Summary Card
Definition
Ulnar tunnel syndrome or Guyon’s canal syndrome is compression of the ulnar nerve as it runs through the osseofibrous ulnar tunnel of the wrist.
Anatomy
The ulnar tunnel is formed by the hamate, pisiform, transverse carpal ligament, volar carpal ligaments, and hypothenar aponeurosis.
Aetiology
There are several causes of ulnar tunnel syndrome, of which ganglion is the most common.
Clinical Presentation
Clinical features depend on location of compression and may be motor, sensory, or both.
Investigations
An X-ray is the primary investigation. US and MRI can be used to look for soft tissue masses resulting in external compression.
Management
Non-surgical treatment includes lifestyle advice, physiotherapy, and splinting. Surgery is indicated when these measures fail.
Primary Contributor: Dr Suzanne Thomson, Educational Fellow.
Reviewer: Dr Kurt Lee Chircop, Educational Fellow.
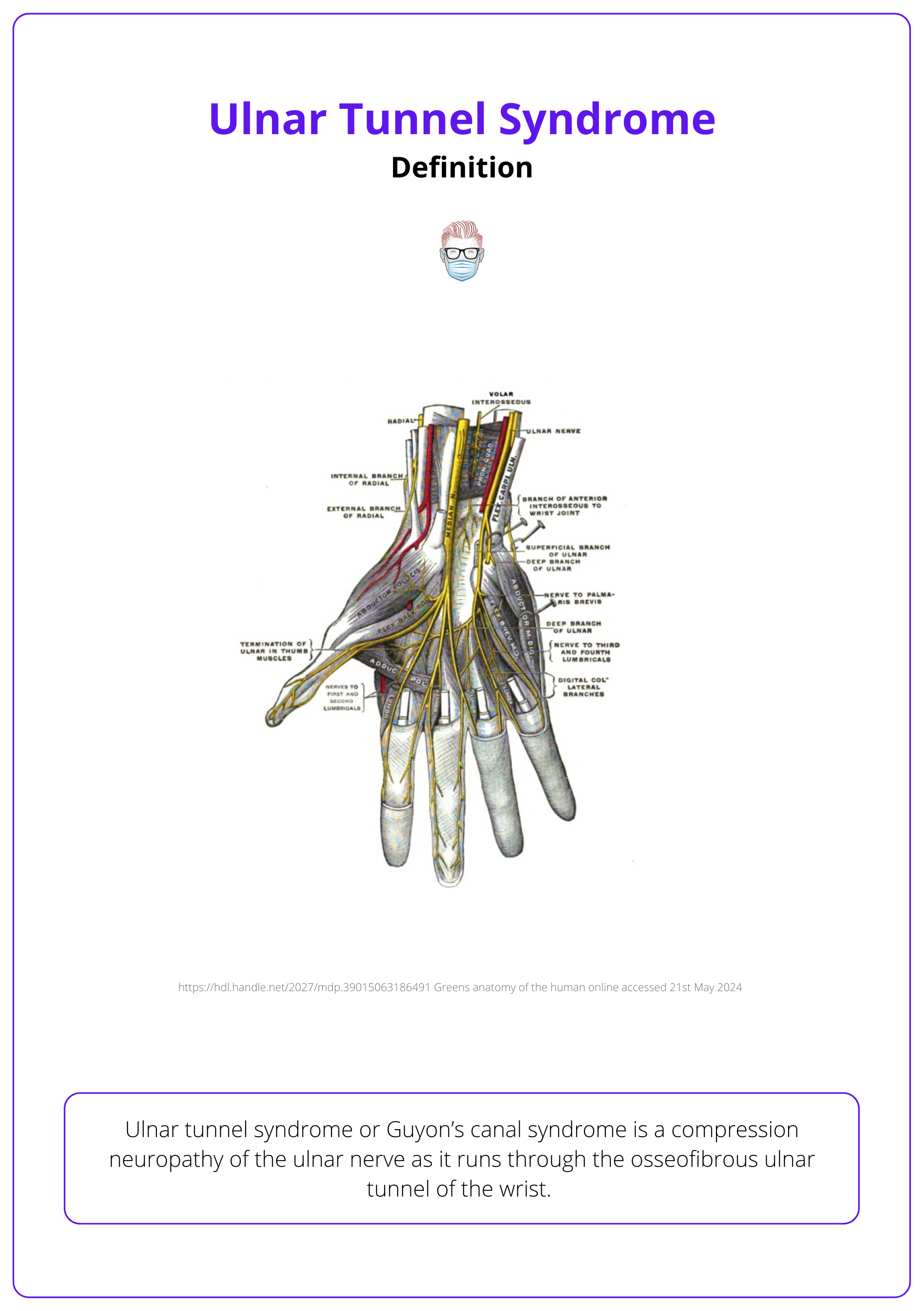
Definition of Ulnar Tunnel Syndrome
Ulnar tunnel syndrome or Guyon’s canal syndrome is a compression neuropathy of the ulnar nerve as it runs through the osseofibrous ulnar tunnel of the wrist.
