In this Article
5 Key Points – Upper Eyelid Ptosis
1. What is Ptosis? Upper Eyelid Ptosis (Blepharoptosis) is defined as a drop in the eyelid 1-2mm below the upper corneal limbus when examined in primary gaze.
2. What is the cause of Ptosis? The commonest cause of ptosis is senile/involutional ptosis due to laxity in the Levator aponeurosis. Other causes can be myogenic, neurological, mechanical.
3. How to examine for Ptosis? The Upper Eyelid Ptosis assessment involves a detailed history, examination and specialist tests. The aim to to determine aetiology, degree of ptosis and Levator function. These factors influence surgical management.
4. What is pseudootosis? Pseudoptosis is an apparent ptosis not caused by an issue related to eyelid elevation. Common causes include brow ptosis and Dermatochalasia.
5. What is the treatment for ptosis? Surgical management is dependent on surgeon’s preference, degree of ptosis and levator function. Options include skin resection, muscle shortening, fat resection, aponeurosis repair.
Definition of Eyelid Ptosis
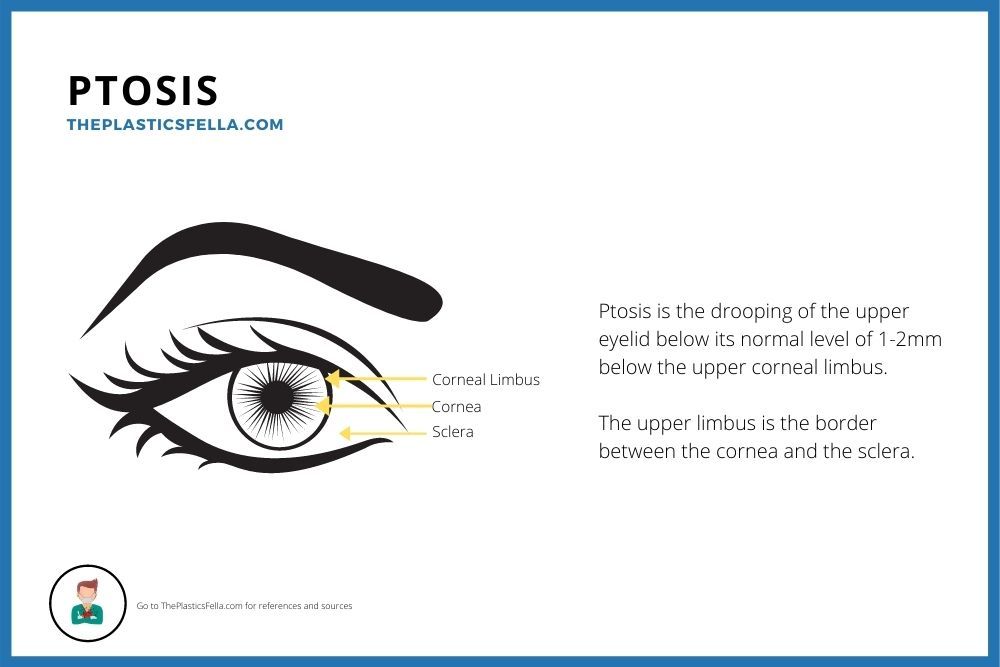
Ptosis is defined as drooping of the upper eyelid in primary gaze 1-2mm below the upper corneal limbus. It can be congenital or acquired.
The upper eyelid normally rests as 1-2mm below the corneal limbus and is highest just nasal to the pupil1. This limbus is the border between the cornea and the sclera, as shown in this labelled diagram. More detail on upper eyelid anatomy available here.
Other conditions that are similar to Ptosis and should be differentiated include:
Pseudoptosis
- Apparent ptosis unrelated to deficiency of eyelid elevation but instead a separate orbital issue such as :
- Brow Ptosis
- Enophthalmos
- Orbital Tumours
- Dermatochalasia (excess eyelid skin)
Blepharophimosis:
- Autosomal dominant condition
- Congenital small palpebral fissures due to Ptosis, Epicanthal folds, and Telecanthus
Blepharochalasis
- Excess eyelid skin and laxity of supporting structures
- Seen in young adults
- A complication of recurrent and episodic eyelid oedema, usually painless, which is refractory to anti-histamines and steroids.
Less Common:
- Steatoblepharon: excess or protruding fat through a lax septum
- Ptosis Adiposa: extreme attenuation of the canthus and septum
- Pseudoblepharoptosis: eyelid in normal position but appearance of ptosis as a result of a ptotic brow and brow skin.
