Summary Card
Definition
Sternal wound infections are divided into superficial (skin subcutaneous tissue and fascia) and deep (extending down to sternal bone hardware and mediastinum).
Classification
SWIs are often classified according to timing from surgery; for example, the Palierolero classification.
Risk Factors
Risk factors can be grouped into patient-related (e.g., diabetes and obesity), intraoperative (e.g., increased surgical time), and postoperative factors (e.g., prolonged ICU stay).
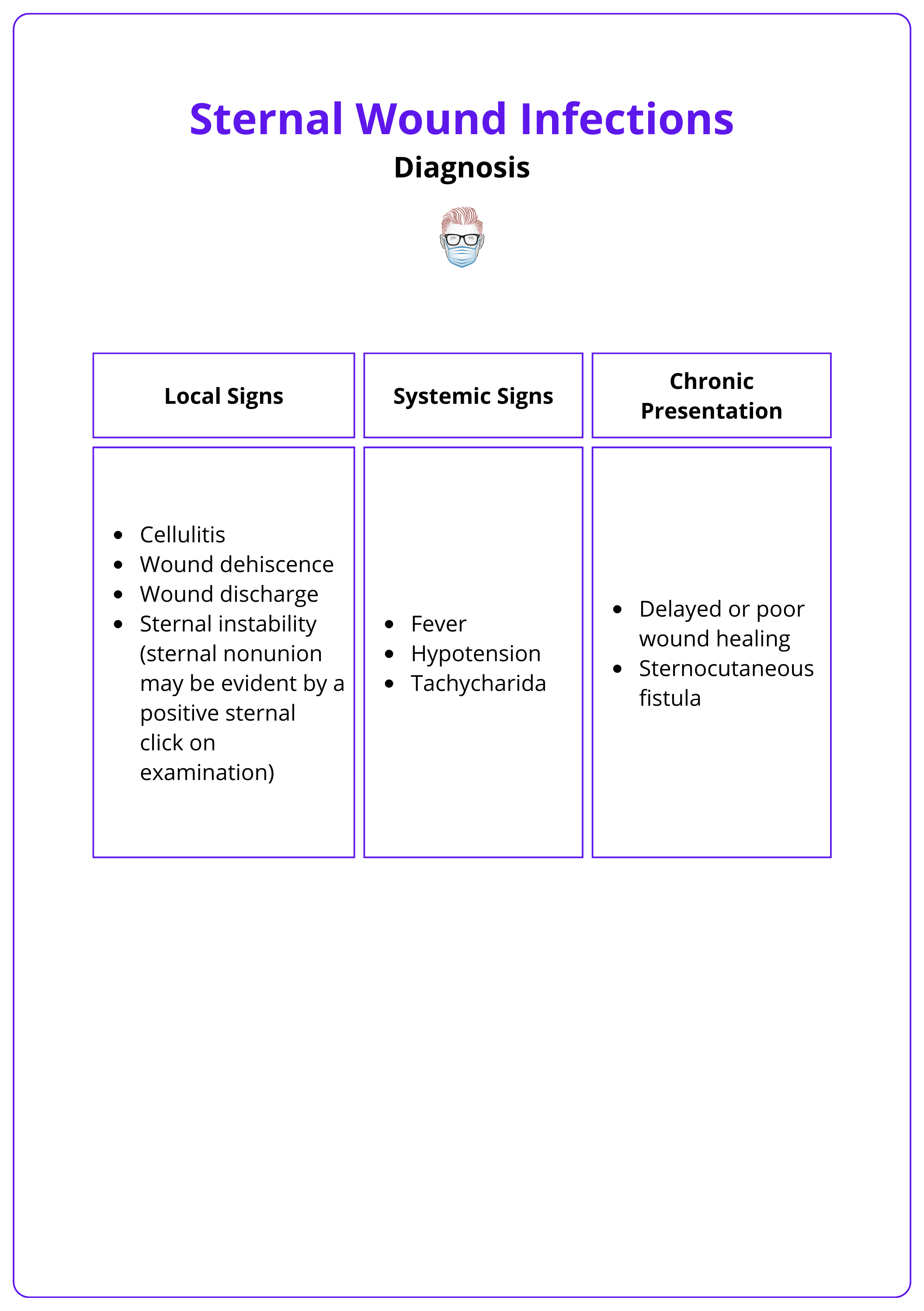
Diagnosis
Diagnosis is clinical and can be supported by laboratory tests such as FBC, ESR, CRP, and blood culture and imaging such as CXR and CT.