Ulnar tunnel syndrome or Guyon’s canal syndrome is a compression neuropathy of the ulnar nerve as it runs through the osseofibrous ulnar tunnel of the wrist. Key points to understand include:
- It is also known as Guyon’s canal, named after the French surgeon who originally described it (Guyon, 1861).
- It is far less common compared to cubital tunnel syndrome.
The image below further illustrates the ulnar nerve in the ulnar tunnel.
Anatomy of the Ulnar Tunnel
The ulnar tunnel is formed by the hamate, pisiform, transverse carpal ligament, volar carpal ligaments, and hypothenar aponeurosis. It is considered in three zones (mixed, motor, and sensory) from proximal to distal.
Anatomical Boundaries
The ulnar tunnel is the osseofibrous tunnel that the ulnar nerve and artery pass through at the level of the carpus. The anatomical borders of Guyon’s Canal are:
- Radial Boundary: Hook of the hamate
- Ulnar Boundary: Pisiform
- Floor: Formed by the Transverse Carpal Ligament
- Roof: Consists of the Volar Carpal Ligament and Hypothenar Aponeurosis
The anatomical positioning of the ulnar tunnel is illustrated in the image below.
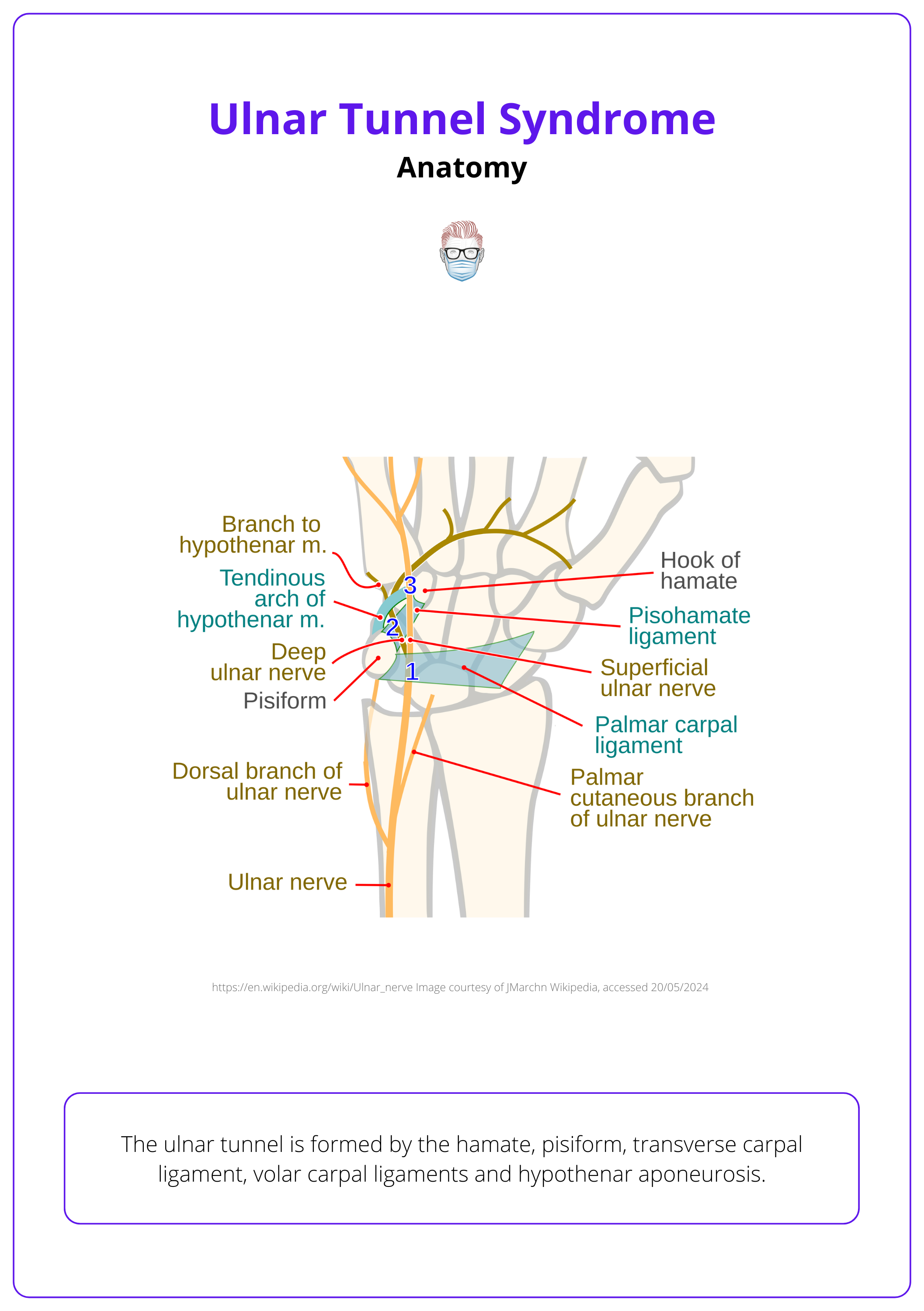
Fractures of the hook of the hamate typically lead to compression in Zone 2 of Guyon's canal. This compression primarily affects the deep motor branch of the ulnar nerve.
Zones of the Canal
The ulnar nerve and artery pass through it and the canal can be considered in 3 zones based on the location and subsequent nerve fibres involve:
- Zone 1: Mixed motor and sensory
- Zone 2: Motor (most common)
- Zone 3: Sensory
These zones are illustrated in the table below with their anatomical location.
