Summary Card
Tissue expansion optimises the viscoelastic properties of skin and increases tissue availability through a process of creep and stress relaxation. Creep can be mechanical (acute) and biological (chronic).
During the tissue expansion, histological changes occur. The epidermis is the only anatomical layer that increases in thickness.
Tissue expanders are designed in different shapes, sizes, textures and expansion directions to fit their specific indication. Four zones or layers form a capsule around the expander.
Tissue expanders are not used in a radiated wound bed, under a skin graft or in a wound with an active infection.
Definition of Tissue Expansion
Tissue expansion increases soft tissue availability by optimising the skin's viscoelastic properties. Architectural and histological changes occur to the skin, subcutaneous tissue & blood supply through mechanical creep, biological creep and stress relaxation.
Neuman first described it in 1957.
Mechanism of Tissue Expansion
Key Point
Tissue expansion optimises the viscoelastic properties of soft tissue through 3 processes: mechanical creep, biological creep and stress relaxation.
Tissue expansion is a time-dependent process of stretch (mechanical creep), growth (biological creep) and strain (stress relaxation). Each process has an essential role in acute and chronic optimisation of the viscoelastic properties of soft tissue.
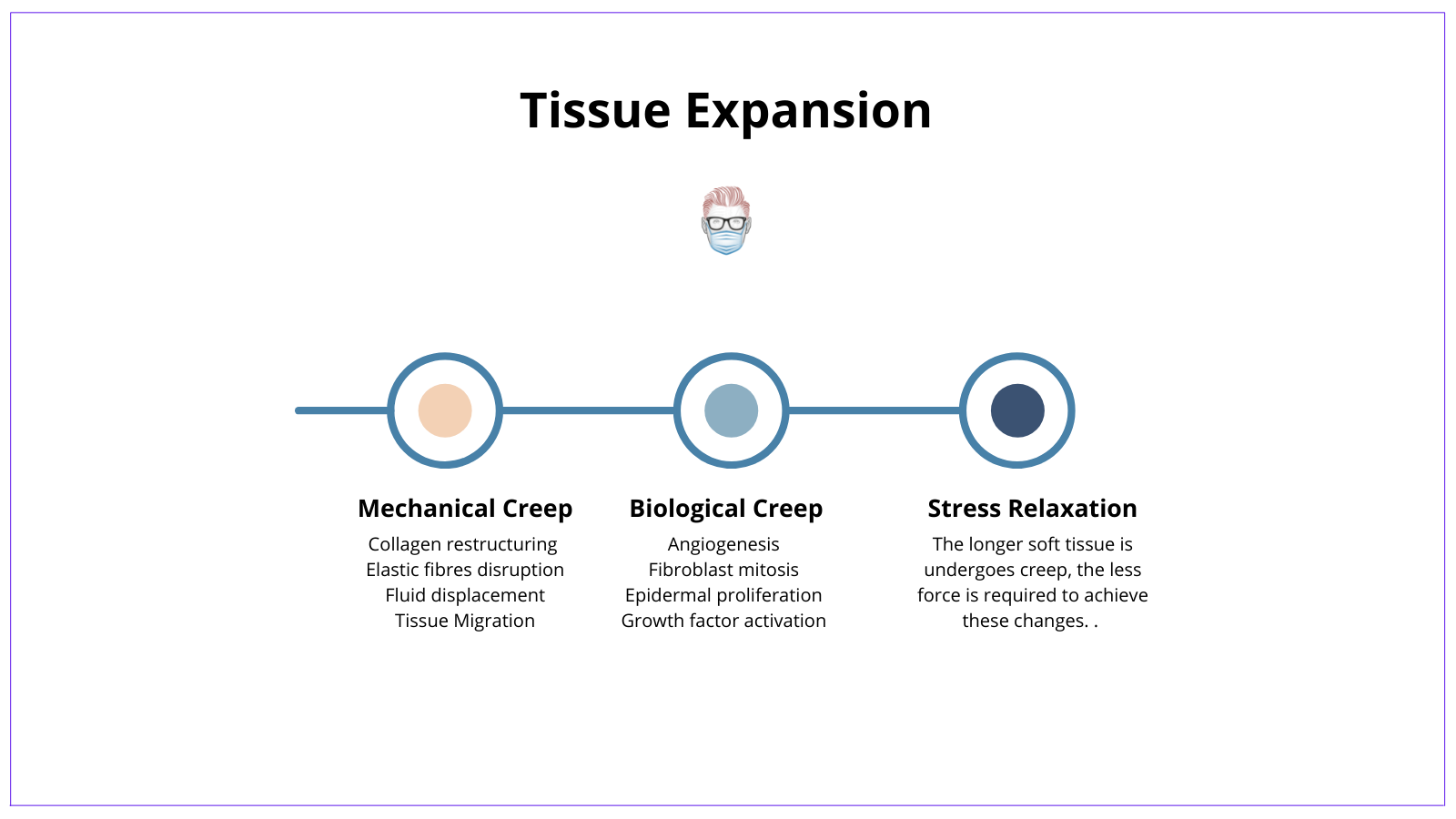
Mechanical Creep
Mechanical creep occurs in the acute phases of mechanical stress, often seen in intra-operative tissue expansion.
