Summary Card
Definition
A Seymour fracture is an open, displaced distal phalangeal physeal fracture with an associated nailbed injury.
Anatomy
They present as mallet fingers with a flexion deformity due to the level of flexor and extensor tendons at the distal phalanx.
Clinical Features
Crush injuries associated with a nail plate avulsion and proximal nail bed interposition at the fracture site.
Investigations
X-rays are required for adequate diagnosis with distinct features seen on the lateral view.
Treatment
Treatment is multimodal and involves irrigation, debridement, reduction, fixation, and antibiotics.
Complications
Include osteomyelitis, nail dystrophy, non-union or malunion, and growth disturbances of the distal phalanx.
Primary Contributor:
Dr Waruguru Wanjau, Educational Fellow, South Africa.
Reviewer:
Dr Suzanne Thomson, Educational Fellow, Scotland.
Definition of Seymour Fracture
A Seymour fracture is an open, displaced distal phalangeal physeal fracture with an associated nailbed injury.
A Seymour fracture is a displaced, open fracture of the juxta-epiphyseal region of the distal phalanx, with an overlying nail bed injury that occurs in skeletally immature individuals.
The image below illustrates a Seymour fracture.
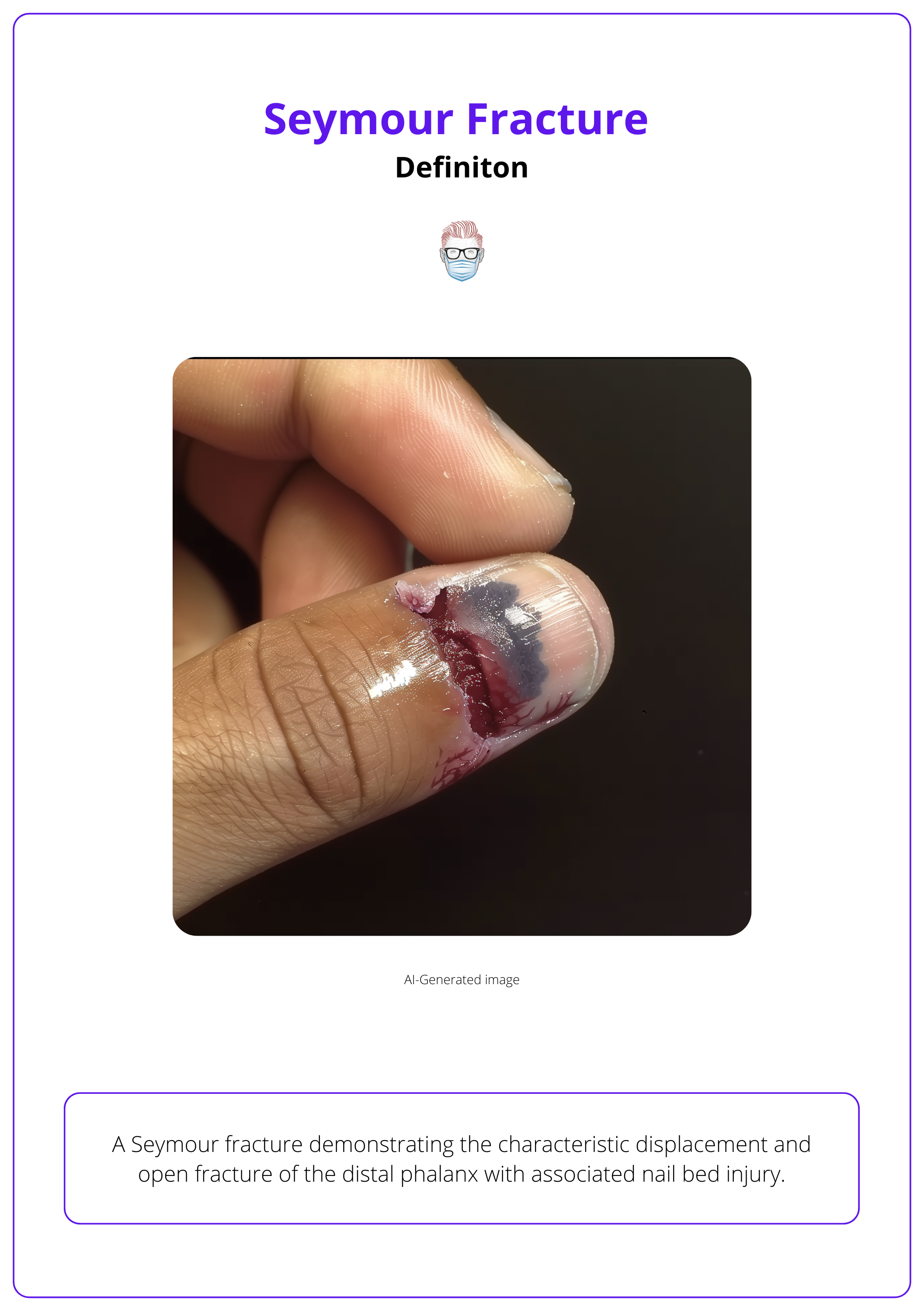
It is associated with the avulsion of the nail plate and a concomitant laceration of the nail bed due to the proximity of the nail bed to the fracture site. It presents as either:
- Salter-Harris Type I
- Salter-Harris Type II
- "Juxta-epiphyseal" occurs at the metaphysis, slightly distal to the physis
Seymour Fractures are often mis-diagnosed. Always be careful of a proximal nail bed injury!
Anatomy of Seymour Fracture
Seymour fractures are caused by crushing injuries and present as mallet fingers with a flexion deformity.
The Seymour Fracture is considered a bony and soft tissue injury. In relation to the bone, there is a predisposition for this fracture in the distal phalanx (Krusche-Mandl, 2013) due to:
- Weakness of the epiphyseal-metaphyseal junction.
- Angulation of the diaphysis on the epiphysis.
- Insertion sites of the flexor and extensor tendons into the distal phalanx.
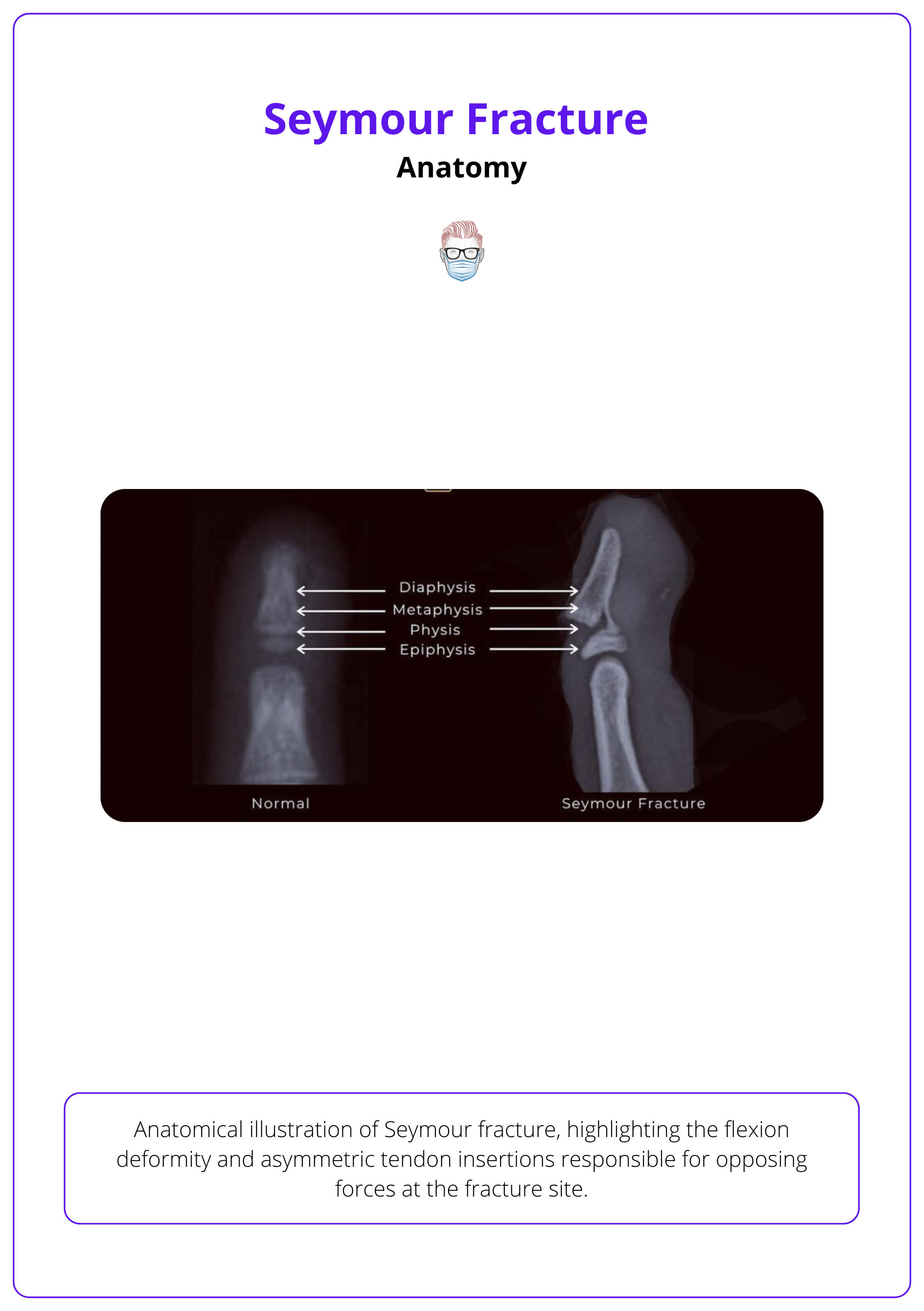
The injury presents as a pseudomallet, characterized by a flexion deformity of the distal phalanx, due to asymmetric tendon insertions.
- Extensor tendon attaches to the epiphysis of the proximal fracture fragment.
- FDP tendon attaches to the metaphysis of the distal fragment.
This configuration results in opposing forces at the fracture site, which hinders proper healing. The image below illustrates the anatomy of the Seymour Fracture.
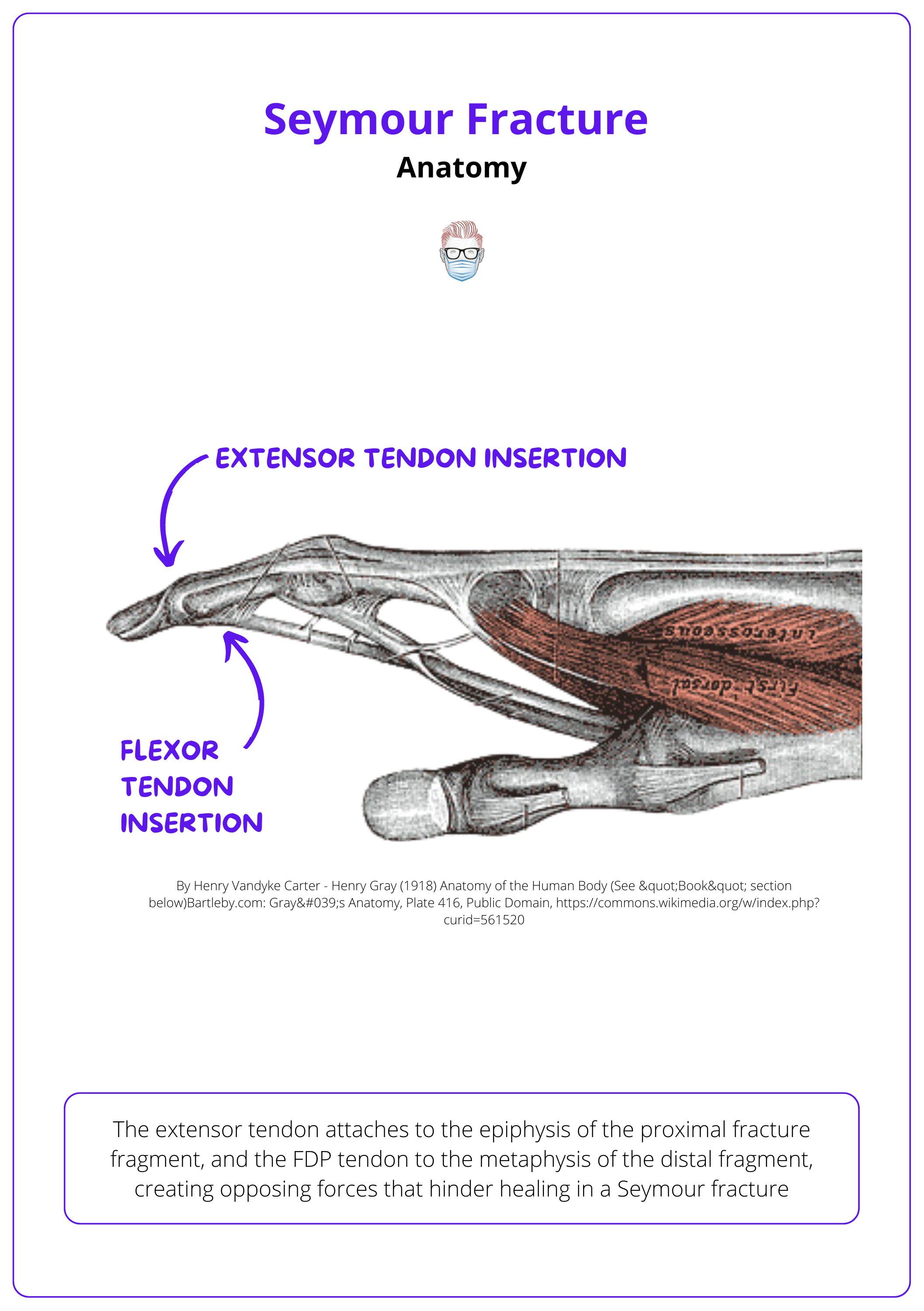
Extensor tendon rupture is uncommon in children because the epiphyseal plate is weaker than the tendon (Krushe-Manndl, 2013).
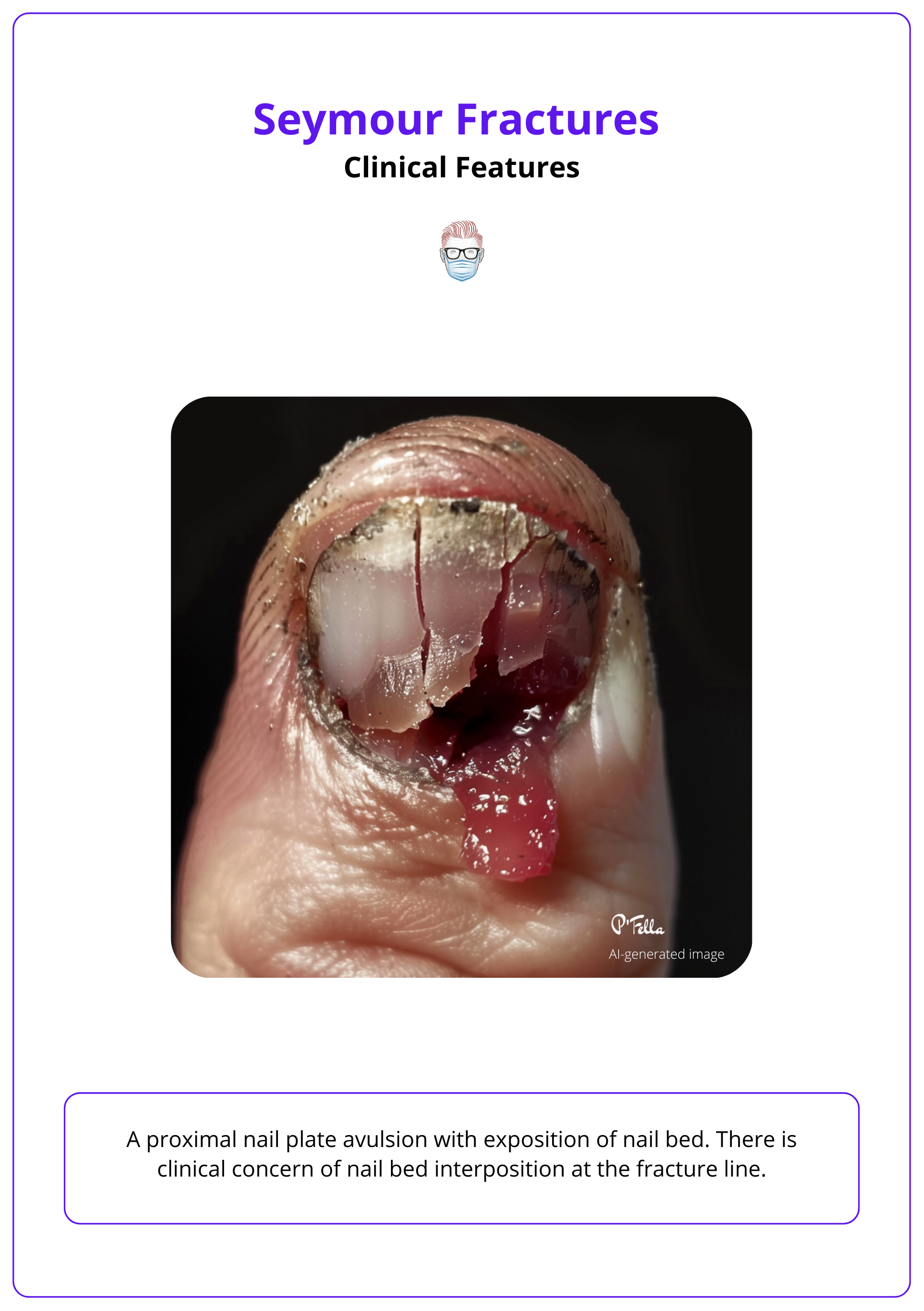
Clinical Features of Seymour Fracture
