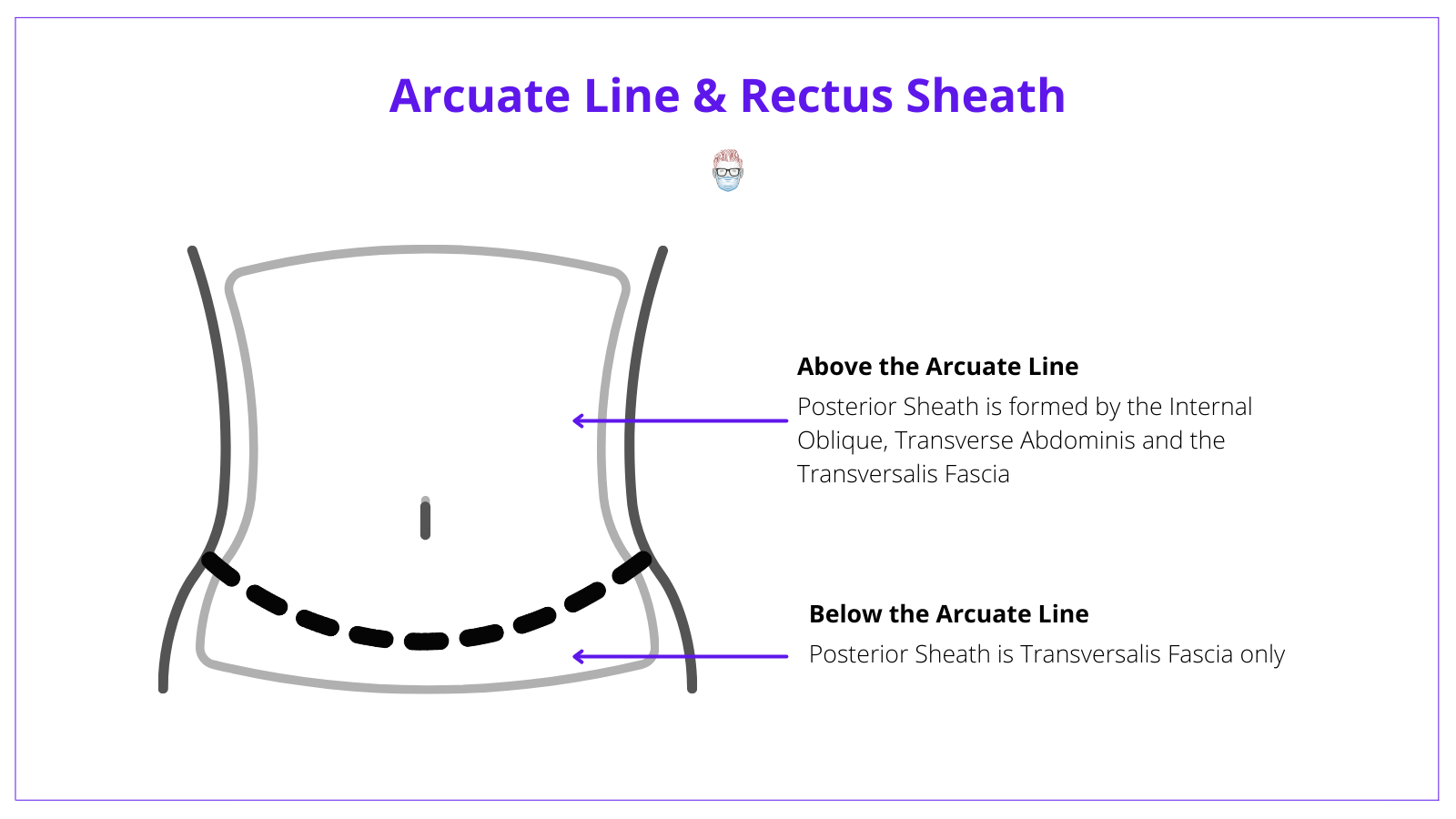
The simplest way to understand this concept is by looking at each individual sheath above and below the arcuate line:
Anterior Sheath:
- Above the AL is formed by the EO + IO
- Below the AL is formed by EO + TA + IO
Posterior Sheath:
- Above the AL is formed by the IO + TA + TF
- Below the AL is replaced by transversalis fascia (TF)
Flap Composition
The VRAM flap is a composite myocutaneous flap consisting of three layers: skin, subcutaneous fat, and muscle. Its versatility allows it to be dissected and raised as the following:
- Muscle-only
- Segmental muscle flap with preservation of part of the muscle
- Myocutaneous flap with a transverse, oblique, or vertical skin island flap
- Osseomyocutaneous (when including inferior ribs - not common)
The most commonly used myocutaneous composition consists of skin, anterior rectus sheath, rectus muscle, and the perforating vessels which connect them.
