Swan Neck vs Boutonnières Deformity
Swan-Neck and Boutonnière deformities are conditions affecting theproximal interphalangeal joint (PIPJ) – this is really their only similarity.
Their main differences are related to clinical findings, mechanics, pathophysiology, classification and treatments.
| Differences | Swan-Neck Deformity | Boutonnières Deformity |
|---|---|---|
| Signs | PIPJ Hyperextension DIPJ Flexion | PIPJ Flexion DIPJ Hyperextension |
| Symptoms | Functional immobility | Aesthetic concern |
| Causes | Pathology at wrist, MCPJ, PIPJ or DIPJ. | Pathology at the PIPJ only |
| Biomechanics | Extension > Flexion Force | Volar migration of lateral bands |
| Classification | Nalebufff Classification 1 | Nalebuff and Millers Classification |
| Treatment | Splints Tendon Release Joint Surgery | Splints Tendon Release Joint Surgery |
This article further explores these differences in further detail.
Swan Neck Deformity
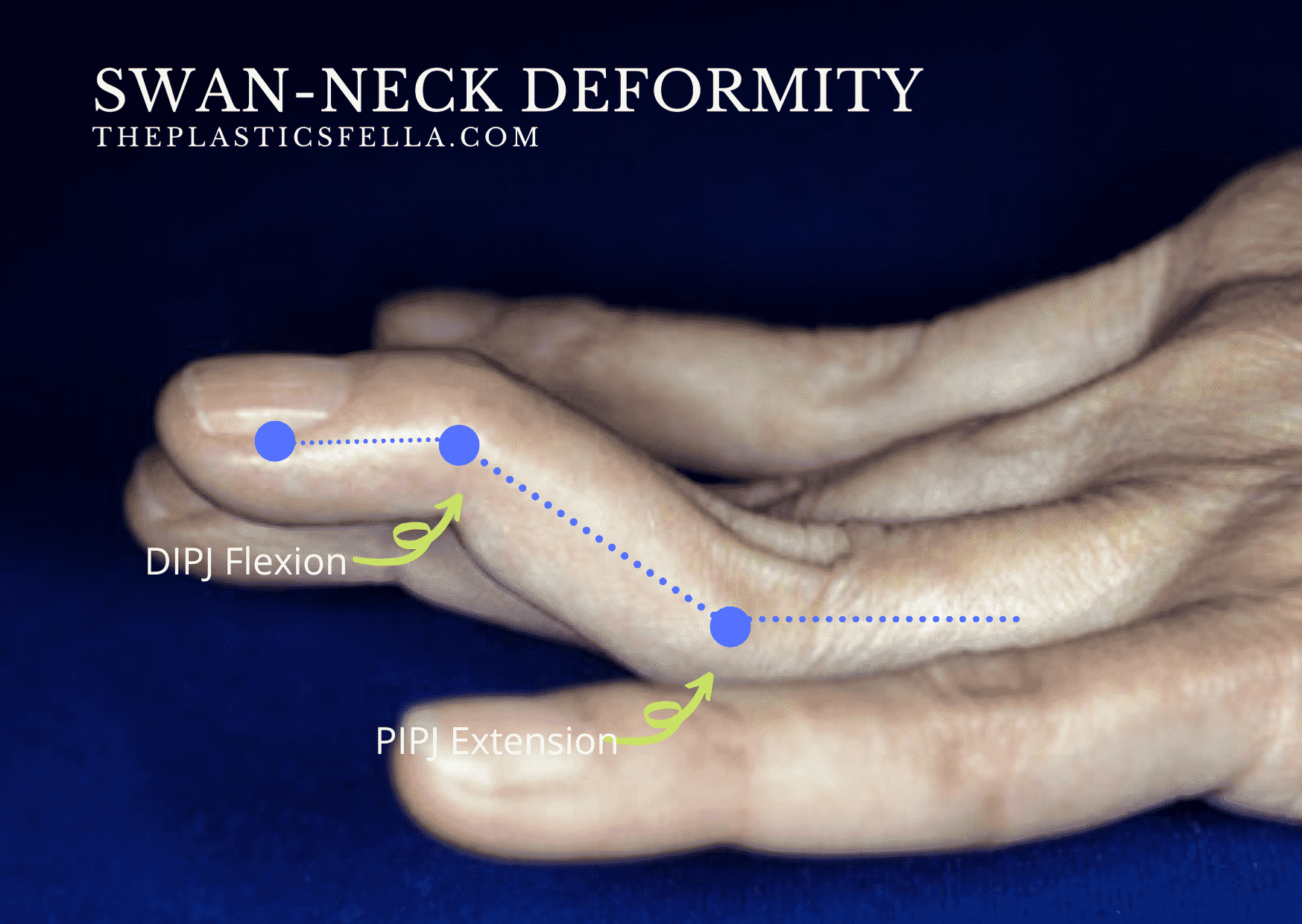
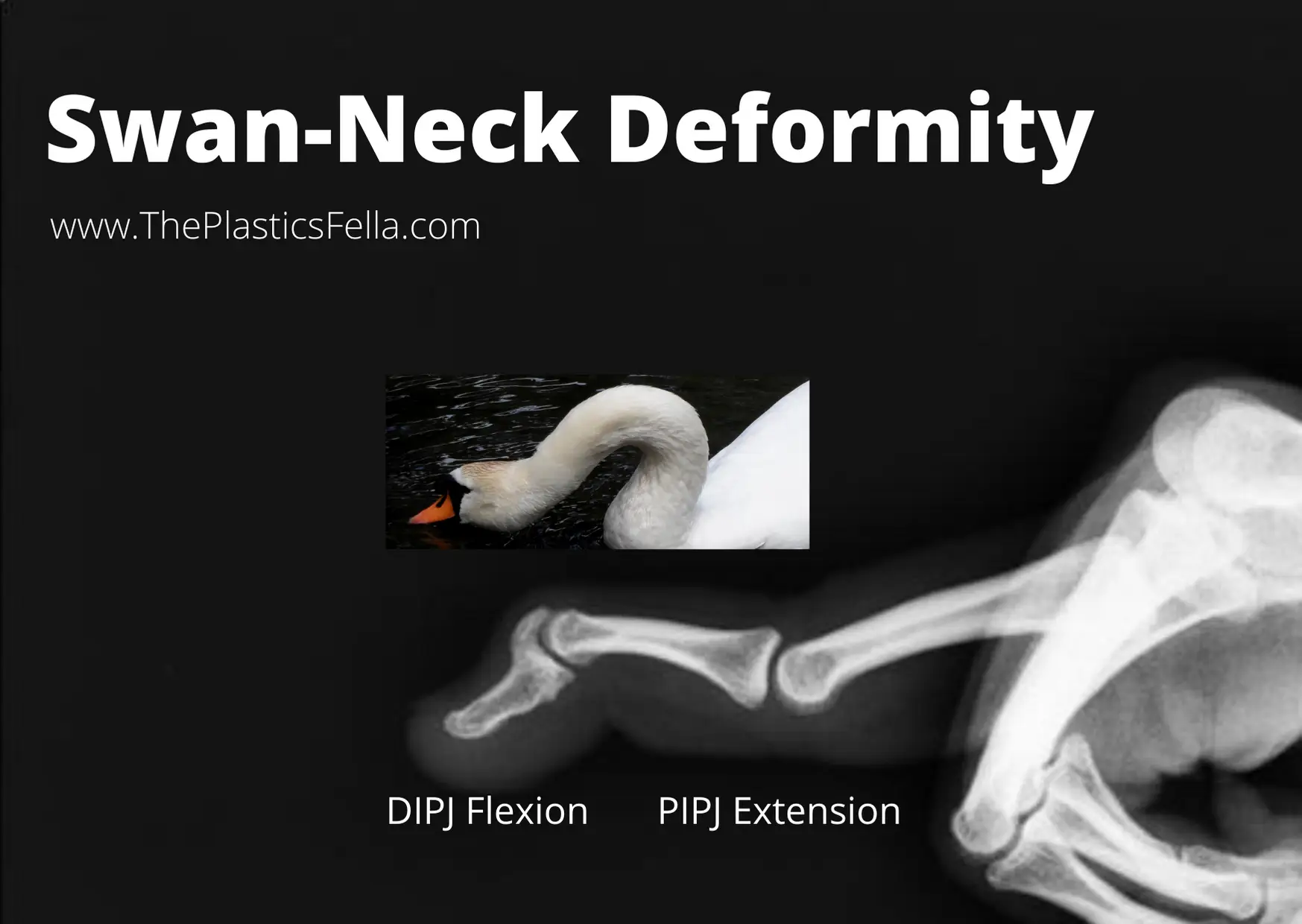
Swan-Neck deformities are characterized by PIPJ hyperextension, with reciprocal flexion at the DIPJ and MCPJ. A patient with a swan-neck deformity has impaired function due to an inability to make a full fist due to loss of PIPJ flexion.
