Summary Card
Definition
Thoracic outlet syndrome (TOS) is the compression of neurovascular structures at the brachial plexus, caused by soft tissue or bony anomalies.
Anatomy
Compression of neurovascular structures at the brachial plexus occurs in three key areas: the interscalene triangle, costoclavicular space, and subcoracoid space, each with specific boundaries and components.
Aetiology
Thoracic outlet syndrome (TOS) is often caused by compression at the interscalene triangle, costoclavicular, or subcoracoid spaces. Anatomical anomalies, tumors, or trauma are predisposing factors.
Presentation
Neurophysiological testing and imaging (X-rays, CT, MRI) help exclude other compression sites and detect anatomical anomalies; surgical exploration provides a definitive diagnosis.
Investigations
Investigating Thoracic Outlet Syndrome involves neurophysiological tests and imaging to rule out other causes, with surgery as the definitive diagnostic tool.
Management
Thoracic outlet syndrome management involves a multidisciplinary approach: physiotherapy, pain control, occupational therapy, psychology, early anticoagulation for vascular TOS, and surgery.
Primary Contributor: Dr Suzanne Thomson, Educational Fellow.
Reviewer: Dr Kurt Lee Chircop, Educational Fellow.
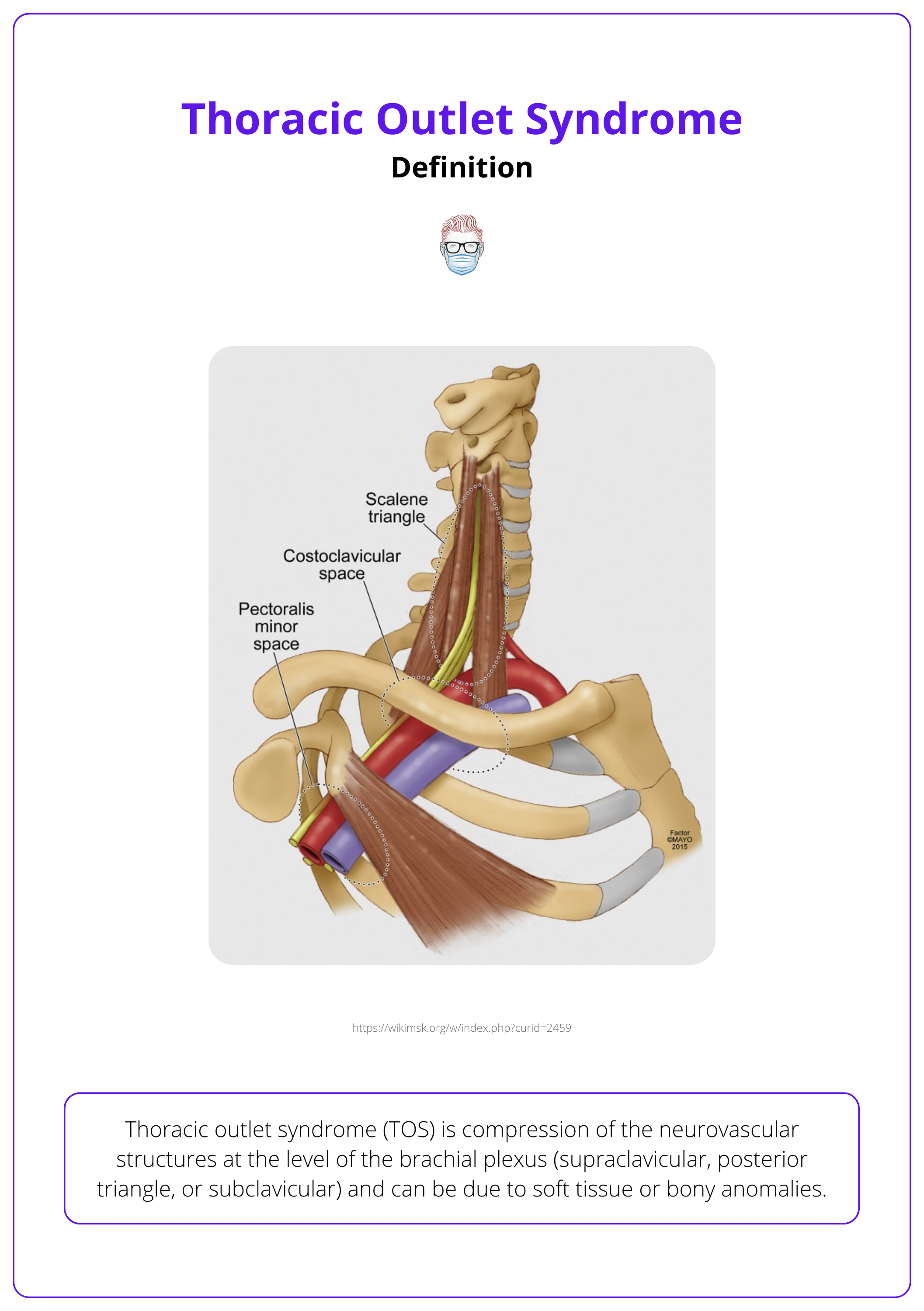
Definition of Thoracic Outlet Syndrome
Thoracic outlet syndrome (TOS) is compression of the neurovascular structures at the level of the brachial plexus (supraclavicular, posterior triangle, or subclavicular) and can be due to soft tissue or bony anomalies.
Thoracic outlet syndrome (TOS) is compression of the neurovascular structures at the level of the brachial plexus due to anatomical features of the brachial plexus and subclavian vessels or fibrous, muscular, or bony anomalies.
It was first described in 1860 by Willshire, attributed to an accessory 1st rib. Now, it is classified into several types:
- Neurogenic: Most common
- Venous: More common than arterial
- Arterial
- or mixed
The image below illustrates the definition and anatomy of thoracic outlet syndrome.
It is relatively uncommon, with an estimated annual incidence of 1-3 cases per 100,000 population (Illig, 2021). Important epidemiological facts are:
- Primarily occurs in adults.
- Vascular compression is commoner in children (Abdalla BA, 2024).
- Slight female predominance, ratio of approximately 3:1.
Neurogenic subtype is more common than vascular, of which venous is more frequent than arterial.