It results in the majority of soft tissue gain via:
- Collagen restructuring: fibres align parallel to each other & the vector force
- Elastic fibres disruption: microfragmenting
- Fluid displacement: water displaced from the ground substance
- Tissue Migration: recruitment of nearby tissue into the expanded field.
Biological Creep
Biological creep occurs in the chronic phase of mechanical stress and results in growth.
Cellular growth and tissue regeneration occur via:
- Angiogenesis
- Fibroblast mitosis
- Epidermal proliferation
- Growth factor activation
Stress Relaxation
The longer soft tissue undergoes mechanical and biological creep, the less force is required to achieve these changes. As the name suggests, stress relaxes.
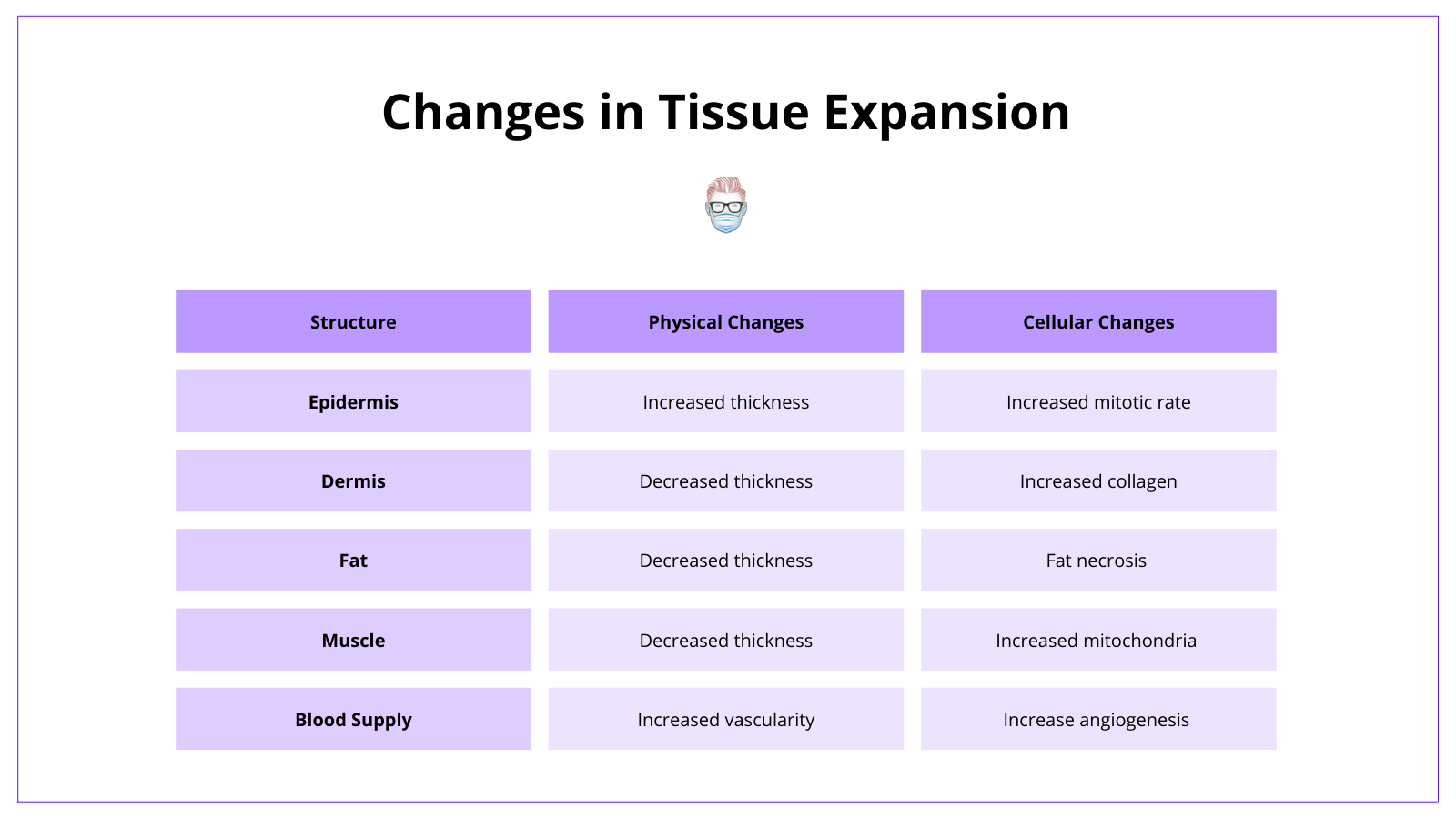
Changes in Tissue Expansion
Key Point
Tissue expansion results in histological and architectural changes to soft tissue over time.