Signs of Swan-Neck Deformity
Swan-neck deformity has the classic clinical signs of PIPJ hyperextension and MCPJ/DIPJ flexion2. This creates a “Z-mechanism” due to an imbalance in forces and is illustrated in the diagram below:
Anatomy
Finger anatomy, in particular the volar plate, lateral bands and terminal tendon and, is key to understanding the biomechanics of swan-neck deformities.
This diagram illustrates the main forces involved in swan-neck deformity.
Cause and Biomechanics
Several causes for swan-neck deformities have been described. The following table describes the most common causes of swan-neck deformities and their biomechanics/pathophysiology.
| Cause | Biomechanics/Pathophysiology |
|---|---|
| Wrist Synovitis | Carpal collapse, supination and ulnar translation lengthens/weakens tendons, which are then overpowered by the intrinsic muscles. This causes MCPJ flexion and PIPJ extension3 |
| MCPJ Synovitis | Extensor tendon insertion point at the proximal phalanx becomes weakened. This increases force to middle phalanx and results in PIPJ hyperextension. |
| MCPJ Volar Plate | A weakened volar plate causes MCPJ subluxation and intrinsic muscle shortening. This causes PIPJ hyperextension. |
| PIPJ Synovitis | Synovitis at the PIPJ attenuates the volar plate and TRL resulting in dorsal translation of the lateral band and destruction of FDS insertion. This causes PIPJ hyperextension, which in turn causes DIPJ flexion due to an increase in FDP tension and decreased in lateral band tension. |
| PIPJ Volar Plate | A lax volar plate allows for PIPJ hyperextension |
| DIPJ Mallet Injury | Rupture of the terminal extensor tendon allows proximal migration and relaxation of the lateral bands. Extensor power is then concentrated on the central slip, resulting in PIPJ hyperextension. The volar plate weekends over time. |
Radiology
X-ray often confirms clinical examination – PIPJ extension and DIPJ Flexion.
In chronic swan-neck deformities, joint changes can be seen – for example: loss of joint space, osteophytes. Joint changes are significant in the classification of Swan-neck deformities and therefore guide management options.
Treatment and Classification
The treatment for swan-neck deformity is guided by the cause and the severity as per Nalebuff’s classification. The main objective is to restore active flexion at the PIPJ if possible, or to fuse the joint in a functional position should this not be possible.
This table summaries Nalebuffs classification1 for swan-neck deformities and the recommended treatment options of splints, physiotherapy and surgery4.
| Grade | PIPJ | Treatment |
|---|---|---|
| 1 | Flexible | Silver Ring Splints Flexor Tenodesis5 FDS Sling6 Littler ORL reconstruction7 |
| 2 | Limited | Intrinsic Release at MCPJ |
| 3 | Fixed in hyperextension | MUA Intrinsic Release |
| 4 | Type 3 with X-Ray Findings | Arthrodesis Arthroplasty |
Boutonnière Deformity
A Boutonnière deformity its characterised by a flexion deformity of the PIPJ, with reciprocal extension at the MCPJ and DIPJ. Unlike a Swan-neck deformity, it is more of an aesthetic issue than a functional – patient can still make fists.