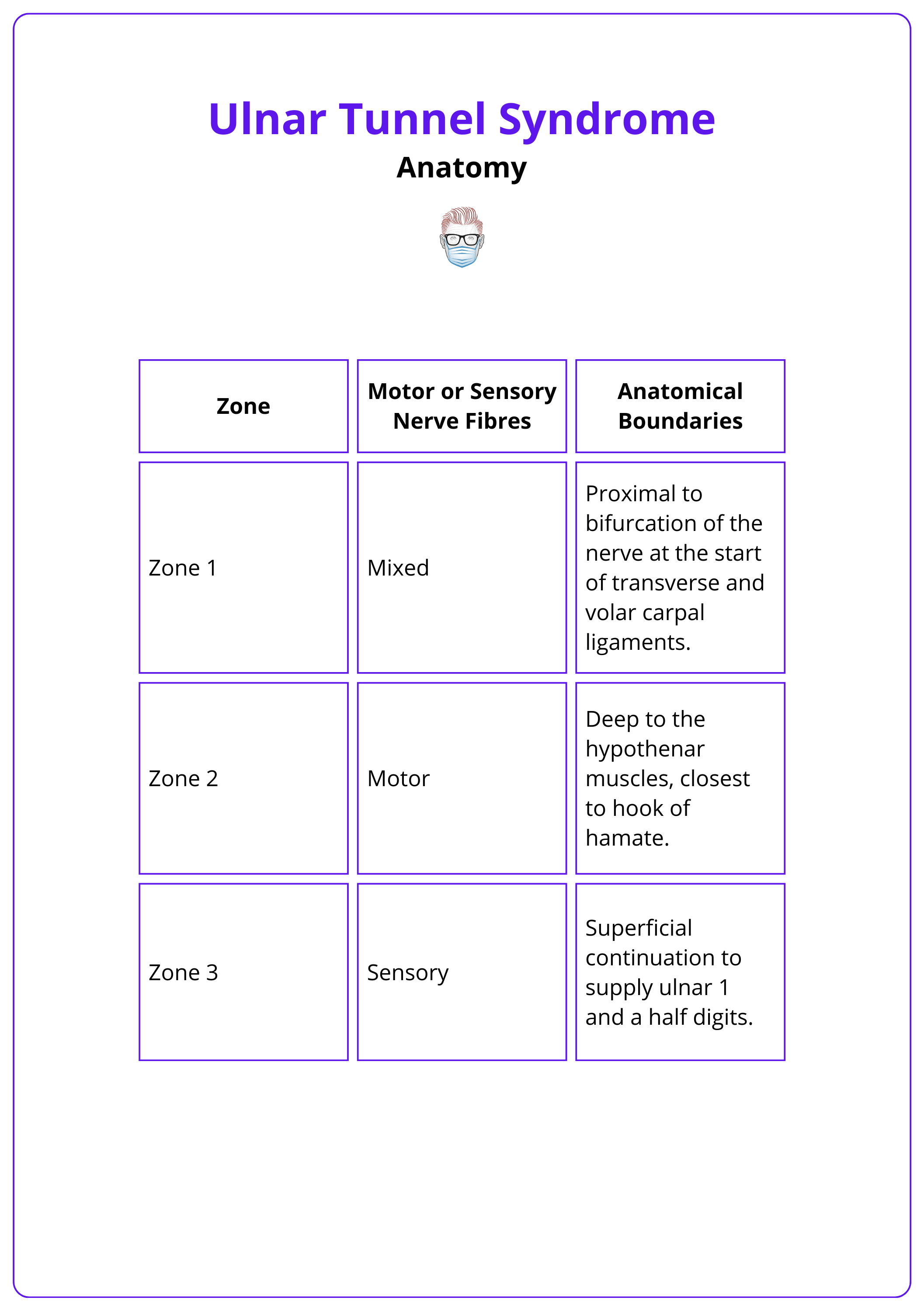
The dorsal cutaneous nerve of the hand branches from the ulnar nerve before it enters Guyon's canal, preserving sensation to the back of the hand in ulnar tunnel syndrome.
Aetiology of Ulnar Tunnel Syndrome
There are several causes of ulnar tunnel syndrome, of which ganglion is the most common.
The most common cause of ulnar tunnel syndrome/compression in Guyon's canal is a ganglion or intra-neural cyst (Lee, 2022). Less common causes include:
- Trauma: Hook of hamate fracture, repetitive external compression
- Anomalous muscles: Palmaris duplicates, Hypothenar or FCU variants
- Vascular: Ulnar artery thrombosis or aneurysm
In Seddon’s original descriptions of surgical treatment for ulnar nerve compression, a ganglion caused compression in four of the first five cases of Guyon's canal that he explored. (Listers The Hand).