Flap Blood Supply
The rectus abdominis muscle has two major pedicles (hence Mathes and Nahai III)
- DIEA (Inferior): dominant, external iliac artery branch.
- DSEA (Superior): dominant, internal mammary artery branch
It is worth noting it does receive additional supply from the subcostal and intercostal arteries.
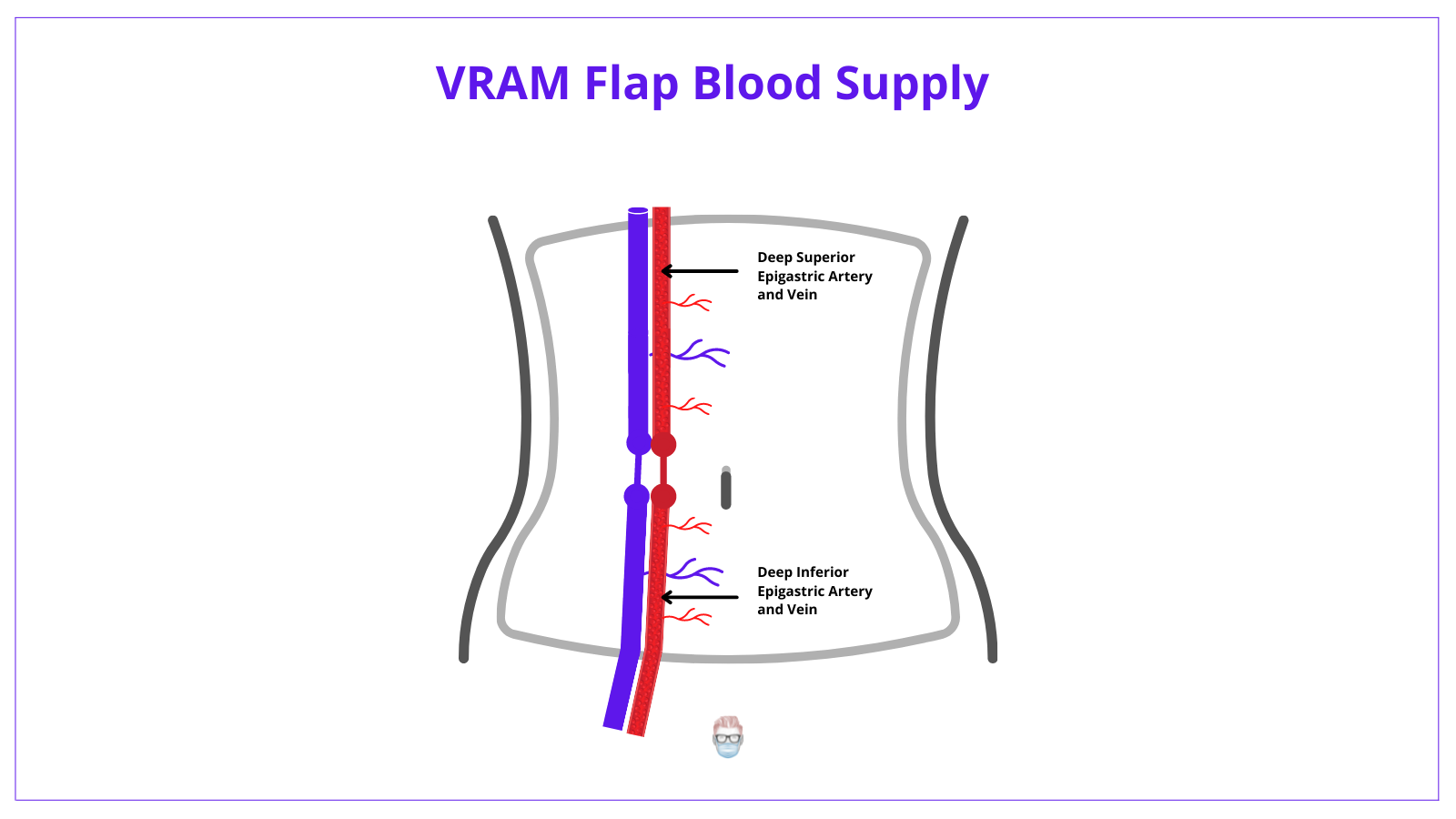
The superficial superior epigastric and circumflex arteries also play a minor role.
Venous drainage of the flap
The venous drainage primarily follows the arterial supply. The main veins involved are:
- Deep Inferior Epigastric Vein
- Deep Superior Epigastric Vein
- Superficial Inferior Epigastric Vein
VRAM flap has a motor & sensory innervation from the 7th–12th intercostal nerves.
VRAM Flap Technique
Design
The design should be considered in conjunction with the ablative surgeons in relation to stomas and planned surgical incisions.
- Identify the amount of skin island required overlying the rectus muscle.