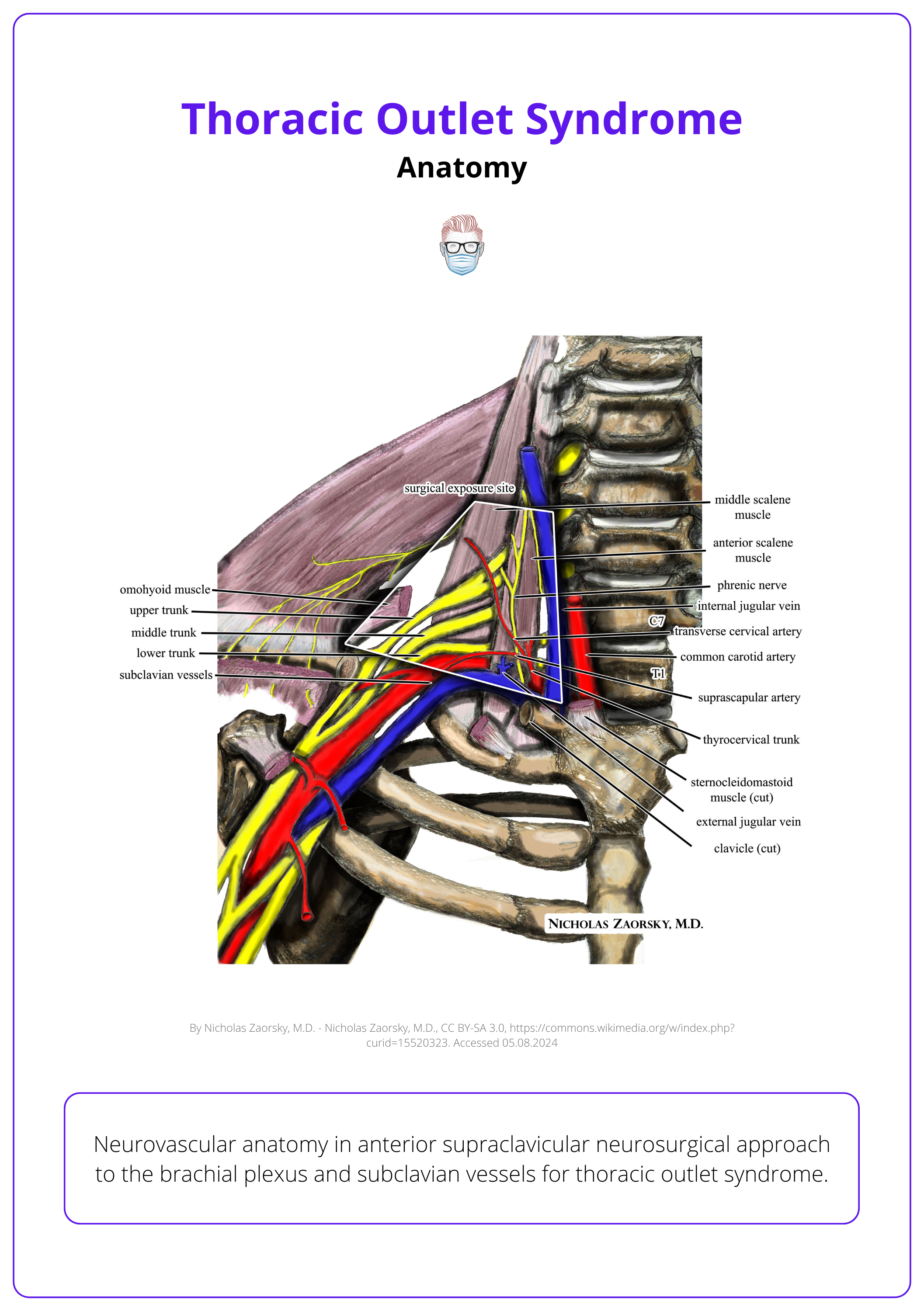
Anatomy of Thoracic Outlet Syndrome
Compression of neurovascular structures at the brachial plexus occurs in three key areas: the interscalene triangle, costoclavicular space, and subcoracoid space, each with specific boundaries and components.
Compression of the neurovascular structures at the level of the brachial plexus can occur at three distinct anatomical locations.
- Interscalene triangle
- Structures: Brachial plexus, subclavian artery, vein runs below anterior scalene
- Boundaries: Scalenus anterior, Scalenus medius, 1st rib
- Costoclavicular space
- Structures: Brachial plexus divisions, subclavian artery and vein
- Boundaries: Clavicle/subclavius, 1st rib, Costoclavicular ligament, Upper border of the scapula
- Subcoracoid space
- Structures: Brachial plexus cords, axillary artery, and vein
- Boundaries: Coracoid, Pectoralis minor, Ribs 2- 4
The image below illustrates the neurovascular anatomy of the thoracic outlet.
Aetiology of Thoracic Outlet Syndrome
Thoracic Outlet Syndrome (TOS) may arise from a variety of factors including anatomical anomalies, neoplasms, and traumatic injuries.
The aetiology of thoracic outlet syndrome can be categorised into anatomical anomalies and pathological factors, such as trauma and tumours.
Anatomical Anomalies
Bone irregularities, muscle variations, and ligament issues all contribute to compression and subsequent thoracic outlet syndrome.
