Summary Card
Overview
Burn size, expressed as total body surface area (TBSA%), is a cornerstone of burn assessment — influencing decisions from triage to rehabilitation
Lund and Browder Burn Chart
The Lund and Browder Chart is the gold standard for calculating burn surface area. It accounts for anatomical differences across age groups and provides the most accurate TBSA% estimate.
Wallace Rule of Nines
The Wallace Rule of Nines estimates burn surface area by dividing the body into regions of 9%. While efficient and widely used, it lacks precision in pediatric and obese populations.
Palmar Method
The Palmar Method estimates burn size using the patient’s palm as a reference point, making it a practical tool for assessing small or scattered burns.
Mortality Score
Several scoring systems exist to predict burn mortality, but the revised Baux score is the most clinically reliable — incorporating age, TBSA%, and inhalation injury to assess prognosis.
Special Considerations
While TBSA estimation methods are widely used, specific populations and burn types require individualized clinical consideration to ensure accurate assessment and appropriate management.
Updated by: Dr Waruguru Wanjau, Educational Fellow.
Verified by thePlasticsFella ✅
Overview of TBSA Burn Calculations
Burn size, expressed as total body surface area (TBSA%), is a cornerstone of burn assessment — influencing decisions from triage to rehabilitation
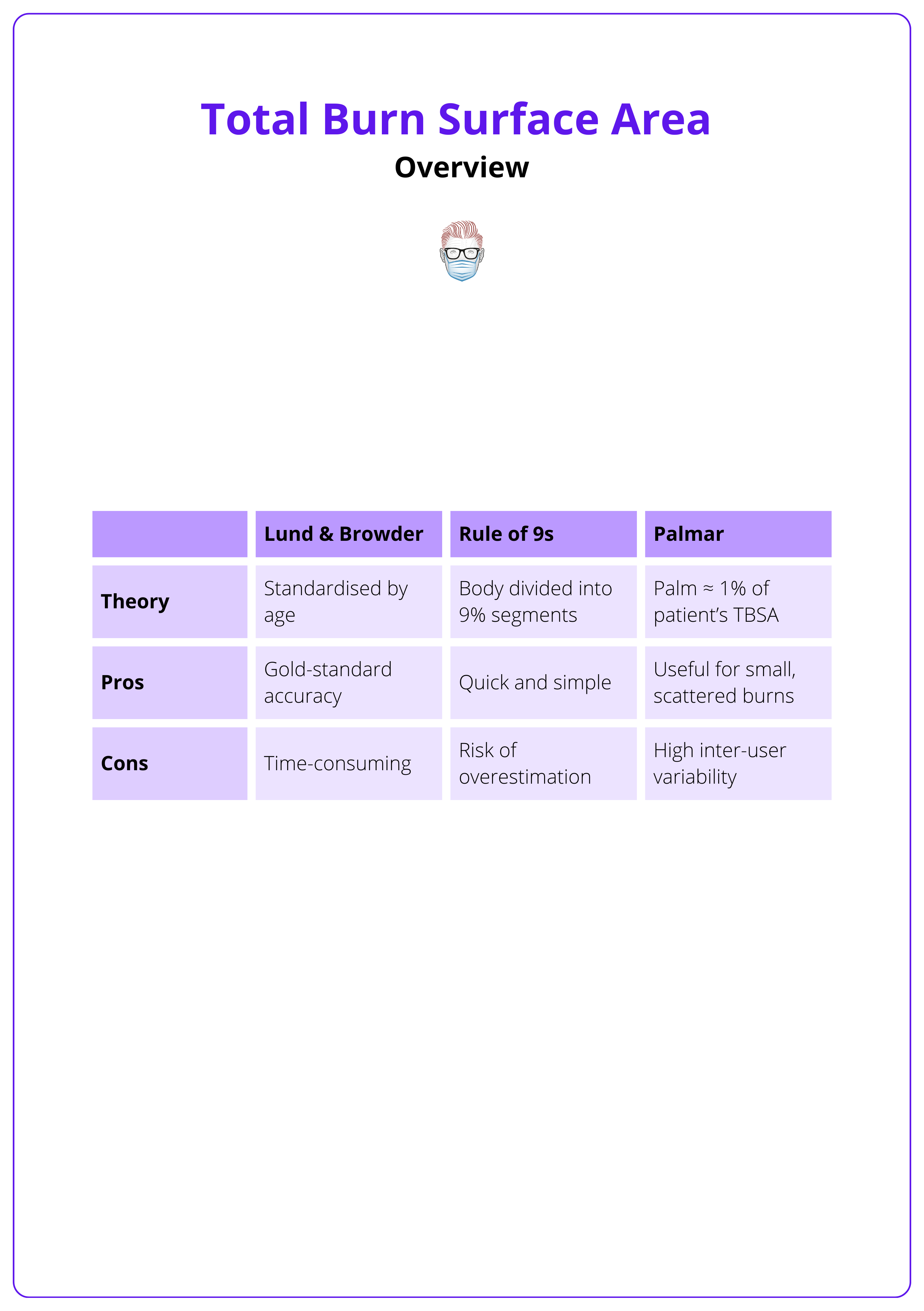
The extent of a burn (particularly its size) directly impacts mortality, functional outcomes, and treatment strategy (Pham, 2019). Three primary methods are used to estimate burn surface area.
