Summary Card
Definition
Trigger finger (stenosing tenosynovitis) is a condition where the flexor tendon becomes trapped at the A1 pulley.
Anatomy
Trigger finger results from mechanical pathology within the flexor tendon and pulley system, involving thickening of the A1 pulley and impaired tendon gliding.
Clinical Features
Physical examination often reveals a palpable nodule, pain over the A1 pulley, and active triggering during movement.
Grading
The Green classification is commonly used to stratify trigger fingers based on the degree and reversibility of triggering.
Management
Management of a trigger finger is initially conservative. Surgical release of the A1 pulley is reserved for severe cases.
Primary Contributor: Dr Kurt Lee Chircop, Educational Fellow.
Reviewer: Dr Waruguru Wanjau, Educational Fellow.
Definition of Trigger Finger
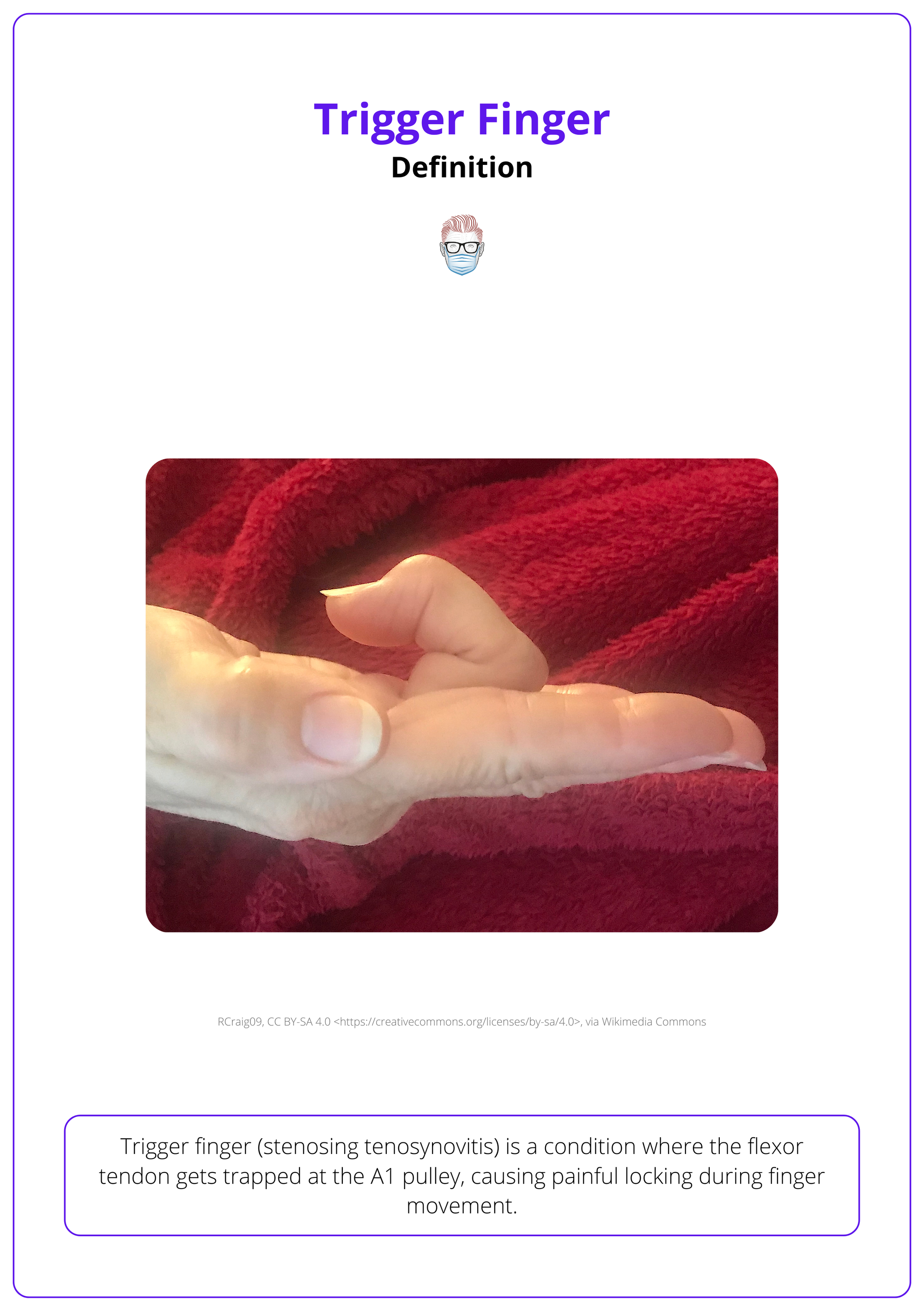
Trigger finger (stenosing tenosynovitis) is a condition caused by flexor tendon entrapment at the A1 pulley, leading to painful locking or catching during finger movement.