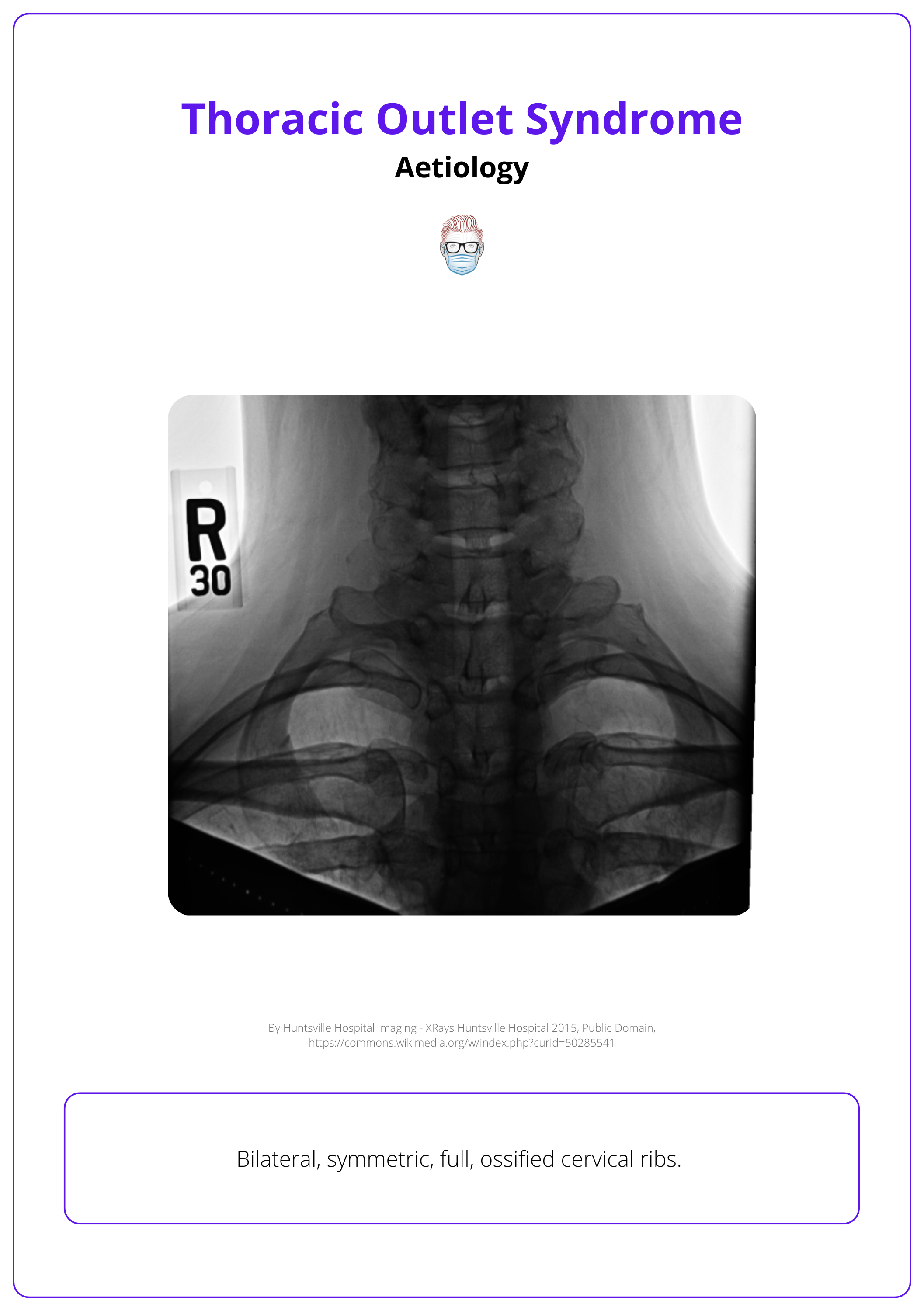
Bone Irregularities:
- Accessory First Rib: Often implicated in congenital anomalies like brachial plexus palsy but usually undetectable on MRI scans.
- Elongated Cervical Vertebrae Processes: These can contribute to compression.
The image below illustrates cervical ribs.
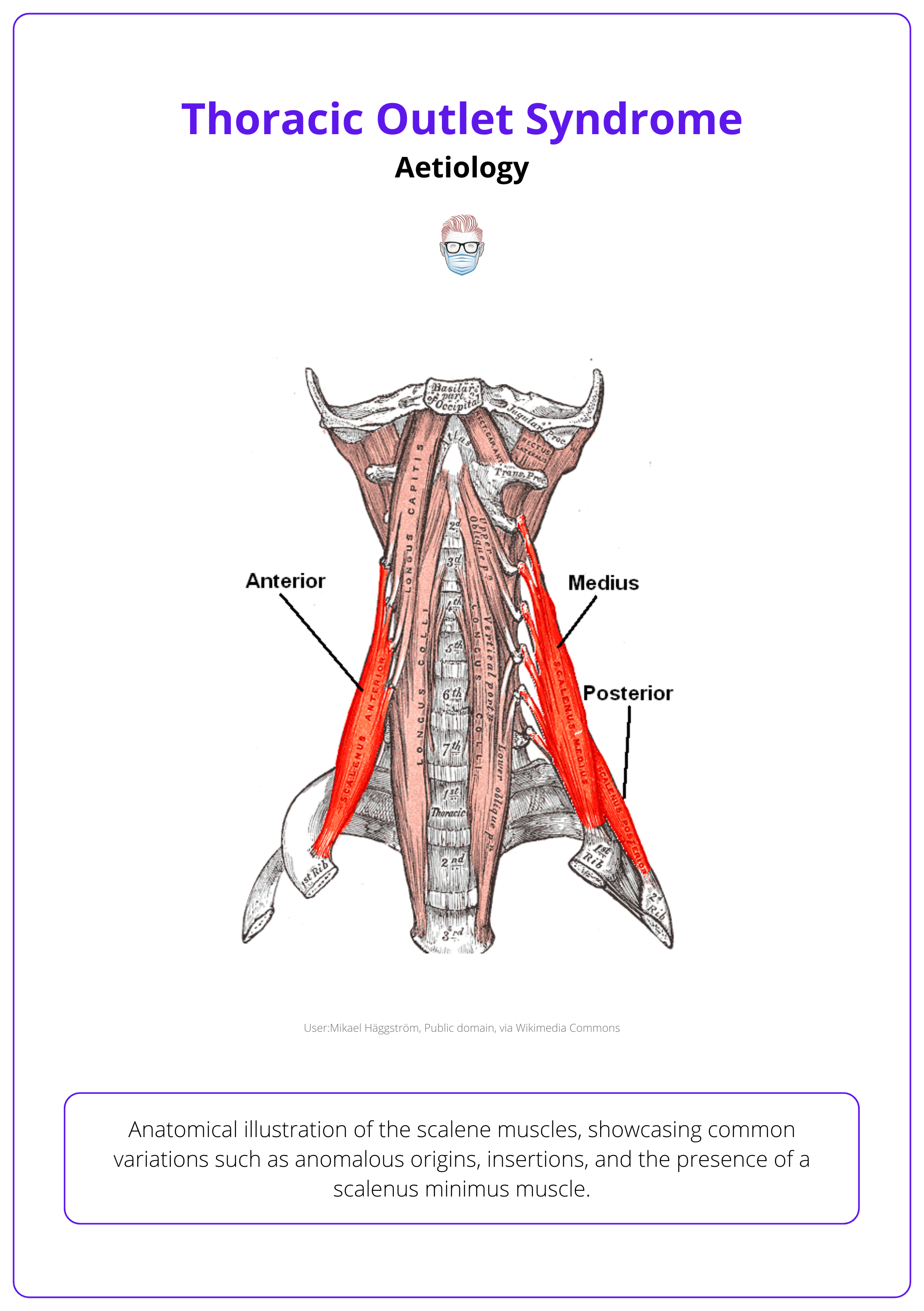
Muscle Variations:
- Scalene Muscle Anomalies: Anomalous origins or insertions and the presence of a scalenus minimus muscle, which originates from cervical transverse processes and attaches to the first rib between the subclavian artery and the T1 nerve root.