- Lund & Browder Chart: Age-adjusted for proportional differences in body surface area.
- Rule of Nines: Simplified method of dividing the body into 9% regions.
- Palmar Method: The patient's palm (including fingers) ≈ 1% TBSA, useful for small or patchy burns.
Accurate estimation of burn TBSA is essential in modern burn care. However, variability between assessors can lead to overestimation and significant differences in measurements (Chan, 2011).
- Fluid Resuscitation: Guides volume calculations in the acute phase.
- Triage & Transfers: Determines need for burn center referral.
- Nutritional and Metabolic Support: Correlates with hypermetabolic demand.
- Length of Stay & Rehabilitation Planning: Predicts care trajectory and intensity.
This table provides an overview of the different methods for TBSA calculation.
Modern tools like 3D imaging, mobile apps, and AI offer improved precision, but adoption is limited by cost, training gaps, and workflow integration (Chong, 2020). As a result, most clinical settings still rely on manual methods, particularly in acute care.
Common burn assessment methods should be used cautiously in obese adult patients, with clinical parameters monitored even more closely (Borhani- Khomani, 2017).
Lund and Browder Burn Chart
The Lund and Browder Chart is the gold standard for calculating burn surface area. It accounts for anatomical differences across age groups and provides the most accurate TBSA% estimates for both adults and children.
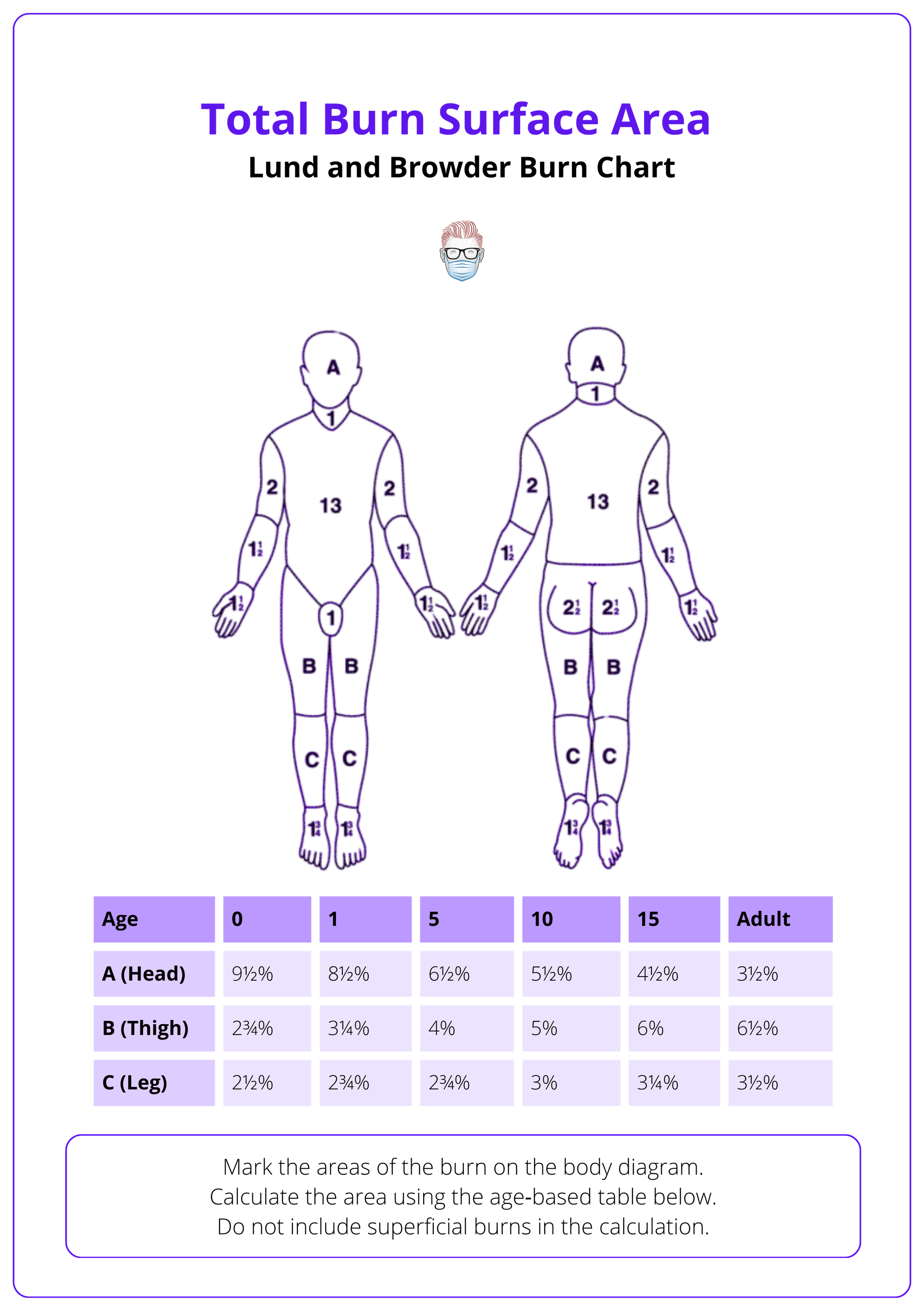
First introduced by Lund and Browder in 1944, this chart revolutionized burn assessment by dividing the body into 12 anatomical regions and incorporating an age-correction factor for pediatric patients (Lund & Browder, 1994). Building on Samuel Berkow’s earlier formula and Boyd’s 1935 data, it remains one of the most historically significant yet clinically relevant burn assessment tools.