Treatment
Superficial infections can be treated with antibiotics and local wound care while DSWI requires debridement, hardware removal, and early closure including flap closure.
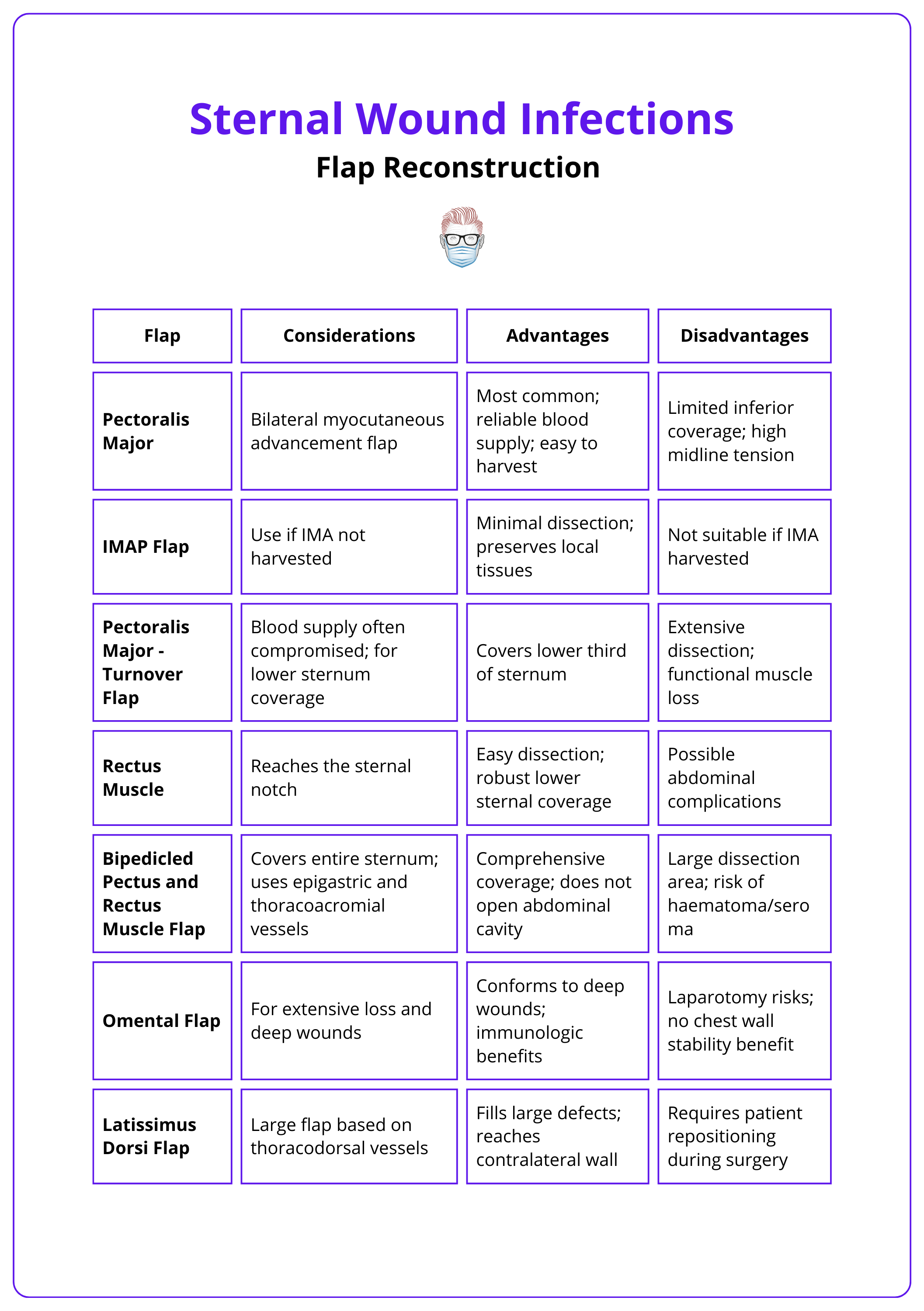
Flap Reconstruction
Pectoralis major, rectus abdominis, latissimus dorsi, and omental flaps are the main flaps used for soft tissue cover in SWIs.