Signs of Boutonnière Deformity
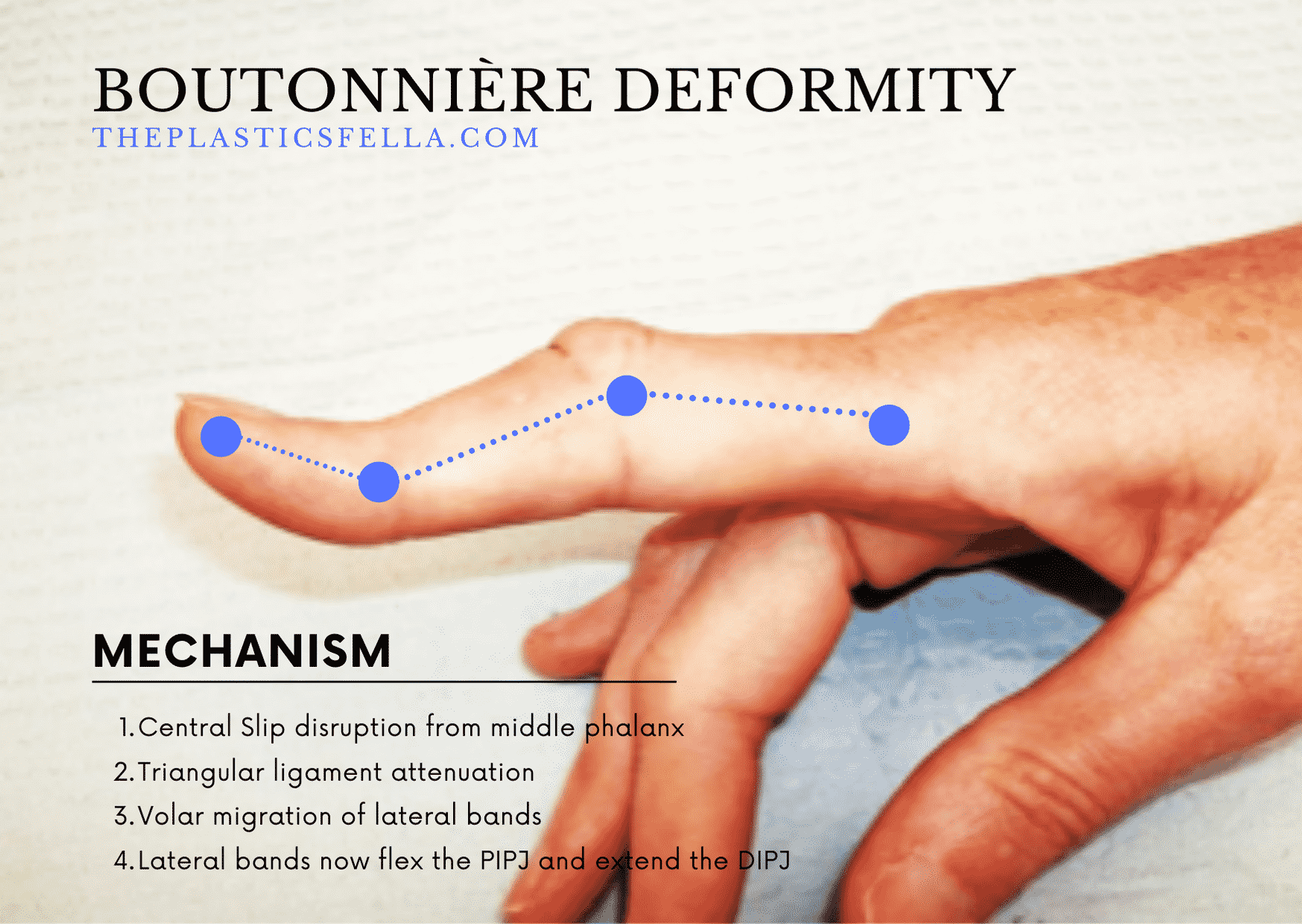
A Boutonniere deformity has the classic signs of MPCJ extension, PIPJ flexion, DIPJ extension. Boutonniere means “buttonhole” in French – the appearance of the PIPJ through the migrated lateral bands8.
This imbalance in forces and their biomechanics is illustrated in the the picture below.
Anatomy
Finger anatomy, in particular the central slip, triangular ligament and lateral bands, is key to understanding the biomechanics of swan-neck deformities9.
Cause and Biomechanics
The cause of a Boutonniere deformity is central slip dysfunction at the PIPJ (zone III). This is commonly due to a central slip tear from trauma or a central slip attenuation from a synovitis. The latter is seen in rheumatoid arthritis.
The biomechanical sequelae of this central slip dysfunction is as follows:
- Triangular ligament stretches
- Lateral bands sublux in a volar direction, maintaining a persistent PIPJ flexion
- Lumbricals and interosseous muscles transmit force into the distal phalanx.
- In chronic cases, fixture joint contractors develop.
To put it simply, the lateral bands now flex the PIPJ and extend the DIPJ.