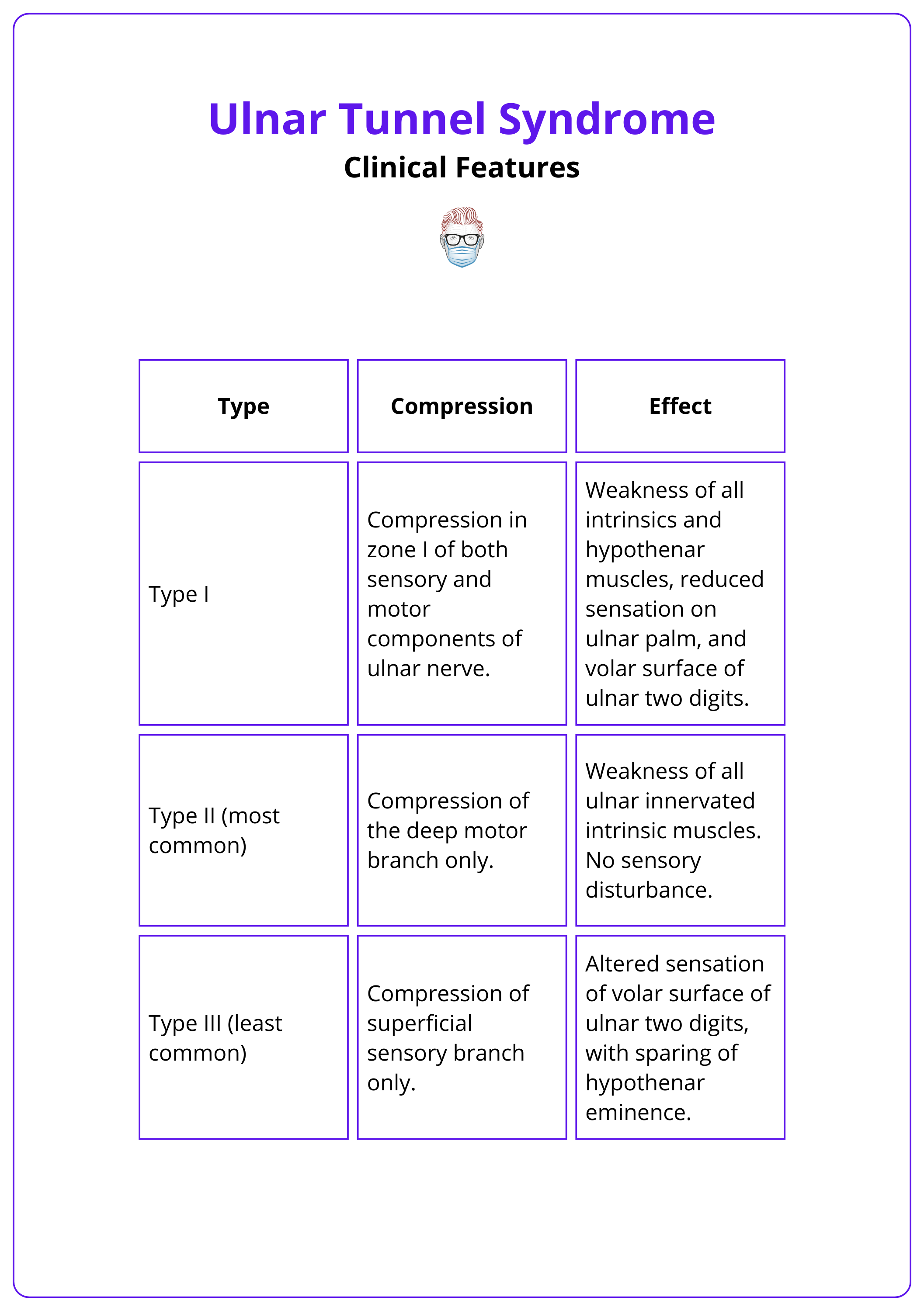
Clinical Features of Ulnar Tunnel Syndrome
Clinical features may be motor, sensory, or both, depending on the location of compression. Symptoms include ulnar-sided wrist pain, muscle weakness, and sensory disturbance in the ulnar digits, with preservation of sensation on the dorsum.