Trigger finger, also known as stenosing tenosynovitis, results from the entrapment of the flexor tendon as it passes through the A1 pulley of the digital sheath. This condition commonly causes pain & or locking during flexion and extension, impairing hand function.
Trigger Finger affects 2–3% of the general population with well-defined demographic patterns and risk factors, including,
- Age: Adults aged 40 to 60 years (Makkouk, 2008).
- Females: Twice as likely to develop trigger finger than men (Saldana, 2001).
- Affected Digits: Ring & middle fingers are most common (Makkouk, 2008).
- Systemic Conditions: Bilateral cases are more common in patients with diabetes or rheumatoid arthritis (Baumgarten, 2007).
An example of a trigger finger can be seen below.
Anatomy of a Trigger Finger
Trigger finger results from mechanical pathology within the flexor tendon and pulley system, specifically involving thickening of the A1 pulley and impaired tendon gliding.
The flexor tendon pulley system ensures smooth finger movement. A trigger finger arises from A1 pulley dysfunction and tendon inflammation, causing pain and locking during motion.
Pulley Anatomy of the Fingers
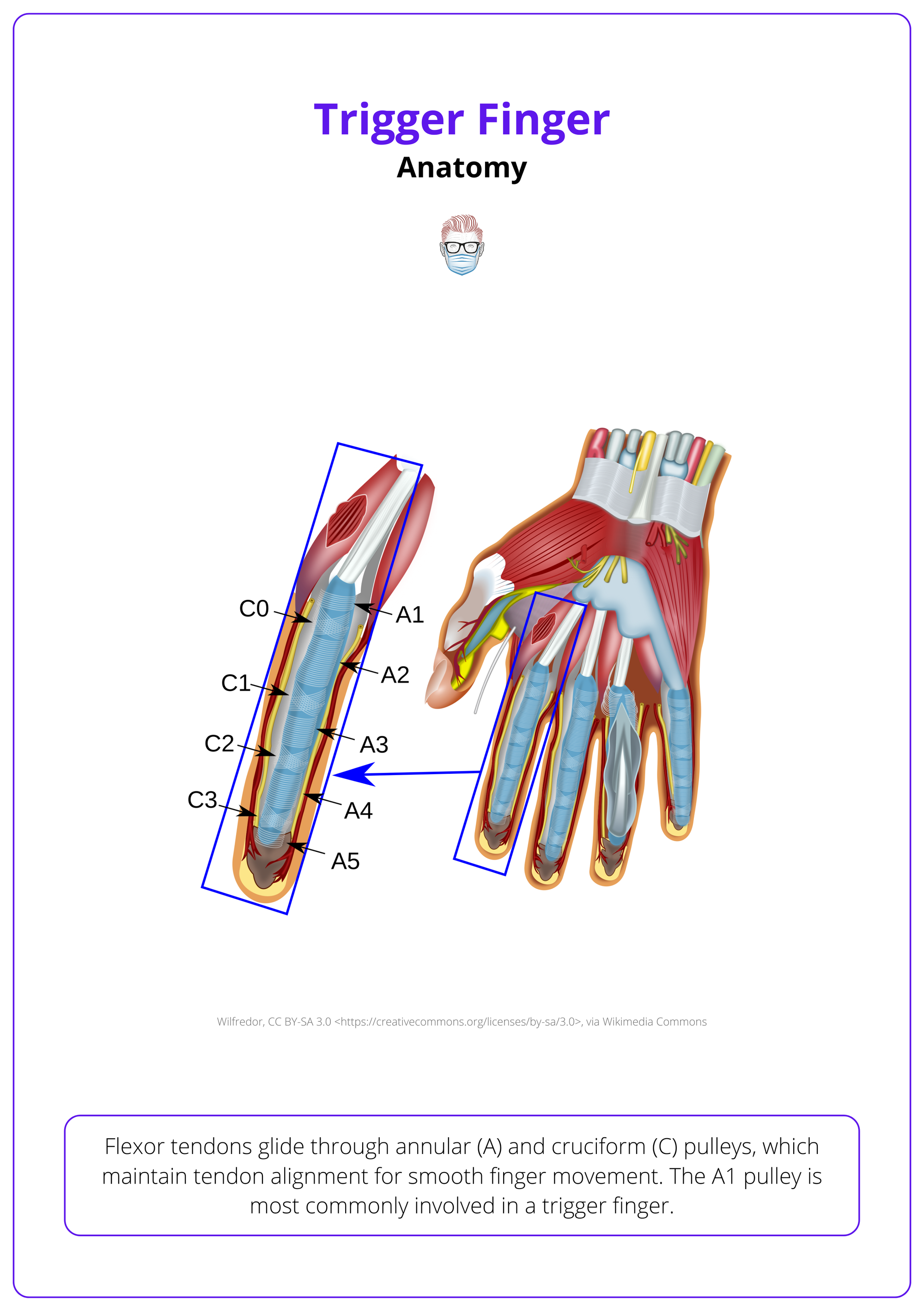
Flexor tendons glide through annular (A) and cruciform (C) pulleys, which maintain tendon alignment for smooth finger movement. The A1 pulley is most commonly involved in trigger fingers.
- Annular (A) Pulleys: Ring-like structures that anchor the tendons close to the phalanges, named A1 to A5.
- A1: Located at the MCP joint, frequently implicated in trigger finger.
- A2: Over the proximal phalanx, essential for preventing bowstringing.
- A3: Found at the PIP joint.
- A4: Spanning the middle phalanx.
- A5: Positioned at the DIP joint.