Today's updated version has expanded to 19 regions, providing greater precision (Hampe, 2017), and can be used in the following manner.
- Visual Mapping: Providers outline burned areas on a printed diagram.
- Age-Based Reference: Each region’s TBSA% is adjusted according to patient age, particularly in the head, thighs, and legs — the only regions that change with growth (Hampe, 2017).
- Burn Depth Inclusion: The chart distinguishes between partial-thickness and full-thickness burns. Superficial burns are excluded from TBSA% calculations.
The image below illustrates the Lund and Browder chart used for calculating TBSA% in burns.
Advantages
- High Accuracy: Considered more precise than Rule of Nines, especially in pediatric patients (Wallace, 1951).
- Pediatric Adaptability: Head is a larger percentage in infants; leg regions compensate proportionally.
- Standard in Practice: Widely used in emergency departments and burn centers (American Burn Association, 2020).
- Evidence-Based: Based on BSA data applicable to 99.9% of the population (Boyd, 1935).
Limitations
- Time-Intensive: Slower to apply than simplified methods.
- Reference Dependent: Requires printed chart and familiarity with scoring technique.
- Obesity Considerations: Not designed to account for variations in body habitus seen in obese patients (Tapking, 2019; Neaman, 2011).
- Landmark Challenges: Lateral burns are harder to assess due to a lack of anatomical guidance.
- Depth Judgement Required: Accurate scoring depends on clinical expertise in assessing burn depth.
The Lund-Browder chart has recently been validated in the modern, more obese pediatric population (Rumpf, 2018).