- Muscle Hypertrophy: Enlarged scalene or pectoralis minor muscles can intensify compression symptoms.
The image below illustrates the scalene muscles.
Ligament Issues:
- Fibrous Bands: Located between scalene muscles, the first rib, and the clavicle.
- Costoclavicular Ligament: A potential cause of Paget-Schroetter syndrome, a type of venous compression that can lead to subclavian deep vein thrombosis (DVT), especially in athletes.
Pathological
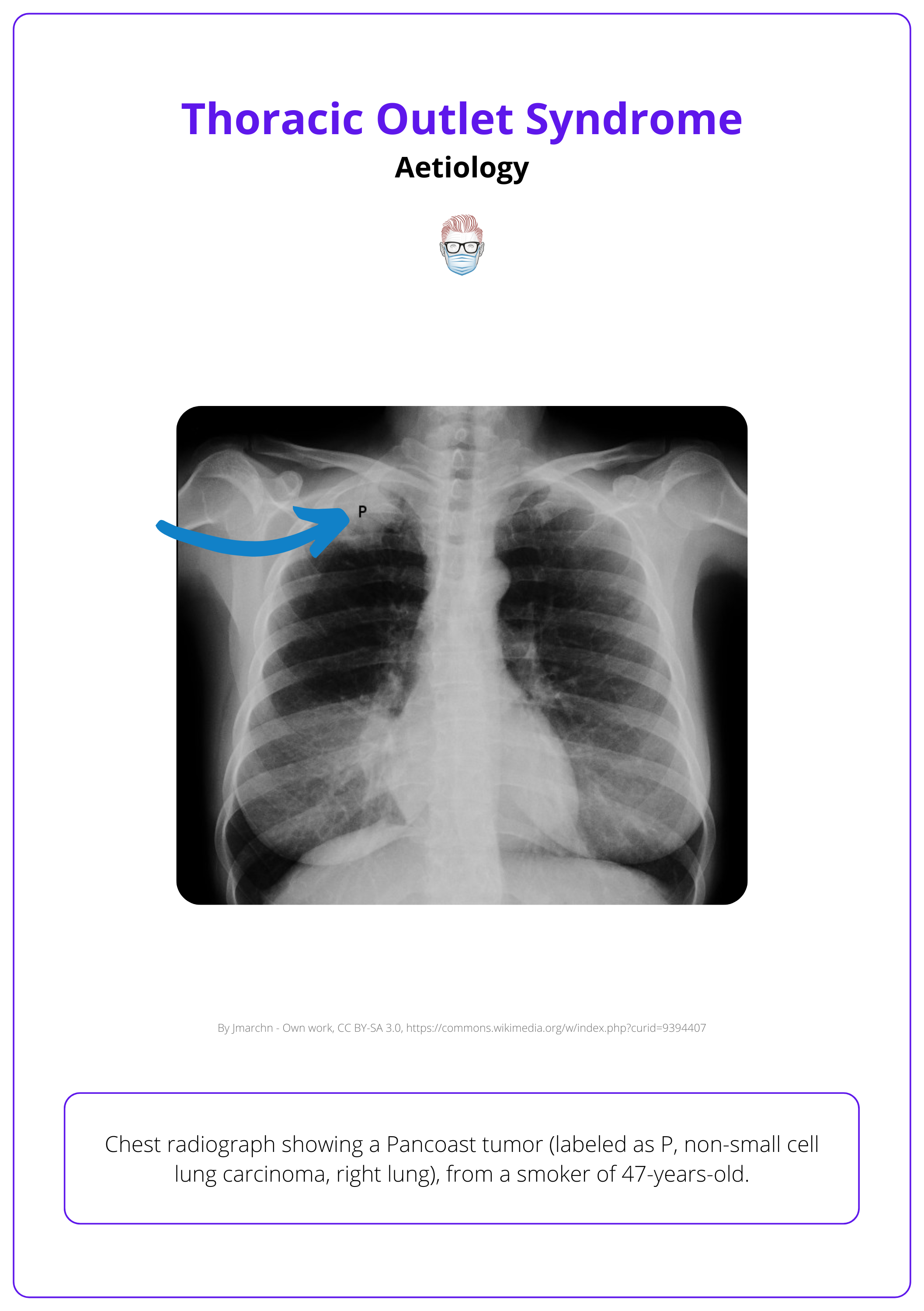
Tumors such as Pancoast tumors and schwannomas, alongside trauma from repetitive athletic movements or vertebral artery compression, all contribute to compression and subsequent Thoracic Outlet Syndrome.
Tumors
- Pancoast Tumor: Impacts the lower part of the brachial plexus.
- Schwannoma: Can significantly compress nearby neurovascular structures.
The radiographed image below illustrates a Pancoast tumor.
Trauma
- Repetitive Athletic Movements: Sports requiring extensive shoulder movements, like swimming and weightlifting, frequently contribute to TOS development.
- Vertebral Artery Compression: Although uncommon, this condition can cause visual disturbances and is linked to TOS.
Sibson’s fascia, which extends over the parietal pleura up to the first rib without attaching to it, can contribute to compression (Reddenbach, 1998).
Presentation of Thoracic Outlet Syndrome
TOS can present with a range of symptoms, often reflecting neurological or vascular compression, or both, leading to frequent delays in diagnosis.