- Cruciform (C) Pulleys: Cross-shaped structures located between annular pulleys (C1-C3). They maintain flexor sheath integrity but are less critical for function compared to annular pulleys.
The anatomy of a trigger finger is illustrated below.
Pathology of Trigger Finger
Trigger finger is characterized by changes within the A1 pulley and flexor tendon that disrupt normal tendon gliding.
Mechanical Pathology
- A1 Pulley Thickening: Narrows the tendon sheath and limits movement.
- Tendon Nodule Formation: Caused by friction and inflammation of the flexor digitorum profundus tendon.
- Tendon Inflammation: Leads to fibrosis, further impairing motion.
Pathophysiological Changes (Brozovich, 2019)
- Fibrocartilaginous Metaplasia: Abnormal tissue changes in the tendon and/or pulley.
- Increased Type III Collagen: Contributes to fibrosis and structural abnormalities.
- Collagen Cross-linking: Exacerbated by hyperglycemia, common in diabetes, impeding collagen breakdown.
- Triggering Mechanism: During flexion, the thickened A1 pulley can trap the flexor tendon, causing locking or "triggering." (Saldana, 2001)
Damage to cruciform pulleys alone generally does not cause significant functional issues unless combined with annular pulley damage.
Clinical Features of Trigger Finger
Trigger finger is characterized by pain, locking during finger movements, and difficulty straightening the affected digit. A palpable nodule and active triggering are hallmark findings during physical examination.
Trigger finger, also known as stenosing tenosynovitis, presents with progressive symptoms affecting hand function. Diagnosis is primarily clinical and is often associated with specific systemic conditions, occupational factors, and demographic risk factors.