Wallace Rule of Nines
The Wallace Rule of Nines estimates burn surface area by dividing the body into regions of 9%. While efficient and widely used, it lacks precision in pediatric and obese populations.
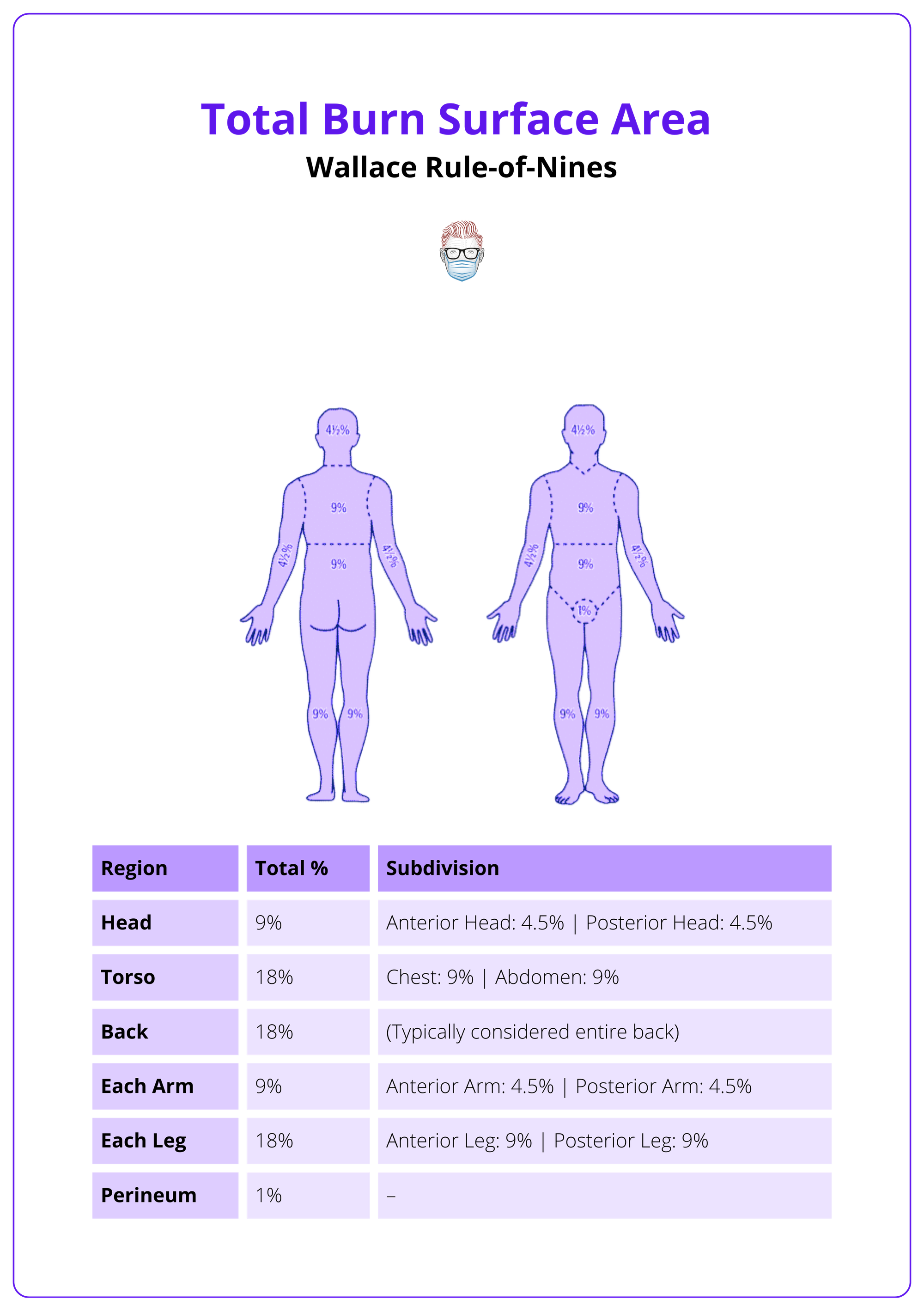
The Rule of Nines, first described by Pulaski and Tennison in 1947 and popularized by Wallace in 1951, remains widely used for emergency burn assessment due to its speed, simplicity, and accuracy (Tocco-Tussardi, 2018; Cheah, 2018). It primarily functions as a rapid screening tool to estimate the extent of partial- and full-thickness burns quickly for initial treatment guidance.