- Mark an outline of the rectus muscle
- Incise vertically (along the muscle axis), just lateral to the midline.
- Consider including paraumbilical myocutaneous perforators into the paddle.
Dissection and Elevation
Essentially, this operation is the elevation of the rectus muscle, anterior sheath and overlying skin paddle based on the deep inferior epigastric vessels with preservation of the posterior sheath.
- Incise down to the posterior rectus sheath
- Release the rectus from its origin, semilunaris and linea alba.
- Ligate the superior epigastric vessels
- Elevate the rectus with the anterior rectus sheath and overlying skin paddle.
- Release the rectus from its insertion at the pubis
Many surgeons prefer to raise the VRAM prior to the laparotomy - to minimise potential contamination.
Inset of Flap
- Rotate the flap 180° on its DIEA pedicle
- Tunnel via an intraperitoneal route into the pelvis (gives more length) or extrapelvic subcutaneous route to the perineum.
- Assess the tension on the pedicle (not too much tension!)
Closure
- Decide if the anterior abdominal wall needs to be reinforced with an onlay mesh (above the arcuate line of the posterior sheath is often sufficient)
- Make sure the omentum is hanging towards/in the pelvis.
- Suture in 3 layers + drain insertion
Post-operative Care
A series of protocols have been designed and published. This is reflective of the different practices in departments. The following is the "Swansea" Protocol published in 20172.
- Bedrest: 5 days in a lateral position, then start mobilizing.
- Catheter: remove Day 10
- Sutures: remove Week 3
- Sit out: Week 3
- Drains: remove if <30mL/day.
Variations
VRAM flap variations do exist and are well described 1.
- Extended VRAM flap: extra flap bulk & reach (supply by intercostals)
- Fascia-sparing: lower hernia/bulge rate
- Component separation donor-site closure: lower hernia & mesh rate
- Mesh fascial closure: less fascial tension (bridged technique)
- Include greater omental flap: reduced dead space, increase healthy tissue
- Deepithelialized skin paddle: greater volume of the flap, can act as a sling.
Discussion
Advantages
- Ergonomics: often don't need to change the position of the patient
- Cosmesis: can improve body contour
- Reliability: consistent blood supply
- Versatility: raised in different compositions, inset into different areas
Disadvantages
- Abdominal wall weakening and increase risk of hernia.
- Slight functional deficit
- Difficult dissection in obese patients with increased risk of fat necrosis
References on VRAM Flap
- Campbell CA, Butler CE. Use of adjuvant techniques improves surgical outcomes of complex vertical rectus abdominis myocutaneous flap reconstructions of pelvic cancer defects. Plast Reconstr Surg. 2011 Aug;128(2):447-458. doi: 10.1097/PRS.0b013e31821e6fd2. PMID: 21788836.
- Warbrick-Smith, J., & Drew, P. J. (2018). Post-operative care of VRAM flaps for perineal reconstruction: Results of a UK practice survey and literature review. Journal of Plastic, Reconstructive & Aesthetic Surgery, 71(2), 271–273. doi:10.1016/j.bjps.2017.10.014
- Pelvic Reconstruction with Omental and VRAM Flaps: Anatomy, Surgical Technique, Normal Postoperative Findings, and ComplicationsTara L. Sagebiel, Silvana C. Faria, Aparna Balachandran, Justin M. Sacks, Y. Nancy You, and Priya R. BhosaleRadioGraphics201131:7, 2005-2019
- Blondeel N, Vanderstraeten GG, Monstrey SJ et al. The donor site morbidity of free DIEP flaps and free TRAM flaps for breast reconstruction. Br J Plast Surg 1997; 50(5): 322–330.
- Blondeel PN, Arnstein M, Verstraete K et al. Venous congestion and
blood flow in free transverse rectus abdominis myocutaneous and deep inferior epigastric perforator flaps. Plast Reconstr Surg 2000; 106(6): 1295–1299. - Boyd JB, Taylor GI, Corlett R. The vascular territories of the superior epigastric and the deep inferior epigastric systems. Plast Reconstr Surg 1984; 73(1): 1–16.
- Codner MA, Bostwick J 3rd, Nahai F, Bried JT, Eaves FF. TRAM flap vascular delay for highrisk breast reconstruction. Plast Reconstr Surg 1995; 96(7): 1615–1622.
- Koshima I, Soeda S. Inferior epigastric artery skin flaps without rectus abdominis muscle. Br J Plast Surg 1989; 42(6): 645–648.
- Mathes SJ, Nahai F. General principles. In: Mathes SJ, Nahai F (eds) Reconstructive surgery: principles, anatomy and technique. Churchill Livingstone, New York, 1997: 3–161.
- Taylor GI, Corlett RJ, Boyd JB. The versatile deep inferior epigastric (inferior rectus abdominis) flap. Br J Plast Surg 1984; 37(3): 330–350.