Complications
Complications with sternal wound infections include recurrent wound infections and wound dehiscence flap donor site morbidity (e.g., hernia) post rectus abdominis harvest.
Primary Contributor: Dr Waruguru Wanjau, Educational Fellow.
Reviewer: Dr Suzanne Thomson, Educational Fellow.
Definition of Sternal Wound Infections
Sternal wound infections are divided into superficial (skin subcutaneous tissue and fascia) and deep (extending down to sternal bone hardware and mediastinum)
Sternal wound infections are classified based on the depth of the infection. Superficial infections affect skin and subcutaneous layers, while deep infections extend to the sternal bone and beyond.
Superficial Sternal Wound Infections (SSWI)
- Involves the skin, subcutaneous tissue, and pectoralis fascia.
- Defined as infections that do not extend beyond the pectoralis fascia (Singh, 2011).
SSWI generally has a lower mortality risk, ranging from 0.5% to 9%, whereas DSWI has a significantly higher risk, reported between 10% and 47% (Singh, 2011).
Deep Sternal Wound Infections (DSWI)
A DSWI is characterized by (Garner, 1988):
- An organism isolated from the culture of mediastinal tissue or fluid.
- Evidence of mediastinitis observed during surgical intervention.
- Presence of symptoms such as chest pain, sternal instability, or fever over 38°C, alongside:
- Purulent drainage from the mediastinum and the isolation of an organism present in a blood culture
- Culture of the mediastinal area