History
Clinical features of thoracic outlet syndrome include numbness and tingling in the upper limb and hand, especially in the C8/T1 dermatomes, along with fatigue and weakness. These symptoms are often accompanied by severe pain in the neck or upper limb.
Key points to note on history are:
- Pain: Upper arm, shoulder, and trapezius. It may be diffuse or well localised due to the location of proximal compression.
- Paraesthesia: Generalized or localized to C8/T1 distribution
- Weakness: Progressive, worsens with repetitive activity
Secondary non-specific features can be associated with thoracic outlet syndrome, such as:
- Headache & visual disturbance due to vertebral artery compression.
- Facial and tongue symptoms may also occur.
Symptoms may be dynamic and depend on upper limb position due to the pathophysiology of proximal compression.
Examination
A thorough examination for Thoracic Outlet Syndrome (TOS) involves systematic inspection and palpation to identify signs of neurovascular compression.
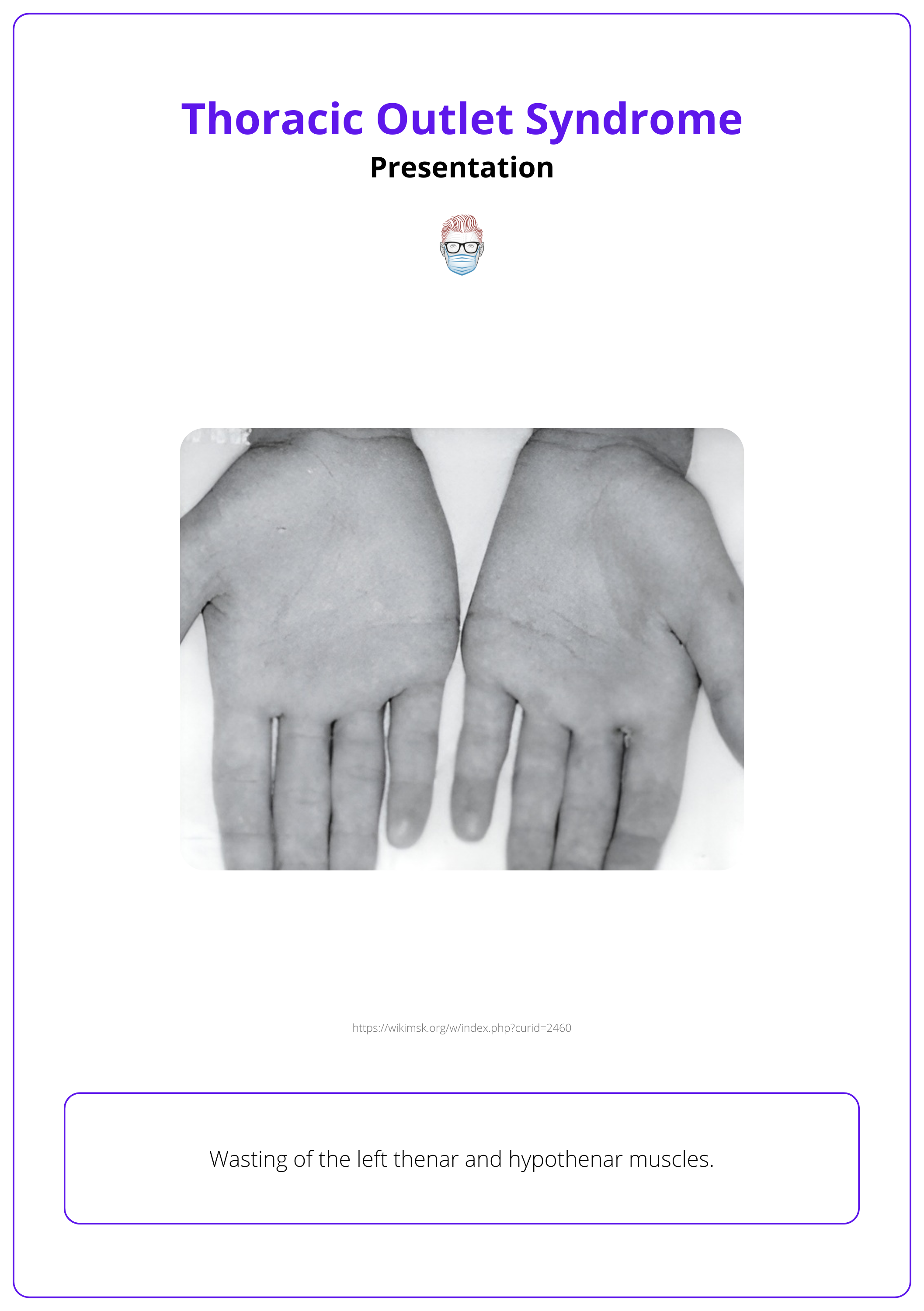
Inspection
- Neck and Posture: Short or "pecking" neck, kyphosis, rounded shoulders.
- Trauma Signs: Clavicular fractures or surgical scars.
- Skin Changes: Pallor, swelling, Raynaud’s, or ischemic ulcers.
- Muscle Wasting: Thenar, hypothenar, interosseous (Gilliatt-Sumner hand).
The image below illustrates the wasting of left thenar and hypothenar muscles.
Palpation and Percussion
- Neck Masses: Palpate for any abnormal masses.
- Shoulder Movement: Clicking during movement.
- Muscle Asymmetry: Muscle wasting or asymmetry.
- Distal Coolness: Coolness in the extremities
- Medial Cutaneous Nerve: Involvement of lower trunk of brachial plexus.