Causes of Upper Eyelid Ptosis
Ptosis has congenital or acquired causes. Common acquired causes can be classified as myogenic, neurogenic, aponeurotic, mechanical, or traumatic conditions.
Senile/Involutional Ptosis is the most common cause of upper eyelid ptosis. It is caused by the stretching of the Levator aponeurosis and muscle with age. Other common causes of ptosis can be classified as myogenic, neurogenic, and mechanical causes of ptosis. This was first classified by Freuh in 19802 , as illustrated in the table below. It us best understood with a good understanding of upperand lower eyelid anatomy.
| Myogenic | Neurogenic | Mechanical |
|---|---|---|
| Senile/Involution | 3rd Nerve Palsy (paralysis Levator muscle) | Dermatochalasis |
| Myaesthenia Gravis | Horner’s Syndrome (paralyses Müller’s muscle) | Upper Lid Tumour |
| Congenital Levator Dystrophy | Demyelination (eg MS) | Scar |
| Blepharophimosis Syndrome | Anophthalmos | |
| Progressive External Opthalmoplegia |
To help determine the exact aetiology of the upper eyelid ptosis, here are some clues which may help in the diagnosis.
| Cause | Clue |
|---|---|
| Senile/Involutional | Levator function is usually good |
| Myasthenia Gravis | Worse in the day Tensilon test is diagnostic |
| Horner’s Syndrome | Effects reduced with 10% phenylephrine hydrochloride |
Assessment of Upper Eyelid Ptosis
The cause, degree of ptosis and levator function should be established through history, examination, and specific ptosis tests. These 3 factors will guide treatment options for upper eyelid ptosis.
Ptosis History
- Time: Congenital, Acquired, and Precipitating and Exacerbating events
- Symptoms: Functional, Aesthetic or both
- Medical History: Diabetes, Myasthenia Gravis, Grave’s Disease, Coagulopathies, Renal or Cardiac issues that may predispose to edema.
- Specific Ocular History: Visual Impairment or Correction, glaucoma, excess tearing, dry eyes, Laser Surgery, Contacts
- Family History
- Social History: Smoking, Occupation, Home Support
Forehead Examination
| Exam | Location | Notes |
|---|---|---|
| Look | Frontalis Crease | Sign of effort to keep brows raised |
| | Glabellar Crease | Indicates corrugator hyperactivity |
| Brow Position | If ptotic, can cause pseudootosis of the eyelid. | |
| Feel/Move | Compensated Brow Ptosis | Increased Brow ptosis when hyperactive frontalis is immobilised. If present, keep brow in correct position for remainder of examination |
Upper Eyelid Examination
| Exam | Location | Notes |
|---|---|---|
| Look | Lid position | 1-2mm below superior limbus |
| Globe Position | Proptosis, enopthalmos causes pseudoptosis. | |
| Globe Vector3 | Negative vector (anterior cornea is anterior to the orbital rim) is linked to post-op lid malposition. A canthopexy is an option. | |
| Intercanthal Tilt4 | Lateral 2mm superior to medial. Negative tilt linked to lateral canthus pathology. | |
| Skin Quantity | Dermatochalasis causes pseudoptosis & lateral hooding | |
| Fat Quantity | Herniation (pseudohernia) or excess pre-septal fat. | |
| Levator dehiscence | Higher skin crease with a deeper upper lid sulcus. | |
| Feel/Move | Levator function/excursion | The upper eyelid movement when brow is immobilised (10-15mm). |
| Bell’s Phenomenon | Upward rolling of eye on resisted eyelid closure, suggests the cornea can be protected in the event of lagophthalmos. |
Lower Lid Examination
| Exam | Location | Notes |
|---|---|---|
| Look | Lid position | 1-2mm below inferior limbus. Scleral show linked to proptosis & poor support. |
| Skin | Rhytids: Redundant Skin Pigment: Blepharomelasma | |
| Fat Herniation | 3 compartments | |