Ulnar Tunnel Syndrome can have motor, sensory, or mixed clinical features. These features are determined by the location of injury to the ulnar nerve (Hoogvleit, 2013).
Motor Symptoms
Motor symptoms can occur with an ulnar nerve injury in zone 2, the most common location. They can also occur in Zone 1 injuries (mixed motor and sensory). Classic features include:
- Dropping objects: loss of fine motor control.
- Interosseous and hypothenar muscle wasting
- Positive Froment's sign: Inability to adduct thumb to hold paper, compensated by flexing flexor pollicis longus due to weak adduction.
Sensory Symptoms
Sensory symptoms can occur with an ulnar nerve injury in zone 3. They can also occur in Zone 1 injuries (mixed motor and sensory). Classic features include:
- Pain at the wrist radiating to the ulnar two digits.
- Sensory disturbance in ulnar digits.
- Symptoms are exacerbated at night or by activity.
Three types of ulnar tunnel syndrome are classified based on the level of nerve compression within Guyon’s canal, as outlined in the table below.
Other tests to evaluate the cause:
- Pain over the hook of the hamate indicating fracture.
- Ulnar artery aneurysm may be palpable.
- Positive Tinel Hoffman percussion test.
Keen cyclists are at risk of ulnar tunnel syndrome due to prolonged and repetitive compression of the ulnar nerve within Guyon’s canal when the hand is resting on the handlebars (Hoogvleit, 2013).
Investigations for Ulnar Tunnel Syndrome
Radiological investigations can be used to look for soft tissue masses resulting in external compression. Nerve conduction studies can delineate in which zone of the ulnar tunnel the ulnar nerve is compressed.
Radiological Investigations
Ulnar Tunnel Syndrome can have a bone or soft tissue aetiology. Clinical assessment will help guide the relevant imaging modality. Options include:
- X-ray: Demonstrate hamate or pisiform fracture.
- US: Demonstrate soft tissue lesions or ulnar artery anomalies, nerve elastography may be useful to demonstrate compression, depending on user experience.
- MRI: Further delineate mass lesions and increasingly detailed anatomy.
Electrophysiology
Increased latency of sensory action potentials in zone I and zone III compressions while increased motor latency and decreased compound muscle action potentials in zone II compression.
Diffusion tensor imaging (dTI) is a promising MRI technique that measures nerve alignment. It may become a standard, non-invasive method for diagnosing cubital tunnel syndrome and other nerve compression syndrome (Griffiths, 2021).
Management of Ulnar Tunnel Syndrome
Non-surgical treatment includes lifestyle advice, physiotherapy, and splinting. Surgical decompression is indicated if refractory to conservative management.
Non-surgical
For mild ulnar tunnel syndrome lasting less than 3 months, lifestyle modifications can be effective. Recommendations include avoiding ulnar compression, such as altering hand position on bicycle handlebars.
- Splinting: The wrist should be splinted in a neutral position, with or without the inclusion of fingers. A Delphi study of expert opinions shows variation in the recommended duration of splinting, ranging from 1 to 12 weeks (Hoogvleit, 2013)
- Nerve Gliding Exercises: These can help alleviate symptoms.
- Medications: NSAIDs and steroids are generally not effective for ulnar tunnel syndrome.
Surgical
Surgery is indicated for severe or persistent symptoms unresponsive to basic interventions. The goal is to release pressure on the ulnar nerve by dividing the roof of Guyon’s canal (volar carpal ligament).
- Incision: Commonly, a carpal tunnel incision is used.
- Nerve Protection: Identify and protect the cutaneous nerve in the distal wound (15% incidence).
- Ligament Division: Divide the volar carpal ligament and possibly some palmaris brevis fibers.
- Identify Structures: Locate the hook of the hamate.
- Nerve Exposure: Expose the full length of the ulnar nerve.
- Hemostasis: Use microcautery for bleeding vessels.
- Muscle Release: Release the aponeurotic arch of the hypothenar muscles with tenotomy scissors.