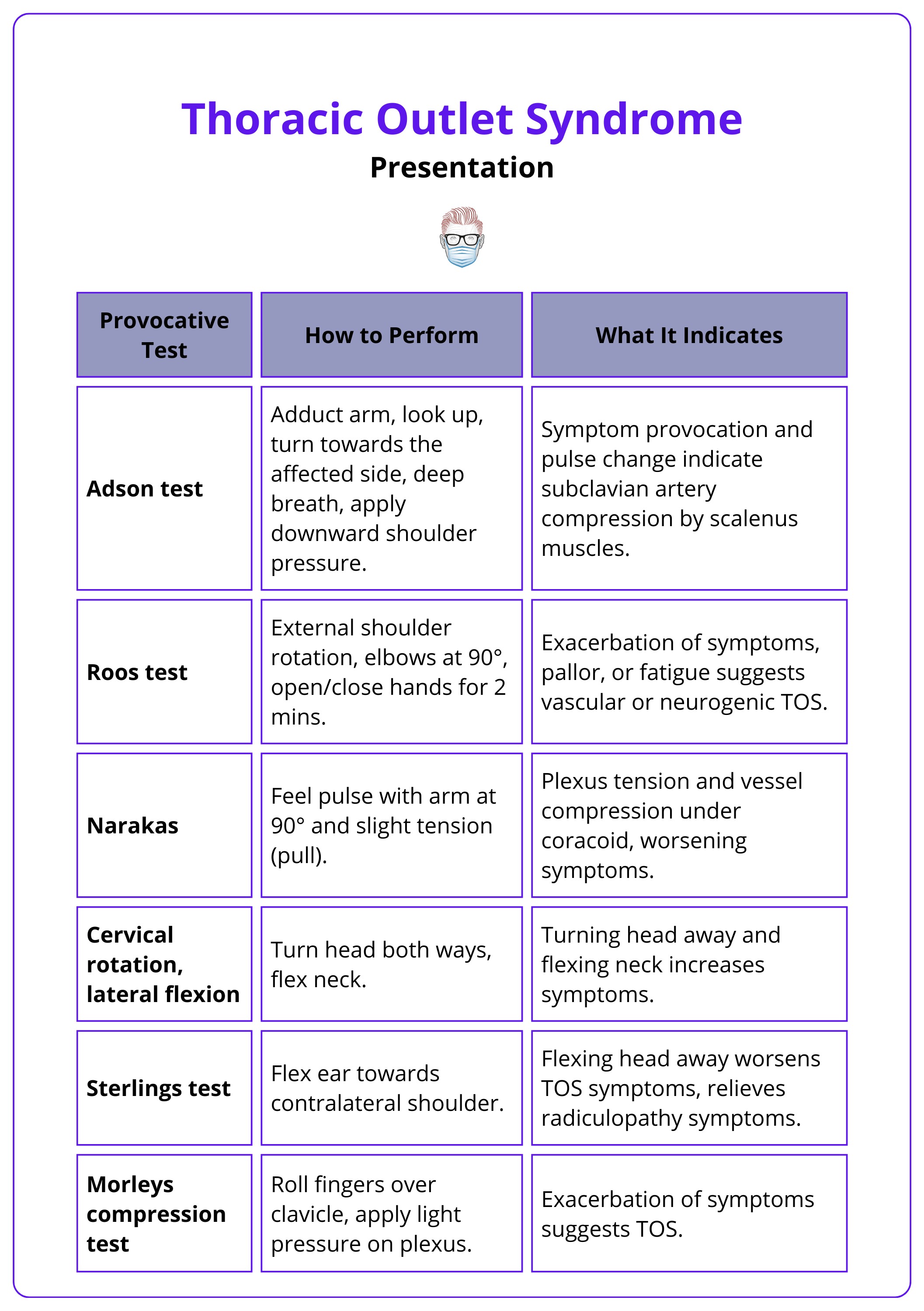
Eponymous Tests
- Tinel-Hoffman Sign: Test for nerve irritation over the brachial plexus.
- Adson Test: Evaluate for a collapsing pulse during hand elevation.
Other eponymous tests are detailed in the table below.
Differential Diagnosis
Neurogenic subtype is more common than vascular, of which venous is more frequent than arterial.
- Neurogenic: Cervical radiculopathy, ulnar nerve entrapment
- Venous: Arm swelling and discoloration with activity, generalized upper limb pain (Differential: Lymphoedema)
- Arterial: Unilateral pallor, tingling in the hand (worse in cold), distal arterial compromise (Differential: Raynaud's disease)
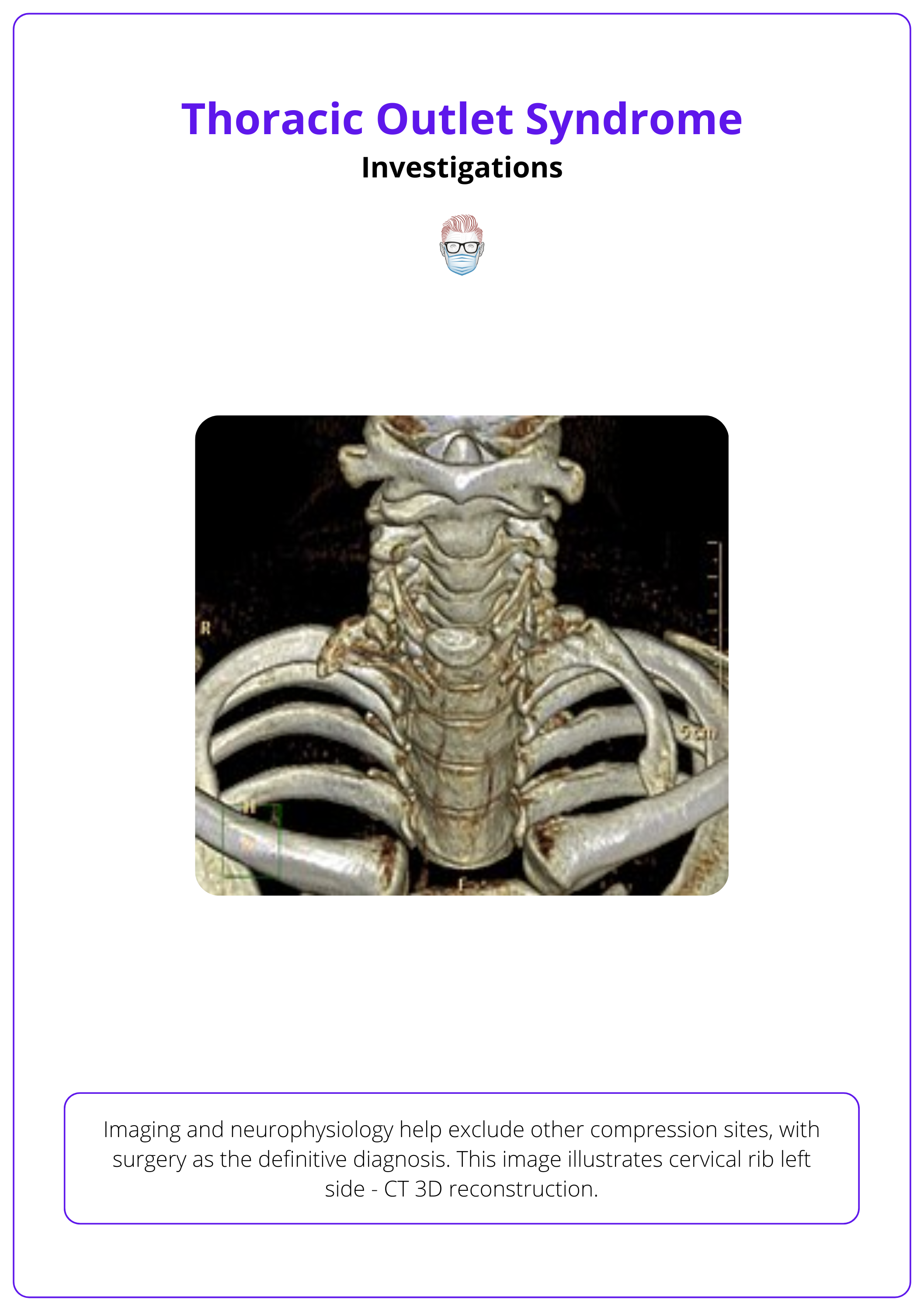
Investigations for Thoracic Outlet Syndrome
Investigating Thoracic Outlet Syndrome involves neurophysiological tests and imaging to rule out other causes, with surgery as the definitive diagnostic tool.