Seymour fractures have a variety of presentations from subtle nailbed injuries to grossly displaced and exposed fractures. It can be commonly misdiagnosed.
A Seymour Fracture has a typical history of a crush injury. In terms of clinical examination, common findings include:
- Nail bed injury with an avulsed nail plate (often lying superficial to the eponychial fold)
- Skin laceration
- 'Pseudomallet' deformity due to flexion forces > extensor forces.
- Elongation of the lunula.
Investigations for Seymour Fracture
X-rays, especially the lateral view are key to identifying Seymour fractures.
The identification of Seymour fractures is key to ensuring adequate and appropriate treatment. X-ray is the imaging modality of choice, key radiological findings are:
- Posteroanterior: may appear normal.
- Lateral: widened physis or displacement between epiphysis and metaphysis. They may also be a flexion deformity at the fracture site.
The image below illustrates Seymour fracture on the lateral view of an X-ray.

A lateral x-ray distinguishes between an extensor tendon rupture and a juxta-epiphyseal Seymour fracture.
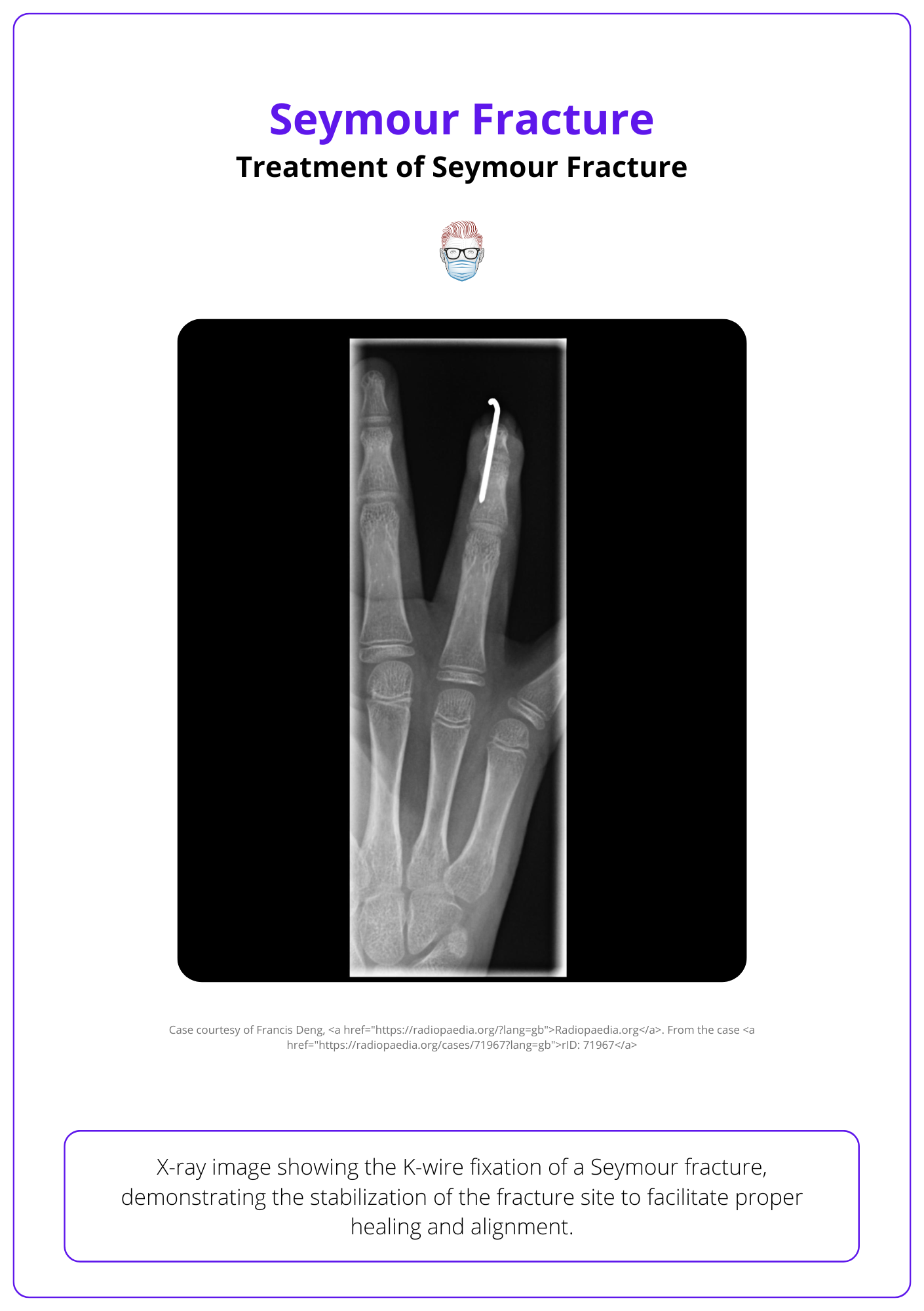
Treatment of Seymour Fracture
Treatment is multimodal and involves irrigation, debridement, reduction, fixation, and antibiotics.
Treatment is multimodal and involves irrigation, debridement, reduction, fixation, and antibiotics (Krushe-Manndl, 2013). The recommended management of Seymour fractures can be looked at from both a soft tissue and bone perspective (Lin, 2019):
Soft Tissue Repair:
- Nail plate removal.
- Extraction of the germinal matrix entrapped at the fracture site through hyperflexion of the digit or distal fragment retraction
- Irrigation and selective debridement
Fracture reduction.
- K-wire if the fracture is unstable or concern of patient non-compliance.
- Splinting the DIPJ if stable fracture after reduction and compliant patient.
- Tip: The nail aids in stable reduction by acting like a splint
It is worth noting, other techniques have been described. For example, late infected Seymour fractures can be treated by a one-suture technique that holds the distal phalanx in place. This technique avoids the need for K-wires in the setting of infection (Englert, 2022).
The absence of fracture healing can be seen on radiographs - by trabecular bone or callus bridging across the fracture site (Samade, 2021).
Complications of Seymour Fracture
Complications include osteomyelitis, nail dystrophy, non-union or malunion, and growth disturbances of the distal phalanx.
The primary concern regarding Seymour Fractures is the interposition of the germinal matrix is between fracture fragments - resulting in Osteomyelitis, Non-union, or Malunion.
Factors that lead to increase complications include:
- Delayed Treatment
- Insufficient debridement.
- Incomplete fracture reduction.
- Inadequate antibiotic treatment.