| Festoons | Eye closure improvess festoon if caused by ptotic orbicularis. | |
| Malar Bag | Shelving of orbicularis over orbital retaining ligament with excess intra-orbital fat. Correction involves improving lid-cheek junction (Loeb procedure, septal reset, midface lift) | |
| Trough Deformity | Medial Concavity at the border of eyelid and cheek due to fat herniation and tight attachment of the orbital septum. | |
| Feel/Move | Pinch Test/Snap Back | If slow to conform to eye it is indicated of tarsal laxity |
Additional Tests
| Exam | How | Why |
|---|---|---|
| Vision | Snellen Chart, Fundoscopy, Ocular Movements | Baseline assessment |
| Tears Production | Schirmer Test | Filter paper in the inferior fornix should collect >5mm in 5 minutes. Consider if dry-eye symptoms |
| Müller Muscle | Phenylephrine Test | If stimulation of Muller’s muscle restores normal lid position, this suggests suitability for Muller’s muscle shortening. |
| Fatigue | Look up for 30 seconds | Drop in upper eyelids from fatigue is linked to myasethenia gravis. |
| Marginal-reflex distance | Look at light source 50cm away and measure distance from corneal light reflex to lid | <2.5mm is clinically significant ptosis. |
Normal Eyelid Measurements
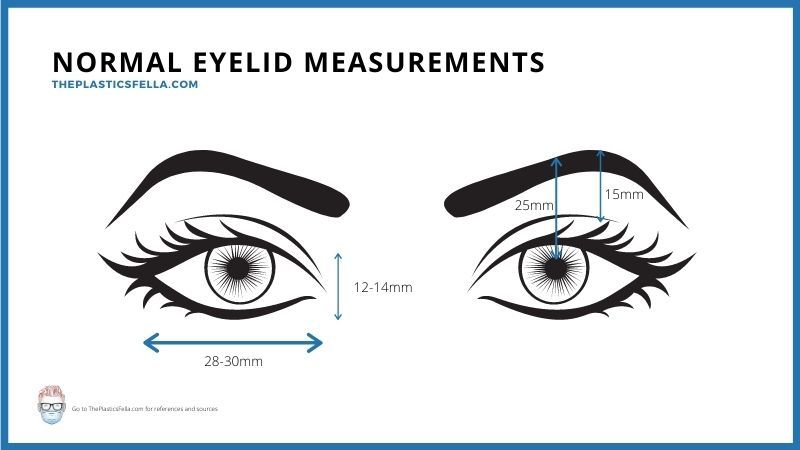
Normal eyelid measurements have been extensively published. More information on upper eyelid anatomy is available here. The following table provides approximations of upper eyelid measurements5,6
| Landmark | Measurement |
|---|---|
| Vertical Palpebral Fissure | 12-14mm |
| Horizontal Palpebral Fissure | 28-30mm |
| Visible Pre-Tarsal Skin | 3-6mm |
| Lash line to supra tarsal crease | 8-10mm |
| Lateral Canthus | 1-2mm above medial cants |
| Anterior hardline to brow | 5-6cm |
| Brow to orbital rim | 1cm (less in males) |
| Brow to midpupil | 2.5cm |
Treatment of Upper Eyelid Ptosis
Treatment of upper eyelid ptosis is influenced by patient factors, surgical preference, aetiology and examination findings. In particular, the degree of ptosis and Levator function.
The surgical treatment options for upper eyelid ptosis is dependent on both patient and surgeon factors. The goal of a blepharoplasty The following table provides a rough guide to management, which is influence by degree of ptosis and Levator function.
| Ptosis | Levator | Surgery | Note |
|---|---|---|---|
| Mild (1-2mm) | Good (>10mm) | Müller Shortening | Fasanella-Servat |
| Moderate (3-4mm) | Good (>10mm) | Aponeurosis Repair | Anterior or Posterior |
| Moderate (3-4mm) | Fair (5-10mm) | Levator resection or advancement | Anterior or Posterior |
| Severe (>4mm) | Poor (<5mm) | Frontalis Suspension | Crawford or Fox |
References
Upper Eyelid Ptosis Bibliography
- Finsterer J. Ptosis: causes, presentation, and management. Aesthetic Plast Surg. 2003;27(3):193-204. doi:10.1007/s00266-003-0127-5
- Frueh B. The mechanistic classification of ptosis. Ophthalmology. 1980;87(10):1019-1021. doi:10.1016/s0161-6420(80)35135-x
- Jelks G, Jelks E. The influence of orbital and eyelid anatomy on the palpebral aperture. Clin Plast Surg. 1991;18(1):183-195. https://www.ncbi.nlm.nih.gov/pubmed/2015744
- Jelks G, Jelks E. Preoperative evaluation of the blepharoplasty patient. Bypassing the pitfalls. Clin Plast Surg. 1993;20(2):213-223; discussion 224. https://www.ncbi.nlm.nih.gov/pubmed/8485931
- Bartlett S, Wornom I, Whitaker L. Evaluation of facial skeletal aesthetics and surgical planning. Clin Plast Surg. 1991;18(1):1-9. https://www.ncbi.nlm.nih.gov/pubmed/2015737
- Farkas L, Kolar J. Anthropometrics and art in the aesthetics of women’s faces. Clin Plast Surg. 1987;14(4):599-616. https://www.ncbi.nlm.nih.gov/pubmed/3652607