When evaluating Thoracic Outlet Syndrome (TOS), a combination of neurophysiological tests and imaging studies is essential to rule out other potential compression sites and to support the diagnosis. Surgery remains the most definitive diagnostic tool.
- Neurophysiology: primarily used to exclude compression at other anatomical sites, ensuring that symptoms are specific to TOS
- X-ray/CT Scan (C-spine and Chest): identifying structural anomalies, such as a cervical rib or a prominent C7/T1 spinous process.
- MRI: MRI is valuable for identifying anatomical abnormalities and nerve or vessel compression, with serial exams useful for tracking progression.
Surgical exploration provides the most definitive diagnosis for TOS. It allows direct visualization of the neurovascular structures, confirming the presence and extent of compression.
Management of Thoracic Outlet Syndrome
A multidisciplinary approach with physiotherapy, pain management, and surgery, which serves as both a diagnostic tool and treatment to relieve neurovascular compression.
Effective management of Thoracic Outlet Syndrome requires a multidisciplinary approach, combining non-surgical therapies with surgical intervention when necessary. Surgery not only serves as a definitive diagnostic tool but also provides the opportunity for decompression to relieve symptoms.
Non-Surgical Management
- Early Anticoagulation and Thrombolysis: Specifically recommended for vascular TOS to prevent and treat thrombosis (Ohman, 2023).
- Physiotherapy: Focuses on exercises designed to improve range of motion, strengthen muscles, and reduce pain associated with TOS.
- Occupational Therapy: Helps patients adapt to daily activities and reduce strain on the affected area.
- Psychological Support: Counseling and psychological support may be necessary for patients coping with chronic pain or disability.
Surgical Management
The primary objective of surgery is to confirm the diagnosis and alleviate any constriction affecting the neurovascular structures.
Surgical Approaches
There are two commonly utilised surgical approaches:
- Supraclavicular Approach: Commonly used due to its effectiveness in providing access to the thoracic outlet. Other approaches, such as trans-axillary, posterior, or inferior, are also viable depending on the specific case (Giehle, 2023).
- Robotic-Assisted Surgery (RATS): An emerging technique for first rib removal in TOS, offering enhanced precision and minimally invasive options (Azenha, 2022).
Surgical Procedure Overview:
The following outlines the essential steps in the surgical management of Thoracic Outlet Syndrome, covering patient preparation, surgical access, nerve protection, and closure.
- Patient Preparation: Position in a beach chair and apply local anesthesia
- Incision and Access: Make a skin incision, raise platysma flaps, and protect nerves and vessels; divide and repair the omohyoid if needed.
- Nerve Protection: safeguard the phrenic and suprascapular nerves.
- Address Anatomical Anomalies: Resect scalenus muscle anomalies or fibrous bands, and consider removing part of the scalenus anterior or first rib.
- Closure: Close the site in layers for optimal healing.
Here is video of a Roo's procedure for Thoracic Outlet Syndrome.
Conclusion
1. Basic of Thoracic Outlet Syndrome (TOS): Gained an understanding of Thoracic Outlet Syndrome as a compression of neurovascular structures.
2. Epidemiology and Aetiology: Learned about the epidemiology of TOS; its higher prevalence in adults with a female dominance and neurogenic form being the most common. Discussed the etiological factors including anatomical anomalies, tumors, or trauma leading to the condition.
3. Diagnosis and Presentation: Explored the diagnostic process involving neurophysiological testing and imaging such as X-rays, CT, and MRI. Discussed how TOS can present variably with symptoms often leading to a delay in diagnosis.
4. Management Strategies: Reviewed the multidisciplinary approach in managing TOS, which includes physiotherapy, pain control, occupational therapy, psychology, early anticoagulation for vascular TOS, and surgical interventions.
5. Surgical and Non-Surgical Treatments: Explored the definitive diagnostic and therapeutic roles of surgery in TOS, alongside conservative treatments and the significance of early and accurate intervention.
Further Reading
- Dolan RT, Moosa A, Giele HP. The Adipofascial Deltopectoral Flap to Cover the Brachial Plexus in Thoracic Outlet Syndrome and Radiation Plexitis. J Plast Reconstr Aesthet Surg. 2020 Aug;73(8):1465-1472. doi: 10.1016/j.bjps.2020.02.039. Epub 2020 Mar 13. PMID: 32467081.