- Decompression Extent: Decompress up to the antebrachial fascia.
- Wound Closure: Use simple interrupted sutures.
This 5-minute video by Susan McKinnon demonstrates the key steps.
At least 5 different surgical incisions are used to release the ulnar tunnel, the most widely used being the carpal tunnel incision (Hoogvleit, 2013).
Conclusion
1. Understanding Ulnar Tunnel Syndrome: You've learned about Ulnar Tunnel Syndrome and its definition as a compression neuropathy of the ulnar nerve at the wrist.
2. Anatomy: You've gained insights into the anatomical features of the ulnar tunnel, including its formation by the hamate, pisiform, and surrounding ligaments and aponeuroses.
3. Identifying Causes: You now understand the various aetiologies of ulnar tunnel syndrome, with ganglions being the most common cause among others such as anomalous muscles and hypothenar anomalies.
4. Clinical Presentation: You've learned how the symptoms of ulnar tunnel syndrome can vary based on the exact location of nerve compression, affecting motor and/or sensory functions.
5. Diagnostic Tools: You are now familiar with the primary and supplementary diagnostic tools for this condition, including X-ray, ultrasound, MRI, and electrophysiological studies.
6. Management Strategies: You've understood the management options ranging from non-surgical approaches like physiotherapy and splinting to surgical interventions when necessary.
Further Reading
- Barton N. Lister’s “the hand”: diagnosis and indications. J Bone Joint Surg Br. 2003;85-B(1):152-152. doi:10.1302/0301-620X.85B1.0850152
- Greens DP, Wolfe SW. Green’s Operative Hand Surgery. 6th ed. Elsevier/Churchill Livingstone; 2011. Accessed May 22, 2024. http://www.clinicalkey.com/dura/browse/bookChapter/3-s2.0-C20091589800
- Guyon, Felix (1861). "Note sur une disposition anatomique propere a la face anterieure de la region du poignet et non encore decrite". Bull Soc Anat Paris. 6: 184–186.
- Spinner RJ. The longest intraneural ganglion cyst: it's not about size but principle(s). J Plast Reconstr Aesthet Surg. 2014 Feb;67(2):e69-70. doi: 10.1016/j.bjps.2013.09.002. Epub 2013 Sep 11. PMID: 24074634.
- Bachoura A, Jacoby SM. Ulnar tunnel syndrome. Orthop Clin North Am. 2012 Oct;43(4):467-74. doi: 10.1016/j.ocl.2012.07.016. PMID: 23026462.
- Lee JH, Lee JK, Park JS, Kim DH, Baek JH, Yoon BN, Kim S, Ha C, Cho WM, Han SH. Characteristics of surgically treated Guyon canal syndrome: A multicenter retrospective study. J Plast Reconstr Aesthet Surg. 2022 Sep;75(9):3269-3278. doi: 10.1016/j.bjps.2022.04.049. Epub 2022 Apr 27. PMID: 35654688.
- Hoogvliet P, Coert JH, Fridén J, Huisstede BM; European HANDGUIDE group. How to treat Guyon's canal syndrome? Results from the European HANDGUIDE study: a multidisciplinary treatment guideline. Br J Sports Med. 2013 Nov;47(17):1063-70. doi: 10.1136/bjsports-2013-092280. Epub 2013 Jul 31. PMID: 23902776.
- Griffiths TT, Flather R, Teh I, Haroon HA, Shelley D, Plein S, Bourke G, Wade RG. Diffusion tensor imaging in cubital tunnel syndrome. Sci Rep. 2021 Jul 22;11(1):14982. doi: 10.1038/s41598-021-94211-7. PMID: 34294771; PMCID: PMC8298404.
- Sinha, S. Pinder, R. M., & Majumder, S. (2013). The largest reported epineural ganglion of the ulnar nerve causing cubital tunnel syndrome: case report and review of the literature. Journal of Plastic, Reconstructive & Aesthetic Surgery, 66(1), e23-e25.