History
Trigger finger symptoms are typically progressive and worsen over time.
- Pain: Localized at the base of the affected digit, near the A1 pulley.
- Locking or Triggering: Difficulty straightening the finger, often accompanied by a locking sensation during movement.
- Stiffness: Especially pronounced in the morning or after prolonged inactivity
Trigger finger is linked to several risk factors.
- Systemic Conditions: Diabetes, rheumatoid, sarcoidosis, gout, and amyloidosis (Vasiliadis, 2017).
- Occupational Factors: Frequent use of hand tools or repetitive manual labor is associated with increased risk.
- Demographics: Females (2:1 ratio) aged 40–60 years (Saldana, 2001).
- Congenital Cases: Rarely seen in children, often involving the thumb.
Paediatric trigger finger is a congenital condition, often presenting with Notta's node and flexion contracture. Surgical intervention is recommended between 2-4 years of age to prevent interphalangeal joint contracture.
Physical Examination
Key findings during the clinical evaluation of trigger finger include,
- Palpable Nodule: A tender nodule at the metacarpal head, associated with tendon thickening.
- Triggering: Observable during active or passive flexion-extension movements.
- Pain: Tenderness localized over the A1 pulley.
The video below shows the clinical presentation of a trigger finger.
Clinical presentation of a trigger finger
Differential Diagnosis
Trigger finger is rarely misdiagnosed. In unusual cases, other conditions that mimic trigger finger must be excluded.
- Dupuytren’s Contracture: Fixed flexion deformity caused by palmar fascia thickening.
- Lumbrical Plus Finger: Unexpected IP joint extension during attempted flexion, caused by FDP retraction.
- Extensor Tendon Injuries: Lacerations or ruptures secondary to trauma.
Lumbrical Plus Finger can cause unexpected extension of the IP joints during flexion attempts. Treatment includes FDP tenodesis or lumbrical release for symptomatic cases (Schuind, 2018).
Grading of Trigger Finger
The Green classification is a system for grading trigger finger, categorizing severity based on the degree of triggering and reversibility.
Trigger finger is assessed using the Green classification, which stratifies the condition to guide treatment and prognosis (Dala-Ali, 2012)
Grade I: Pre-triggering
- Mild pain and tenderness over the A1 pulley.
- No locking or mechanical obstruction.
Grade II: Triggering with Intermittent Locking
- Locking during movement that can be corrected passively.
Grade III: Locked Finger
- Grade IIIa: Patient can correct the locking manually.
- Grade IIIb: Correction requires external force.
Grade IV: Fixed Flexion Contracture
- Irreversible flexion deformity due to prolonged mechanical obstruction or fibrosis.
Management of Trigger Finger
Treatment for trigger finger starts with conservative measures like activity modification, splinting, NSAIDs, and corticosteroid injections. Surgical release of the A1 pulley is reserved for persistent or severe cases.
Management of trigger finger is guided by the severity of symptoms and response to non-invasive treatments. Non-surgical interventions are typically first-line, with surgery considered for refractory or severe cases (Gil, 2020).
Non-Surgical Treatment
- Activity Modification: Avoid repetitive hand movements or prolonged use of hand tools.
- Splinting: Night splints are effective for reducing symptoms by immobilizing the affected finger.
- NSAIDs: Alleviate pain and inflammation but are generally supportive rather than definitive.
- Corticosteroid Injections
- First-line for many patients, particularly effective for reducing inflammation in the tendon sheath.
- Provides symptom relief in 50%-80% of cases (Baumgarten et al., 2007).
- Less effective in diabetic patients due to altered tissue response.
Surgical Management
For patients with persistent or severe symptoms, surgery may be required to release the mechanical obstruction.
- Open A1 Pulley Release
- Standard surgical approach through a small incision.
- Offers symptom relief in over 90% of cases (Gil, 2020).
- Percutaneous Release
- Minimally invasive, performed with a needle to divide the A1 pulley.
- Associated with quicker recovery but carries a higher risk of nerve injury compared to open techniques (Cebesoy et al., 2007).