Key points include,
- Not Definitive: After initial stabilization, clinicians should use more detailed methods, such as the Lund and Browder Chart, for comprehensive burn care planning (Giretzlehner, 2025).
- Effective in Mass Casualties and Prehospital Settings: Valuable for rapid triage because it is easy to memorize and apply quickly (Giretzlehner, 2025).
- Excludes Superficial Burns: Includes only partial- and full-thickness injuries, enhancing clinical accuracy and decision-making.
The correct calculation of the Rule of 9's is visualised below.
Advantages
- Efficient: Ideal for rapid estimation in high-pressure settings like field triage or emergency departments (Wallace, 1951).
- Reduces Underestimation: Tends to overestimate slightly, which is safer when calculating initial resuscitation needs (Watchel, 2000).
- Minimal Training Required: Quickly understood and applied by most healthcare providers.
Limitations
- Lacks Precision in Key Populations: Not recommended for children under 12 years due to inaccurate body proportion representation (Lee, 2025).
- Not Obesity-Adjusted: Poorly reflects surface area distribution in obese or very muscular patients (Tapking, 2019).
- Overestimation Risk: Especially for smaller burns or when used by less experienced providers (Wachtel, 2000).
The "Rule of Eights" provides a more accurate TBSA burn estimation for infants weighing less than 10 kg, assigning approximately 32% to the trunk, 20% to the head, 16% to each leg, and 8% to each arm (Moore, 2024).
Palmar Method
The Palmar Method estimates burn size using the patient’s palm as a reference point, making it a practical tool for assessing small or scattered burns.
The Palmar Method is the simplest and most accessible way to estimate Total Body Surface Area (TBSA) in burn patients. It relies on the patient’s own palm, including digits, as a reference — typically representing about 1% of their TBSA. This method is especially useful when burns are irregularly distributed or when other tools are unavailable.
NICE guidelines recommend using the palm, including digits for estimating small or patchy burns. However, the exact percentage can vary based on body habitus, age, and whether digits are included.
- Palm + Digits ≈ 1% TBSA
- Palm only (no fingers) ≈ 0.5% TBSA
Advantages
- Quick and Requires No Tools: Useful in prehospital settings or when resources are limited (Carrougher, 2024).
- Ideal for Scattered or Localized Burns: Offers flexibility when assessing non-contiguous burn areas.
- Simple for Patient Involvement: Easy to explain and demonstrate for patient education.
Limitations
- Not Accurate for Large Burns: Accumulated errors increase as burn size increases.
- Subject to Variability: Palm size differs between individuals, especially in children, making estimates less reliable (Pham, 2019).
- No Burn Depth Consideration: This method doesn’t distinguish between burn types (e.g., superficial vs full-thickness).
Mortality Score in Burns Patients
Several scoring systems exist to predict burn mortality, but the revised Baux score is the most clinically reliable — incorporating age, TBSA%, and inhalation injury to assess prognosis.