Treatment and Classification
Boutonniere deformity can be graded into Nalebuff and Millers Classification, which guides the appropriate treatment pathway.
| Grade | PIPJ | Treatment |
|---|---|---|
| 1 | Extensor Lag of 10-15°, passively correctable | Splinting Steroid Injection Dolphin or Fowler Tenotomy |
| 2 | Extensor lag of 30-40°, passively correctable | Shorten central slip, or Centralise Lateral Bands10 |
| 3 | Fixed flexion deformity | Arthrodesis, or Swanson-type Arthroplasty |
| 4 | Stage 3 with Arthritis | Arthrodesis, or Swanson-type Arthroplasty |
The purpose of splinting is is to achieve full PIPJ extension whilst DIPJ passive flexion exercises are being done. This should be continued for a minimum of 8 weeks to gain the maximum possible correction. If splinting is unsuccessful, a surgical release of the joint is considered.
Any tendon surgery should be delayed until good passive motion of the joint is restored. In these surgeries, care must be taken not to jeopardise flexor function in an effort to restore PIPJ extension, since this will result in a greater functional deficit. In several, the results were unpredictable, with only modest improvement in the proximal interphalangeal extension, which deteriorated over time. Arthrodesis should be reserved for the most severe rheumatoid boutonniere deformities11.
FAQs
What’s the difference between Swan-Neck and Boutonniere Deformity? There are 5 key differences between these two conditions: cause, clinical findings, anatomical pathology, classification and treatment. The only real similarity is that they involve the PIPJ and can be treated with splinting or surgery.
Who was Nalebuff? Nalebuff provides the classifications for both swan neck and boutonniere deformities Edward Nalebuff was a pioneer in hand surgery and clinical professor emeritus at the Tufts School of Medicine. More information can be found here.
Bibliography
- 1. Nalebuff E. The rheumatoid swan-neck deformity. Hand Clin. 1989;5(2):203-214. https://www.ncbi.nlm.nih.gov/pubmed/2661576.
- 2. Heywood AWB. The Pathogenesis of the Rheumatoid Swan Neck Deformity. Hand. June 1979:176-183. doi:10.1016/s0072-968x(79)80031-5
- 3. Shapiro JS. Wrist involvement in rheumatoid swan-neck deformity. The Journal of Hand Surgery. September 1982:484-491. doi:10.1016/s0363-5023(82)80045-2
- 4. Boyer M, Gelberman R. Operative correction of swan-neck and boutonniere deformities in the rheumatoid hand. J Am Acad Orthop Surg. 1999;7(2):92-100. doi:10.5435/00124635-199903000-00002
- 5. Tonkin MA, Hughes J, Smith KL. Lateral band translocation for swan-neck deformity. The Journal of Hand Surgery. March 1992:260-267. doi:10.1016/0363-5023(92)90402-b
- 6. Wei DH, Terrono AL. Superficialis Sling (Flexor Digitorum Superficialis Tenodesis) for Swan Neck Reconstruction. The Journal of Hand Surgery. October 2015:2068-2074. doi:10.1016/j.jhsa.2015.07.018
- 7. Littler J, Eaton R. Redistribution of forces in the correction of Boutonniere deformity. J Bone Joint Surg Am. 1967;49(7):1267-1274. https://www.ncbi.nlm.nih.gov/pubmed/5622971.
- 8. Massengill J. The boutonniere deformity. Hand Clin. 1992;8(4):787-801. https://www.ncbi.nlm.nih.gov/pubmed/1460075.
- 9. Grau L, Baydoun H, Chen K, Sankary ST, Amirouche F, Gonzalez MH. Biomechanics of the Acute Boutonniere Deformity. The Journal of Hand Surgery. January 2018:80.e1-80.e6. doi:10.1016/j.jhsa.2017.07.011
- 10. Gainor BJ, Hummel GL. Correction of rheumatoid swan-neck deformity by lateral band mobilization. The Journal of Hand Surgery. May 1985:370-376. doi:10.1016/s0363-5023(85)80037-x
- 11. Kiefhaber TR, Strickland JW. Soft tissue reconstruction for rheumatoid swan-neck and boutonniere deformities: Long-term results. The Journal of Hand Surgery. November 1993:984-989. doi:10.1016/0363-5023(93)90387-i