A Seymour fracture presenting after 24 hours is considered a delayed fracture and has a greater risk of infection (Samade, 2021). An algorithm for the approach for delayed Seymour fractures can be found here.
Premature physeal closure is usually due to infection rather than direct injury to the growth plate (Lin, 2019).
Conclusion
1. Definition and Anatomy of Seymour Fractures: You've learned that a Seymour fracture is an open, displaced distal phalangeal physeal fracture with an associated nail bed injury, commonly occurring in children.
2. Causes and Presentation of Seymour Fractures: You now understand that these fractures often result from crushing injuries and are characterized by symptoms such as mallet fingers with a flexion deformity at the distal phalanx.
3. Seymour Fracture Diagnostic Approaches: You're aware that X-rays, particularly lateral views, are crucial in diagnosing Seymour fractures.
4. Treatment Modalities for Seymour Fractures: You've learned about treatment approaches for Seymour fractures, which includes irrigation, debridement, reduction, fixation, and antibiotics.
5. Potential Complications of Seymour Fractures: You understand possible complications such as osteomyelitis, nail dystrophy, non-union or malunion, and growth disturbances.
Further Reading
- Perez-Lopez LM, Parada-Avendaño I, Cabrera-Gonzalez M, Fontecha CG. Seymour fracture: Better do not underestimate it. Jt Dis Relat Surg. 2021;32(3):569-574. doi: 10.52312/jdrs.2021.330. Epub 2021 Nov 19. PMID: 34842086; PMCID: PMC8650660.
- Kiely AL, Nolan GS, Cooper LRL. The optimal management of Seymour fractures in children and adolescents: a systematic review protocol. Syst Rev. 2020 Jun 23;9(1):150. doi: 10.1186/s13643-020-01407-5. PMID: 32576259; PMCID: PMC7313162.
- Krusche-Mandl I, Köttstorfer J, Thalhammer G, Aldrian S, Erhart J, Platzer P. Seymour fractures: retrospective analysis and therapeutic considerations. J Hand Surg Am. 2013 Feb;38(2):258-64. doi: 10.1016/j.jhsa.2012.11.015. PMID: 23351909.
- Seymour N. Juxta-epiphysial fracture of the terminal phalanx of the finger. J Bone Joint Surg Br. 1966 May;48(2):347-9. PMID: 5939484.
- Lin JS, Popp JE, Balch Samora J. Treatment of Acute Seymour Fractures. J Pediatr Orthop. 2019 Jan;39(1):e23-e27. doi: 10.1097/BPO.0000000000001275. PMID: 30358692.
- Samade R, Lin JS, Popp JE, Samora JB. Delayed Presentation of Seymour Fractures: A Single Institution Experience and Management Recommendations. Hand (N Y). 2021 Sep;16(5):686-693. doi: 10.1177/1558944719878846. Epub 2019 Oct 9. PMID: 31597480; PMCID: PMC8461200.
- Reyes BA, Ho CA. The High Risk of Infection With Delayed Treatment of Open Seymour Fractures: Salter-Harris I/II or Juxta-epiphyseal Fractures of the Distal Phalanx With Associated Nailbed Laceration. J Pediatr Orthop. 2017 Jun;37(4):247-253. doi: 10.1097/BPO.0000000000000638. PMID: 26327401.
- Farid M, Shibu M. A rare case of Seymour fracture in an adult with non-fused growth plates. Case Reports Plast Surg Hand Surg. 2021 May 19;8(1):72-75. doi: 10.1080/23320885.2021.1927738. PMID: 34104672; PMCID: PMC8143599.
- Englert EG, Tooley T, Weisz K, Shapiro P. Suture Fixation of Subacute Pediatric Seymour Fractures. J Hand Surg Glob Online. 2022 Dec 7;5(2):231-233. doi: 10.1016/j.jhsg.2022.10.013. PMID: 36974281; PMCID: PMC10039310.
- Abzug JM, Kozin SH. Seymour fractures. J Hand Surg Am. 2013 Nov;38(11):2267-70; quiz 2270. doi: 10.1016/j.jhsa.2013.08.104. PMID: 24206995.