Tissue expansion results in physical and cellular changes to soft tissue structures. These changes are detailed below.
- Epidermis: increased mitotic rate of the basal layer, increased thickness.
- Dermis: decreased thickness, increased collagen fibres & realignment.
- Fat: decreases thickness with some fat necrosis
- Muscle: decreased thickness, function not affected.
- Blood supply: increased angiogenesis (like delay phenomenon)
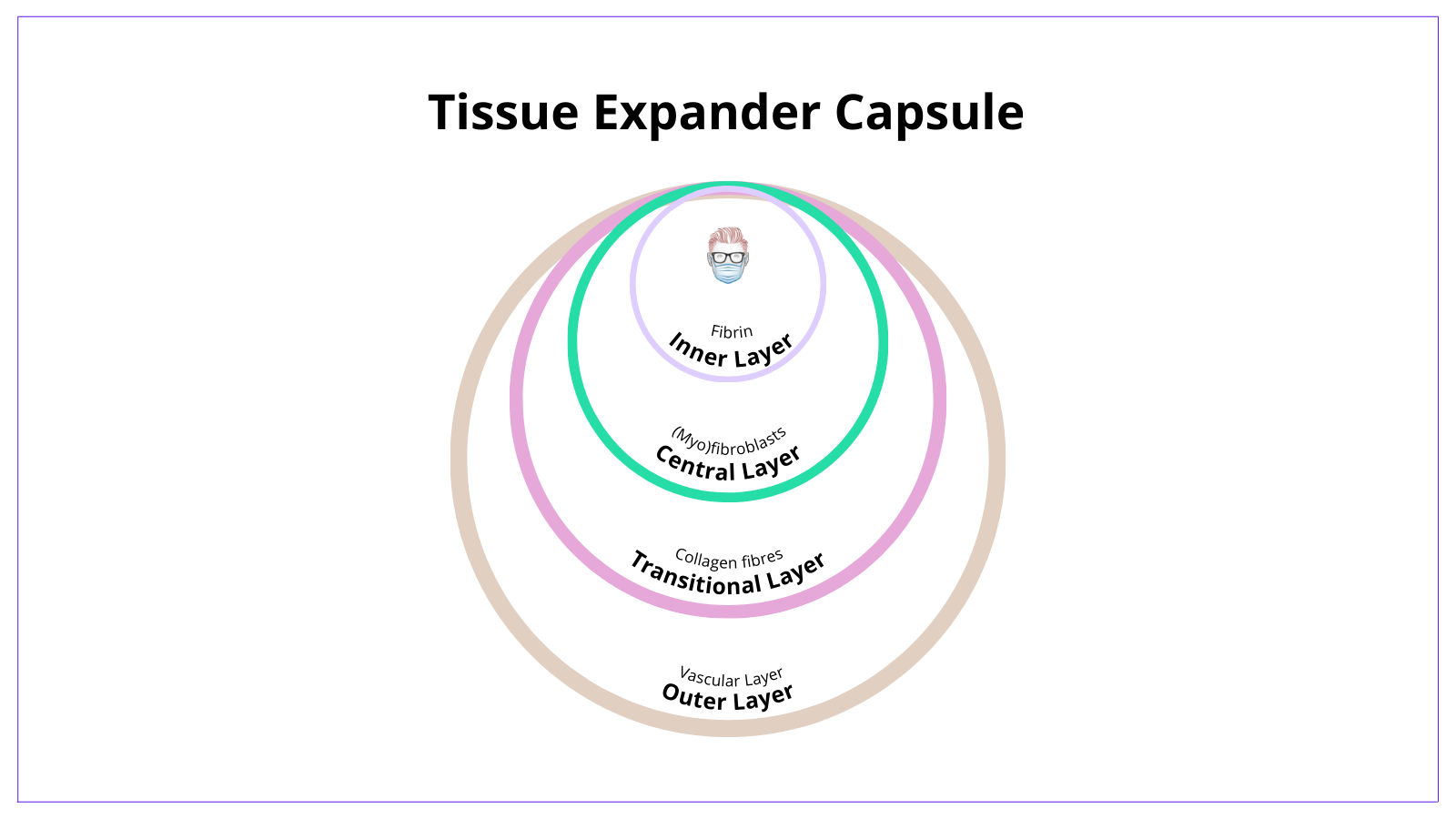
Capsule Formation
Key Point
After insertion, a capsule forms around the tissue expander. This has been shown to develop in 4 layers of different cellular structures.