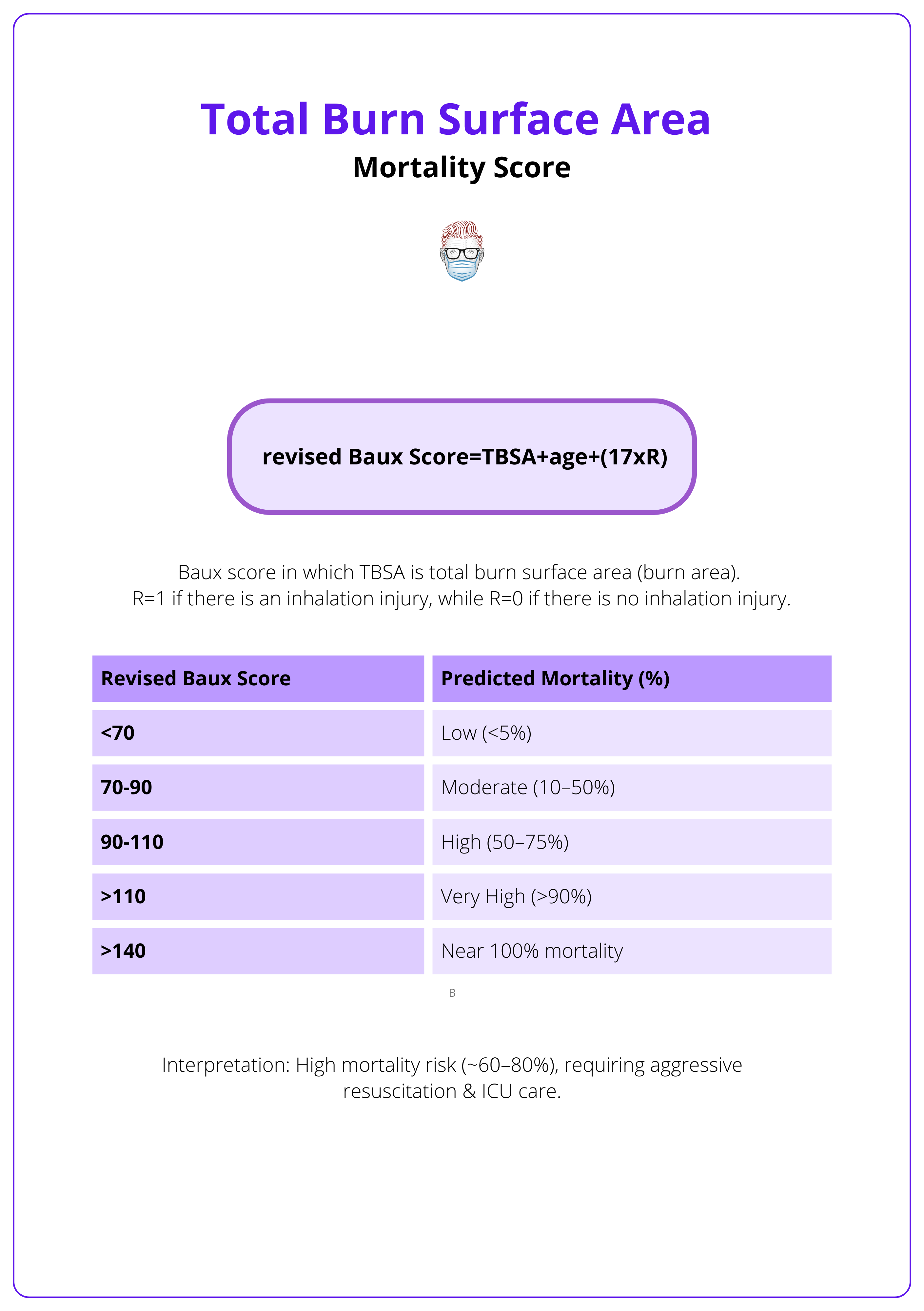
Mortality prediction tools help assess burn severity, guide treatment, and inform prognosis. Among various models (ABSI, Ryan, Smith, McGwin, BOBI, FLAMES, APACHE II), the Revised Baux Score and ABSI are most commonly used. Studies suggest the Revised Baux Score is more accurate and practical in contemporary burn care (Halgas, 2018; Edgar, 2023; Lip, 2018).
Revised Baux Score
Revised Baux Score = Age + TBSA (%) + 17 (if inhalation injury is present). This scoring system provides a rapid severity assessment, predicts mortality risk, and supports clinical decision-making. It uses three key clinical factors.
- Age: Mortality risk increases with patient age.
- TBSA (%): Greater burn surface area correlates with poorer outcomes.
- Inhalation Injury: Airway involvement significantly elevates the mortality risk.
Revised Baux score is summarised in the image below.
Limitations
- Oversimplified: Does not account for comorbidities, frailty, or modern care improvements.
- Overestimation Risk: May overpredict mortality in centers with advanced burn care.
- Less Accurate at Extremes: Performance decreases in very young or very old patients (Edgar, 2023).
The Baux equation has a diminished ability to predict mortality risk when applied to patients at both extremes of age (Edgar, 2023).