- Excision of Flexor Digitorum Superficialis (FDS) Slip
- Used for recurrent or persistent triggering after A1 pulley release.
- Typically involves releasing the ulnar slip of the FDS tendon.
Complications of Surgery
- Nerve Injury: Radial digital nerve injury, especially in thumb surgeries.
- Bowstringing: Caused by damage to the A2 or A4 pulleys, requiring potential reconstruction.
- Other Risks: Wound dehiscence, scar tenderness, stiffness, or tendon scoring (more common with percutaneous techniques).
Postoperative Care
- Early Mobilisation: Encouraged to prevent stiffness and improve recovery.
- Pain Management: NSAIDs or analgesics are prescribed to manage postoperative pain.
- Physical Therapy: May be recommended for patients with postoperative stiffness or functional limitations.
Conclusion
1. Definition of Trigger Finger: Trigger finger involves the entrapment of the flexor tendon at the A1 pulley, causing painful locking during finger movement.
2. Risk Factors of Trigger Finger: Common in adults 40-60 years old, especially in those with diabetes or engaging in repetitive hand use.
3. Anatomy and Pathology of Trigger Finger: The condition stems from thickening of the A1 pulley and formation of tendon nodules, which disrupt normal tendon gliding.
4. Symptoms of Trigger Finger: Presents with finger stiffness, pain at the base of the finger, and a palpable nodule, often accompanied by a clicking or locking sensation.
5. Diagnosis and Grading of Trigger Finger: Diagnosed through clinical examination and supported by X-ray. Severity is graded from mild discomfort to severe locking requiring intervention.
6. Management of Trigger Finger: Treatment ranges from splinting and NSAIDs to corticosteroid injections for mild cases, with surgical release of the A1 pulley reserved for severe or refractory cases.
Further Reading
- Baumgarten, K. M., Gerlach, D., & Boyer, M. I. (2007). Corticosteroid injection in diabetic patients with trigger finger. The Journal of Bone and Joint Surgery, 89(12), 2604-2611.
- Cebesoy, O., Karakurum, G., Payzın, B., & Baltacı, E. T. (2007). Percutaneous release of the trigger thumb: Is it safe, cheap, and effective? International Orthopaedics, 31(3), 345-349.
- Makkouk, A. H., Oetgen, M. E., Swigart, C. R., & Dodds, S. D. (2008). Trigger finger: Etiology, evaluation, and treatment. Current Reviews in Musculoskeletal Medicine, 1(2), 92-96.
- Saldana, M. J. (2001). Trigger digits: Diagnosis and treatment. The Journal of the American Academy of Orthopaedic Surgeons, 9(4), 246-252.
- Vasiliadis, Angelo V., and Iraklis Itsiopoulos. "Trigger finger: an atraumatic medical phenomenon." The Journal of Hand Surgery (Asian-Pacific Volume) 22.02 (2017): 188-193.
- Zafonte, Brian, Dora Rendulic, and Robert M. Szabo. "Flexor pulley system: anatomy, injury, and management." The Journal of Hand Surgery 39.12 (2014): 2525-2532.
- Brozovich, Nikolas, Devandra Agrawal, and Gangadasu Reddy. "A critical appraisal of adult trigger finger: pathophysiology, treatment, and future outlook." Plastic and Reconstructive Surgery–Global Open 7.8 (2019): e2360.
- Schuind, Frédéric A., Fabian Moungondo, and Pierre Van Wetter. "A new clinical sign of lumbrical plus finger." The Journal of hand surgery 43.6 (2018): 573-e1.
- Dala-Ali, Benan M., et al. "The efficacy of steroid injection in the treatment of trigger finger." Clinics in Orthopedic Surgery 4.4 (2012): 263-268.
- Gil, Joseph A., Andrew M. Hresko, and Arnold-Peter C. Weiss. "Current concepts in the management of trigger finger in adults." JAAOS-Journal of the American Academy of Orthopaedic Surgeons 28.15 (2020): e642-e650.