A DSWI can be considered as soft-tissue openings that extend down to the sternal bone and hardware (Levy, 2019). DSWI can involve the mediastinum, bone, or cartilage, and infections beneath the subcutaneous tissue (Yusuf, 2018).
Mediastinitis, a severe complication after coronary artery bypass surgery, doubles the mortality rate in patients with deep sternal wound infection (DSWI). (Braxton, 2004).
Classification of Sternal Wound Infections
SWIs can be classified according to timing from surgery according to the Palierolero classification.
There are many classifications of SWI. Greig et al classified according to location (upper, lower, or entire sternum), which can be used to guide the best reconstructive option (Hever, 2021).
SWIs can also be classified according to timing from surgery – the Palierolero classification which is detailed in the table below (Palierolero, 1991 & Singh, 2011).
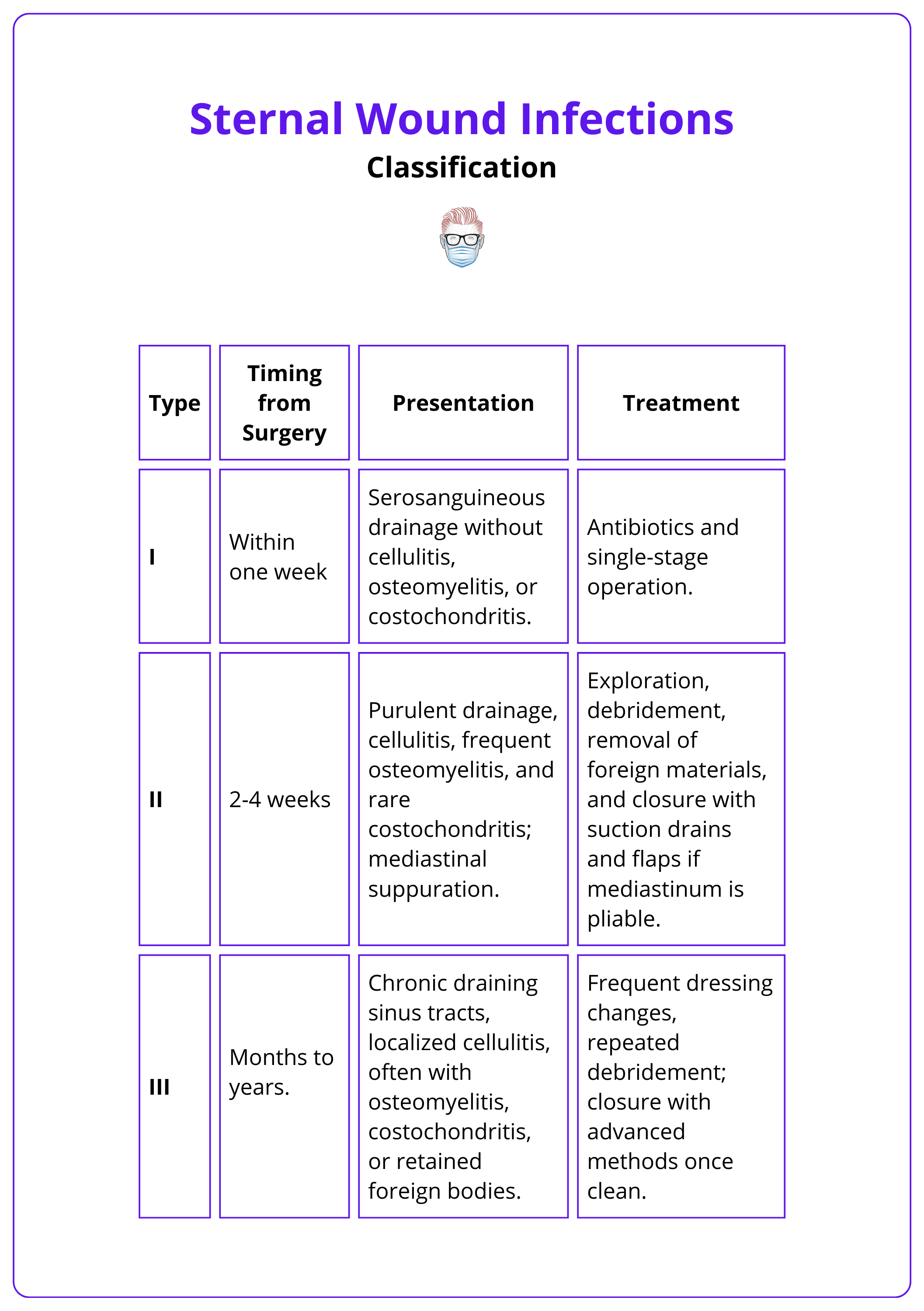
Kitano et al added a fourth classification which included infection of aortic grafts used to repair aortic arch aneurysms as exposure to grafts exacerbated infection and necessitated surgical replacement conferring higher mortality rates (Kitano, 2022).
Risk Factors for Sternal Wound Infections
Risk factors can be grouped into patient-related (e.g., diabetes and obesity), intraoperative (e.g., increased surgical time), and postoperative factors (e.g., prolonged ICU stay).
Major risk factors for the development of a DSWI following cardiac surgery can be grouped into patient-related, intraoperative, and postoperative factors as detailed in the table below (Levy, 2019 & Singh, 2011 & Cutrell, 2016).