Special Considerations
While TBSA estimation methods are widely used, specific populations and burn types — such as pediatric, obese, circumferential, electrical, and chemical burns — require individualized clinical consideration to ensure accurate assessment and appropriate management.
Standard burn estimation techniques like the Rule of Nines, Lund-Browder Chart, and Palmar Method are based on assumptions of average body proportions. However, factors such as age, BMI, burn depth, and distribution can significantly impact accuracy.
Pediatric Patients
- Proportional Differences: Children have proportionally larger heads and smaller limbs, impacting TBSA estimates (Lund & Browder, 1944; Meeh, 1879; Rumpf, 2018).
- Preferred Tools: Use the Lund-Browder chart or Pediatric Rule of Nines — the latter assigns 18% to the head and 14% to each leg in infants (American Burn Association, 2023).
- Common Pitfall: Errors are often due to incorrect application, not the reference values themselves (Rumpf, 2018).
- Educational Support: Pediatric burn estimation is emphasized in global training programs like ABLS, Interburns, and EMSB (Interburns, 2025; ANZBA, 2023).
Obese and Morbidly Obese Patients
- Inaccurate Surface Area Distribution: Higher BMI alters skin surface proportions — typically underestimating trunk and overestimating limbs (Borhani- Khomani 2017; Neaman, 2011).
- Proposed Adjustments: Head: 5%, Arms: 15%, with trunk and leg proportions adjusted by BMI category (Neaman, 2011).
- Alternate Systems: The Rule of Sevens, developed by Williams and Wohlgemuth, proposes more accurate TBSA percentages for obese patients (Williams, 2013).
- Gender Considerations: Burn size involving the breasts in women can be underestimated; bra cup size may need to be factored into anterior trunk TBSA estimates (Hidvegi, 2004).
Circumferential Burns
- Extremities: Risk of compartment syndrome, potentially requiring escharotomy to restore perfusion.
- Chest Involvement: Can restrict ventilation, necessitating early airway management or chest wall escharotomy.
- Abdominal Burns: May increase intra-abdominal pressure, leading to abdominal compartment syndrome and systemic compromise.
Electrical Burns
- Injury Beyond the Surface: Electrical injuries often cause deep muscle and tissue necrosis, not reflected in TBSA%.
- TBSA Misleading: Surface appearance underestimates true injury severity — advanced imaging and cardiac monitoring are essential.
- Clinical Priority: Early surgical evaluation and compartment pressure monitoring are often warranted.
Chemical Burns
- Severity ≠ Size: Unlike thermal burns, TBSA does not correlate with severity in chemical injuries.
- Assessment Factors: Severity depends on chemical type, concentration, contact time, and penetration depth.
- Immediate Care Focus: Rapid decontamination and pH neutralization take precedence over TBSA measurement.
For extensive burns, calculating unburned areas and subtracting from 100% can improve accuracy — a technique taught in Interburns and EMSB courses (Interburns, 2025; ANZBA, 2023).
Conclusion
1. Overview: TBSA% is critical in burn care — influencing resuscitation, referrals, nutrition, and rehab planning.
2. Lund and Browder Chart: Gold standard TBSA tool; adjusts for age-based anatomical differences, offering high accuracy.
3. Rule of Nines: Quick and easy; divides the body into 9% segments but lacks precision in kids and obese patients.
4. Palmar Method: Uses the patient’s palm (≈1% TBSA) for small, scattered burns — ideal when tools aren’t available.
5. Mortality Score (Revised Baux): Adds age + TBSA + 17 (if inhalation injury) to predict burn mortality; simple but less accurate in extremes.
6. Special Considerations: Children, obese patients, and electrical or chemical burns require tailored TBSA assessment strategies.
Further Reading
- Miller S, Bessey P, Schurr M, et al. National Burn Repository 2005: a ten-year review. J Burn Care Res. 2006;27(4):411-436. doi:10.1097/01.BCR.0000226260.17523.22
- Chan QE, Barzi F, Cheney L, Harvey JG, Holland AJ. Burn size estimation in children: Still a problem. Emergency Medicine Australasia. November 2011:181-186. doi:10.1111/j.1742-6723.2011.01511.x
- Lund C, Browder NC. The estimation of areas of burns. Surg Gynecol Obstet . 1944:79:352–8. https://scholar.google.com/scholar?cluster=4671664022958447735&hl=en&as_sdt=0,5.