- Jammeh ML, Yang A, Abuirqeba AA, Ohman JW, Thompson RW. Reoperative Brachial Plexus Neurolysis After Previous Anatomically Complete Supraclavicular Decompression for Neurogenic Thoracic Outlet Syndrome: A 10-Year Single-Center Case Series. Oper Neurosurg (Hagerstown). 2022 Aug 1;23(2):125-132. doi: 10.1227/ons.0000000000000252. Epub 2022 May 9. PMID: 35838452; PMCID: PMC9287103.
- Tzou CH, Paternostro-Sluga T, Frey M, Aszmann OC. Birth brachial plexus palsy caused by cervical rib. J Plast Reconstr Aesthet Surg. 2014 Jul;67(7):1004-5. doi: 10.1016/j.bjps.2014.02.020. Epub 2014 Feb 26. PMID: 24630141.
- Nagasao T, Morotomi T, Kuriyama M, Kogure T, Kudo H, Hamamoto Y, Tamai M. Thoracic outlet syndrome after the Nuss procedure for pectus excavatum: Is it a rare complication? J Plast Reconstr Aesthet Surg. 2017 Oct;70(10):1433-1439. doi: 10.1016/j.bjps.2017.05.043. Epub 2017 Jun 3. PMID: 28662867.
- Hearn SL, Medley K, Liao EA. Kinked again! From congenital brachial plexus palsy to adult neurogenic thoracic outlet syndrome: Case Report. Am J Phys Med Rehabil. 2024 Jul 2. doi: 10.1097/PHM.0000000000002572. Epub ahead of print. PMID: 38954650.
- Dengler NF, Ferraresi S, Rochkind S, Denisova N, Garozzo D, Heinen C, Alimehmeti R, Capone C, Barone DG, Zdunczyk A, Pedro MT, Antoniadis G, Kaiser R, Dubuisson A, Kretschmer T, Rasulic L. In Reply: Thoracic Outlet Syndrome Part I: Systematic Review of the Literature and Consensus on Anatomy, Diagnosis, and Classification of Thoracic Outlet Syndrome, and Thoracic Outlet Syndrome Part II: Consensus on the Management of Thoracic Outlet Syndrome by the European Association of Neurosurgical Societies' Section of Peripheral Nerve Surgery. Neurosurgery. 2024 Jul 11. doi: 10.1227/neu.0000000000003112. Epub ahead of print. PMID: 38990007.
- Abdalla BA, Kakamad FH, Namiq HS, Asaad SK, Abdullah AS, Mustafa AM, Ghafour AK, Kareem HO, Ahmed SQM, Mohammed BA, Hasan KM, Mohammed SH. Pediatric thoracic outlet syndrome: a systematic review with metadata. Pediatr Surg Int. 2024 Jul 13;40(1):186. doi: 10.1007/s00383-024-05769-y. PMID: 39003407.
- Davies MG, Hart JP. Endovascular management of acute and subacute venous thoracic outlet syndrome. Front Surg. 2024 Feb 19;11:1302568. doi: 10.3389/fsurg.2024.1302568. PMID: 38440414; PMCID: PMC10909919.
- Thompson JF, Winterborn RJ, Bays S, White H, Kinsella DC, Watkinson AF. Venous thoracic outlet compression and the Paget-Schroetter syndrome: a review and recommendations for management. Cardiovasc Intervent Radiol. 2011 Oct;34(5):903-10. doi: 10.1007/s00270-011-0148-4. Epub 2011 Mar 30. PMID: 21448772.
- Teijink SBJ, Goeteyn J, Pesser N, van Nuenen BFL, Thompson RW, Teijink JAW. Surgical approaches for thoracic outlet decompression in the treatment of thoracic outlet syndrome. J Thorac Dis. 2023 Dec 30;15(12):7088-7099. doi: 10.21037/jtd-23-546. Epub 2023 Dec 14. PMID: 38249887; PMCID: PMC10797336.
- Jammeh ML, Yang A, Abuirqeba AA, Ohman JW, Thompson RW. Reoperative Brachial Plexus Neurolysis After Previous Anatomically Complete Supraclavicular Decompression for Neurogenic Thoracic Outlet Syndrome: A 10-Year Single-Center Case Series. Oper Neurosurg (Hagerstown). 2022 Aug 1;23(2):125-132. doi: 10.1227/ons.0000000000000252. Epub 2022 May 9. PMID: 35838452; PMCID: PMC9287103.
- Willshire WH. Supernumerary first rib: clinical records. Lancet. 1860;2:633.
- Giehle H. Thoracic outlet syndrome Pulvertaft video https://youtu.be/cbPlVt_EfKY?feature=shared
- Illig KA, Rodriguez-Zoppi E. How Common Is Thoracic Outlet Syndrome? Thorac Surg Clin. 2021 Feb;31(1):11-17. doi: 10.1016/j.thorsurg.2020.09.001. PMID: 33220767.
- Tzou CH, Paternostro-Sluga T, Frey M, Aszmann OC. Birth brachial plexus palsy caused by cervical rib. J Plast Reconstr Aesthet Surg. 2014 Jul;67(7):1004-5. doi: 10.1016/j.bjps.2014.02.020. Epub 2014 Feb 26. PMID: 24630141.
- Redenbach DM, Nelems B. A comparative study of structures comprising the thoracic outlet in 250 human cadavers and 72 surgical cases of thoracic outlet syndrome. Eur J Cardiothorac Surg. 1998 Apr;13(4):353-60. doi: 10.1016/s1010-7940(98)00037-2. PMID: 9641331.
- Ohman JW, Thompson RW. Thoracic Outlet Syndrome in the Overhead Athlete: Diagnosis and Treatment Recommendations. Curr Rev Musculoskelet Med. 2020 Aug;13(4):457-471. doi: 10.1007/s12178-020-09643-x. PMID: 32514995; PMCID: PMC7340704.
- Azenha LF, Kocher GJ, Kestenholz PB, Gioutsos K, Minervini F. Thoracic outlet syndrome: a retrospective analysis of robotic-assisted first rib resections. J Robot Surg. 2023 Jun;17(3):891-896. doi: 10.1007/s11701-022-01486-7. Epub 2022 Nov 3. PMID: 36327061.
- Hart AM, BAPRAS National Teaching, Peripheral nerve. Accessed 10th August 2024.
- Lewis, Mark, et al. "The diagnosis of thoracic outlet syndrome." Journal of Vascular Diagnostics (2014): 113-120.