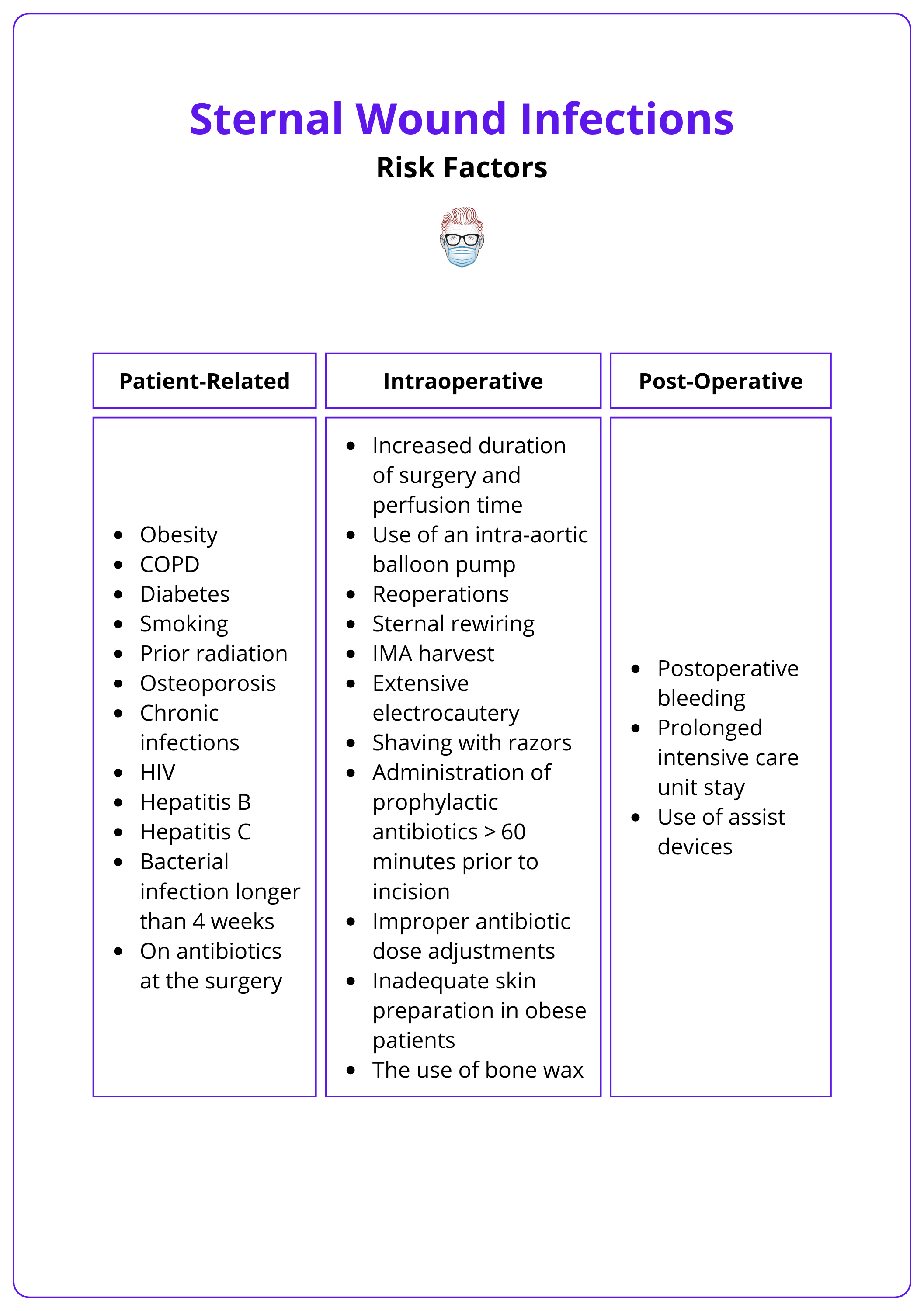
Patients undergoing a median sternotomy for coronary artery bypass grafting have the highest rate of sternal wound infections compared with those for other surgeries (Singh, 2011).
Diagnosis of Sternal Wound Infections
Diagnosis is clinical and can be supported by laboratory tests such as FBC, ESR, CRP, blood culture, and imaging such as CXR, CT, and MRI.
Aetiology
Sternal wound infections can be caused by primary or secondary infections.
- Primary: Staphylococcus aureus is the most commonly isolated pathogen in DSWIs, followed by Coagulase-Negative Staphylococci (CoNS).
- Secondary: After initial surgical and antibiotic treatments, infections that persist tend to involve Gram-negative rods, particularly Enterobacteriaceae, with a decreasing proportion of Gram-positive cocci (Chan, 2016).
Rarely, DSWI can also occur by hematogenous route (mainly in children) and by contiguous extension from an adjacent infectious process (e.g., arthritis) (De foe, 2001).