- Wachtel TL, Berry CC, Wachtel EE, Frank HA. The inter-rater reliability of estimating the size of burns from various burn area chart drawings. Burns. March 2000:156-170. doi:10.1016/s0305-4179(99)00047-9
- WALLACE A. The exposure treatment of burns. Lancet. 1951;1(6653):501-504. doi:10.1016/s0140-6736(51)91975-7
- Tocco-Tussardi I, Presman B, Huss F. Want Correct Percentage of TBSA Burned? Let a Layman Do the Assessment. J Burn Care Res. 2018;39(2):295-301. doi:10.1097/BCR.0000000000000613
- Cheah A, Kangkorn T, Tan E, Loo M, Chong S. The validation study on a three-dimensional burn estimation smart-phone application: accurate, free and fast? Burns Trauma. 2018;6:7. doi:10.1186/s41038-018-0109-0
- Moore R, Waheed A, Burns B. statpearls. February 2024. http://www.ncbi.nlm.nih.gov/books/NBK513287/.
- Jose RM, Roy DK, Vidyadharan R, Erdmann M. Burns area estimation—an error perpetuated. Burns. August 2004:481-482. doi:10.1016/j.burns.2004.01.019
- Kamolz L, Lumenta D, Parvizi D, et al. Smartphones and burn size estimation: “Rapid Burn Assessor”. Ann Burns Fire Disasters. 2014;27(2):101-104. https://www.ncbi.nlm.nih.gov/pubmed/26170784.
- Pham C, Collier Z, Gillenwater J. Changing the Way We Think About Burn Size Estimation. J Burn Care Res. 2019 Jan 1;40(1):1-11. doi: 10.1093/jbcr/iry050. PMID: 30247559.
- Rumpf RW, Stewart WCL, Martinez SK, Gerrard CY, Adolphi NL, Thakkar R, Coleman A, Rajab A, Ray WC, Fabia R. Comparison of the Lund and Browder table to computed tomography scan three-dimensional surface area measurement for a pediatric cohort. J Surg Res. 2018 Jan;221:275-284. doi: 10.1016/j.jss.2017.08.019. Epub 2017 Oct 5. PMID: 29229139.
- Borhani-Khomani K, Partoft S, Holmgaard R. Assessment of burn size in obese adults; a literature review. J Plast Surg Hand Surg. 2017 Dec;51(6):375-380. doi: 10.1080/2000656X.2017.1310732. Epub 2017 Apr 18. PMID: 28417654.
- Chong HP, Quinn L, Jeeves A, Cooksey R, Lodge M, Carney B, Molony D. A comparison study of methods for estimation of a burn surface area: Lund and Browder, e-burn and Mersey Burns. Burns. 2020 Mar;46(2):483-489. doi: 10.1016/j.burns.2019.08.014. Epub 2019 Sep 24. PMID: 31561927.
- Edgar MC, Bond SM, Jiang SH, Scharf IM, Bejarano G, Vrouwe SQ. The Revised Baux Score as a Predictor of Burn Mortality: A Systematic Review and Meta-Analysis. J Burn Care Res. 2023 Nov 2;44(6):1278-1288. doi: 10.1093/jbcr/irad075. PMID: 37220881.
- Halgas B, Bay C, Foster K. A comparison of injury scoring systems in predicting burn mortality. Ann Burns Fire Disasters. 2018 Jun 30;31(2):89-93. PMID: 30374258; PMCID: PMC6199008.
- Lip HTC, Idris MAM, Imran FH, Azmah TN, Huei TJ, Thomas M. Predictors of mortality and validation of burn mortality prognostic scores in a Malaysian burns intensive care unit. BMC Emerg Med. 2019 Nov 7;19(1):66. doi: 10.1186/s12873-019-0284-8. PMID: 31699024; PMCID: PMC6839226.
- Carrougher, G.J. and Pham, T.N., 2024. Burn size estimation: A remarkable history with clinical practice implications. Burns Open, 8(2), pp.47-52.