A capsule forms around a tissue expander after being inserted in a short period. This capsule is a collection of collagen, myofibroblasts and fibroblasts structured into 4 layers, as described by Pasyk.
- Inner Layer: a synovial fibrin lining that contains macrophages.
- Central Layer: elongated fibroblasts & myofibroblasts
- Transitional Layer: collagen fibres
- Outer layer: a vascular layer with collagen fibres.
These layers can be visualised in the image below.
Types of Tissue Expanders
Key Point
Tissue expanders vary in size, shape, direction of expansion, port location and function. These variations reflect the specific use of indication of that tissue expander.
A tissue expander is an inflatable silicone reservoir. There are different types of tissue expanders based on their specific purposes. The main variables relate to the tissue expander port, texture, base, shape and function.
Port Location
There are two commonly used ports: integrated and remote ports. Their main differences are in their location and their risk profile.
Integrated
- This is part of the tissue expander and is incorporated into the shell.
- It is often located by a magnetic finder.
- Benefit: no subcutaneous tunnelling or separate port site required.
- Risks: could potentially puncture the tissue expander with a needle.
Remote
- They are not directly incorporated into the shell but rather via a tube
- The port is often palpable in the subcutaneous tissue (or externally)
- Benefit: unlikely to puncture the expander with the needle on expansion
- Risks: the tunnel connecting the port and expander can become kinked, or the port can flip over in the subcutaneous tissue.
Shape, Size & Base
Tissue expanders are designed in various shapes and sizes, for example, oval, rectangular, round or square (or even custom). The expected tissue expansion gain is the essential point relating to shape and size differences.
- Round expanders increase surface area by ~25% (often used in the breast)
- Crescentic increases surface area ~ 33% (often used on the scalp)
- Rectangular expanders increase surface area by ~ 40%.
The base always has an important role. It should be 2.5 x the diameter of the defect needed to be reconstructed or covered.
- Solid base: unidirectional expansion
- Soft base: omnidirectional expansion
Volume is a less defining feature because the expanders can often be overinflated.
Thickness Variations
A tissue expander can have variations in thickness and compliance. This is specifically designed to allow differential expansion based on the desired preferences. For example, breast tissue expansion to maintain a ptotic appearance.
Differential expansion can be described in two ways
- Isotropic: expand in any direction
- Anisotropic: expand in controlled directions
Surface
A tissue expander can have a smooth or textured surface (just like a breast implant). A textured implant has reduced rates of contracture and migration.
Clinical Application of Tissue Expanders
Key Point
Tissue expansion can be used for a diverse group of reasons. It is commonly used in delayed breast reconstruction. It should not be used in wounds with a high risk of wound breakdown.
Indications
Tissue expansion has a diverse range of indications in most body parts. Their insertion, location and design technique can be adjusted for specific purposes. Examples are detailed below.
Scalp Expansion
- It can be used for male pattern baldness and tissue defects requiring reconstruction.
- An expander is inserted into a subgaleal position.
- If performing an advancement flap reconstruction, the amount of tissue available for advancementequals the circumference minus the base width of the expander.
Face Expansion
- It can be inserted post-auricular for ear reconstructions or on the forehead for flaps.
- Based on the facial subunit principle.
Breast Expansion
- A widespread application for delayed or immediate-delayed breast reconstruction
- Subpectoral insertion with integrated port or remote port.
Contraindications
There are some instances where tissue expansion should not be used. This is a case-by-case basis and is often related to the wound bed and healing ability. Examples are listed below.
- Radiated wound bed
- Inserted under a skin graft
- Active infection
- Poorly healed scar
Flashcards
They are continually updated and are for thePlasticsPro users.
This is for thePlasticsPro
Join the Club to enjoy unlimited access to all of thePlasticsFella.
Join the Club