Infections with Gram-negative rods are associated with a worse prognosis compared to those caused by Gram-positive organisms (Yusuf, 2018).
Clinical Features
The diagnosis of DSWI is clinical in nature. The local, systematic, and chronic presentation of a DSWI is detailed in the table below.
Investigations
A sternal wound infection requires comprehensive laboratory and radiology investigations.
- Laboratory Tests: Infective and inflammatory markers, cultures.
- CXR: Mediastinal widening, air-fluid level, pneumomediastinum, pleural effusion.
- CT chest: Assess dehiscence depth and identify fluid collections, abscesses, air pockets, extension into adjacent structures, pleural or pericardial fluid, adenopathy, and parenchymal or sternal abnormalities.
- MRI: Early osteomyelitis detection. Findings include hypointense signals on T1-weighted images and hyperintense signals on T2-weighted images.

PET combined with CT imaging is useful in localising the disease sites to guide adequate debridement. PET may also be used to monitor the response to therapy (Zhang, 2018).
Treatment of Sternal Wound Infections
Superficial infections can be treated with antibiotics and local wound care while DSWI requires debridement, hardware removal, negative pressure dressing, and closure.
Principles
Sternal wound infections should be treated by a multi-disciplinary team. Early administration of targeted antibiotics and local wound care is essential to prevent complications associated with DSWI/mediastinitis (Levy, 2019).
In relation to deep sternal wound infections, a recommended treatment approach (Levy, 2019 & Cauley, 2022) includes:
- Debridement: including hardware removal
- Sampling: Aseptic tissue and bone culture collection for tailored antibiotics
- Antibiotics: Start broad-spectrum antibiotics preoperatively and tailor them to cultures. Osteomyelitis typically requires a 6+ weeks regimen.
- Reconstruction: Stabilisation of the thoracic skeleton (respiration) & soft tissue coverage with flap reconstruction (obliterate dead space, protect organs).
When foreign bodies cannot be removed (e.g., pacing wires, graft material), staged debridement and reconstruction should be considered for ongoing infection concerns. (Levy, 2019)
Wound Management Options
After infection control, a flap can reconstruct the defect by eliminating dead space, providing vascularized tissue for healing and antibiotics, covering vital structures, and compressing sternal segments to promote bone healing. An algorithm for sternal wound closures can be found here.
Closure options include:
- Closed suction antibiotic catheter irrigation systems
- Vacuum-assisted closure (VAC)
- Flap Reconstruction: discussed in more detail below
VAC may be the only treatment for critically ill patients, especially with negative blood cultures, shallow wounds (<4 cm), low bony exposure, and sternal instability (Gladevitch, 2010). However, VAC use can increase bleeding risk and potentially damage underlying tissues, including rare right ventricular rupture. A skin graft with VAC dressing can enhance adherence and success (Gladevitch, 2010).
Flap Reconstruction for Sternal Wound Infections
Pectoralis major, rectus abdominis, latissimus dorsi, and omental flaps are the main flaps used for soft tissue cover in SWIs.
The goal of flap reconstruction is to eliminate dead space, provide vascularized tissue for healing and antibiotics, protect vital structures, and compress sternal segments for osseous healing.
Workhorse flaps for chest wall reconstruction include:
- Pectoralis major: unilateral turnover or rotation advancement, bilateral.
- Omental transposition
- Rectus abdominis muscle
- Latissimus dorsi muscle
The table below details flap reconstruction considerations, advantages, and disadvantages for each flap.
Complications of Sternal Wound Infections
Complications with sternal wound infections include recurrent wound infections, wound dehiscence, and flap donor site morbidity (e.g., hernia post rectus abdominis harvest).
Complications include:
- Recurrent wound infections
- Hematoma
- Wound dehiscence
- Re-exploration for wound necrosis
- Partial flap loss
- Donor site complications from flap harvest such as abdominal hernia formation after rectus abdominis harvest
Predictors of perioperative mortality after sternal debridement and muscle flap coverage (Patel, 2009).
- Presternotomy end-stage renal disease
- Chronic obstructive lung disease
- Mechanical ventilation
Postoperative adhesions between the posterior sternum and cardiac structures can easily shear and lead to dreaded complications of ventricle laceration or arterial graft avulsion (Levy, 2019).
Conclusion
1. Understanding Sternal Wound Infections: You have learned to distinguish between superficial and deep sternal wound infections, understanding their impact on patient health and the complexities.
2. Classification: You are familiar with the Palierolero classification system, categorizing SWIs based on the timing of their occurrence post-surgery.
3. Risk Factors: You have looked into risk factors that contribute to the development of SWIs, categorized into patient-related, intraoperative, and postoperative factors.
4. Diagnostic Proficiency: You understand the clinical signs of SWIs and the role of laboratory tests and imaging in confirming the diagnosis and planning treatment.
5. Treatment Strategies: You understand the differences in treatment approaches for superficial versus deep infections, including antibiotics, local wound care, and more aggressive interventions like debridement and flap reconstruction.
6. Flap Reconstruction Options: You have learned about various flap options for reconstructing defects caused by SWIs.
7. Complications: You understand the potential complications associated with SWIs and the importance of meticulous surgical technique and postoperative care to minimize these risks.
Further Reading
- Levy AS, Ascherman JA. Sternal Wound Reconstruction Made Simple. Plast Reconstr Surg Glob Open. 2019 Nov 27;7(11):e2488. doi: 10.1097/GOX.0000000000002488. PMID: 31942289; PMCID: PMC6908337.
- Pairolero PC, Arnold PG, Harris JB. Long-term results of pectoralis major muscle transposition for infected sternotomy wounds. Ann Surg. 1991 Jun;213(6):583-9; discussion 589-90. doi: 10.1097/00000658-199106000-00008. PMID: 2039289; PMCID: PMC1358581.
- Singh K, Anderson E, Harper JG. Overview and management of sternal wound infection. Semin Plast Surg. 2011 Feb;25(1):25-33. doi: 10.1055/s-0031-1275168. PMID: 22294940; PMCID: PMC3140234.
- Braxton JH, Marrin CA, McGrath PD, Morton JR, Norotsky M, Charlesworth DC, Lahey SJ, Clough R, Ross CS, Olmstead EM, O'Connor GT. 10-year follow-up of patients with and without mediastinitis. Semin Thorac Cardiovasc Surg. 2004 Spring;16(1):70-6. doi: 10.1053/j.semtcvs.2004.01.006. PMID: 15366690.
- Gdalevitch P, Afilalo J, Lee C. Predictors of vacuum-assisted closure failure of sternotomy wounds. J Plast Reconstr Aesthet Surg. 2010 Jan;63(1):180-3. doi: 10.1016/j.bjps.2008.08.020. Epub 2008 Nov 22. PMID: 19028156.
- Jones G, Jurkiewicz MJ, Bostwick J, Wood R, Bried JT, Culbertson J, Howell R, Eaves F, Carlson G, Nahai F. Management of the infected median sternotomy wound with muscle flaps. The Emory 20-year experience. Ann Surg. 1997 Jun;225(6):766-76; discussion 776-8. doi: 10.1097/00000658-199706000-00014. PMID: 9230817; PMCID: PMC1190886.
- Patel NV, Woznick AR, Welsh KS, Bendick PJ, Boura JA, Mucci SJ. Predictors of mortality after muscle flap advancement for deep sternal wound infections. Plast Reconstr Surg. 2009 Jan;123(1):132-138. doi: 10.1097/PRS.0b013e3181904b56. PMID: 19116546.
- De Feo M, Renzulli A, Ismeno G, Gregorio R, Della Corte A, Utili R, Cotrufo M. Variables predicting adverse outcome in patients with deep sternal wound infection. Ann Thorac Surg. 2001 Jan;71(1):324-31. doi: 10.1016/s0003-4975(00)02137-8. PMID: 11216770.
- Cutrell JB, Barros N, McBroom M, Luby J, Minhajuddin A, Ring WS, Greilich PE. Risk factors for deep sternal wound infection after cardiac surgery: Influence of red blood cell transfusions and chronic infection. Am J Infect Control. 2016 Nov 1;44(11):1302-1309. doi: 10.1016/j.ajic.2016.03.027. Epub 2016 May 11. PMID: 27179393.
- Chan M, Yusuf E, Giulieri S, Perrottet N, Von Segesser L, Borens O, Trampuz A. A retrospective study of deep sternal wound infections: clinical and microbiological characteristics, treatment, and risk factors for complications. Diagn Microbiol Infect Dis. 2016 Mar;84(3):261-5. doi: 10.1016/j.diagmicrobio.2015.11.011. Epub 2015 Nov 14. PMID: 26707065.
- Yusuf E, Chan M, Renz N, Trampuz A. Current perspectives on diagnosis and management of sternal wound infections. Infect Drug Resist. 2018 Jul 16;11:961-968. doi: 10.2147/IDR.S130172. PMID: 30038509; PMCID: PMC6053175.
- Pairolero PC, Arnold PG. Management of infected median sternotomy wounds. Ann Thorac Surg. 1986 Jul;42(1):1-2. doi: 10.1016/s0003-4975(10)61822-x. PMID: 3729602.
- Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections, 1988. Am J Infect Control. 1988 Jun;16(3):128-40. doi: 10.1016/0196-6553(88)90053-3. Erratum in: Am J Infect Control 1988 Aug;16(4):177. PMID: 2841893.
- Bakri K, Mardini S, Evans KK, Carlsen BT, Arnold PG. Workhorse flaps in chest wall reconstruction: the pectoralis major, latissimus dorsi, and rectus abdominis flaps. Semin Plast Surg. 2011 Feb;25(1):43-54. doi: 10.1055/s-0031-1275170. PMID: 22294942; PMCID: PMC3140231.
- Kitano D, Takahashi H, Nomura T, Okada K, Terashi H, Sakakibara S. A new clinical classification and reconstructive strategy for post-sternotomy surgical site infection. Regen Ther. 2022 Oct 29;21:519-526. doi: 10.1016/j.reth.2022.10.007. PMID: 36382133; PMCID: PMC9634152.
- Zhang R, Feng Z, Zhang Y, Tan H, Wang J, Qi F. Diagnostic value of fluorine-18 deoxyglucose positron emission tomography/computed tomography in deep sternal wound infection. J Plast Reconstr Aesthet Surg. 2018 Dec;71(12):1768-1776. doi: 10.1016/j.bjps.2018.07.017. Epub 2018 Aug 2. PMID: 30196022.
- Pech T, Kania A, Fehlberg W, Kalff JC, Walgenbach KJ, Busch KH. Therapie der Sternumosteomyelitis nach medianer Sternotomie bei 130 Patienten mittels gestielter myokutaner Latissimuslappenplastik [Treatment of Sternal Osteomyelitis after Median Sternotomy in 130 Patients with Pedicled Myocutaneous Latissimus Flap]. Zentralbl Chir. 2018 Aug;143(S 01):S51-S60. German. doi: 10.1055/a-0624-9574. Epub 2018 Sep 5. PMID: 30184571.
- Cauley RP, Barron S, Slatnick B, Maselli A, Kang C, Delvalle D, Chu L, Morris D. An Algorithmic Approach to the Surgical Management of Sternal Dehiscence: A Single-Center Experience. J Reconstr Microsurg. 2022 Oct;38(8):671-682. doi: 10.1055/s-0042-1743167. Epub 2022 Mar 4. PMID: 35253126.
- Hever P, Singh P, Eiben I, Eiben P, Nikkhah D. The management of deep sternal wound infection: Literature review and reconstructive algorithm. JPRAS Open. 2021 Mar 6;28:77-89. doi: 10.1016/j.jpra.2021.02.007. PMID: 33855148; PMCID: PMC8027694.
- Greig AV, Geh JL, Khanduja V, Shibu M. Choice of flap for the management of deep sternal wound infection--an anatomical classification. J Plast Reconstr Aesthet Surg. 2007;60(4):372-8. doi: 10.1016/j.bjps.2006.10.005. Epub 2007 Jan 19. PMID: 17349591.


