Summary Card
Causes of Septic Arthritis
Septic arthritis of the hand is caused by direct inoculation into the joint space, spread from surrounding infection, or hematogenous spread.
Clinical Presentation of Septic Arthritis
Clinically septic arthritis of the hand presents as a swollen, warm, erythematous, and painful joint.
Septic Arthritis Diagnosis
Diagnosis is based on clinical, radiological (X-rays, ultrasound, and MRI), and laboratory findings (bloodwork WBC, CRP, ESR, and arthrocentesis when possible).
Treating Septic Arthritis
Treatment of septic arthritis requires a combination of surgical debridement, antibiotics, and rehabilitation.
Complications
Septic Arthritis can result in joint stiffness, chronic infections, and persistent pain.
Primary Contributor:
Dr Waruguru Wanjau, Plastic Surgery Trainee, South Africa.
Reviewer:
Dr Suzanne Thomson, Plastic Surgeon, Scotland.
Causes of Septic Arthritis
Septic arthritis of the hand can arise from direct inoculation through trauma or medical procedures, local spread, or less commonly through hematogenous spread.
Septic arthritis of the hand can originate from several sources. It may develop from an infection spreading locally from surrounding tissues, or through hematogenous spread from distant sites. Direct inoculation can occur due to trauma or as a complication following surgical procedures.
In regards to the specific joints involved in septic arthritis and their aetiology:
- DIPJ: flexor tenosynovitis, felon, mucous cyst, or paronychia.
- PIPJ: flexor tenosynovitis.
- MCPJ: human bite during a fight (fight bite).
- Haematogenous: rare, usually immunocompromised adults.
Patient risk factors for septic arthritis include advanced age, rheumatoid arthritis, diabetes, and immunosuppression (Earwood, 2021).
Clinical Presentation of Septic Arthritis
Clinically septic arthritis of the hand presents as a swollen, warm, erythematous, painful joint.
Septic Arthritis can present with local and systemic signs and symptoms.
Local signs include:
- Skin changes: swelling, warmth, erythema
- Pain: pain during active motion, passive motion, and rest
Systemic symptoms suggest haematogenous spread. These symptoms include:
- Fevers, chills, malaise
- Sepsis
These signs and symptoms may not be present in patients with immunosuppressed patients or those with prosthetic joints - they may present with loosening in prosthetic joints.
Septic Arthritis Diagnosis
Diagnosis is based on clinical, radiological (X-rays, ultrasound, and MRI), and laboratory findings (bloodwork WBC, CRP, ESR ± arthrocentesis).
The diagnosis of septic arthritis of the hand is based on clinical observations, laboratory investigations, and imaging (Chenoweth, 2020).
Bloods
Laboratory blood work includes:
- Inflammatory Markers: WBC, CRP, and ESR. The trend in inflammatory markers can be used to monitor treatment response, with CRP often lagging a little behind WBC.
- Blood cultures are indicated in the event of pyrexia, and may be indicative of sepsis or haematogenous spread.
Staphylococcus aureus is the most common causative factor in blood cultures.
Imaging
The imaging modalities that can be used to evaluate septic arthritis are X-Ray, ultrasound, and MRI.
X-rays
Obtain 2 or more views of the affected joint.
- Can be used to evaluate for a retained foreign object, osteomyelitis.
- Two to three weeks post onset one may see signs characteristic of osteomyelitis, such as osteolysis osteopenia, osteosclerosis, periosteal reaction, and sequestration (Lipatov, 2022).
This can be visualised in the image below.

Ultrasound:
- Can detect intra-articular effusion.
- If joint aspiration, request gram stain and culture, cell count, crystal analysis, protein level, and glucose level.
Retained foreign objects can induce chemical synovitis that resembles an infectious process.
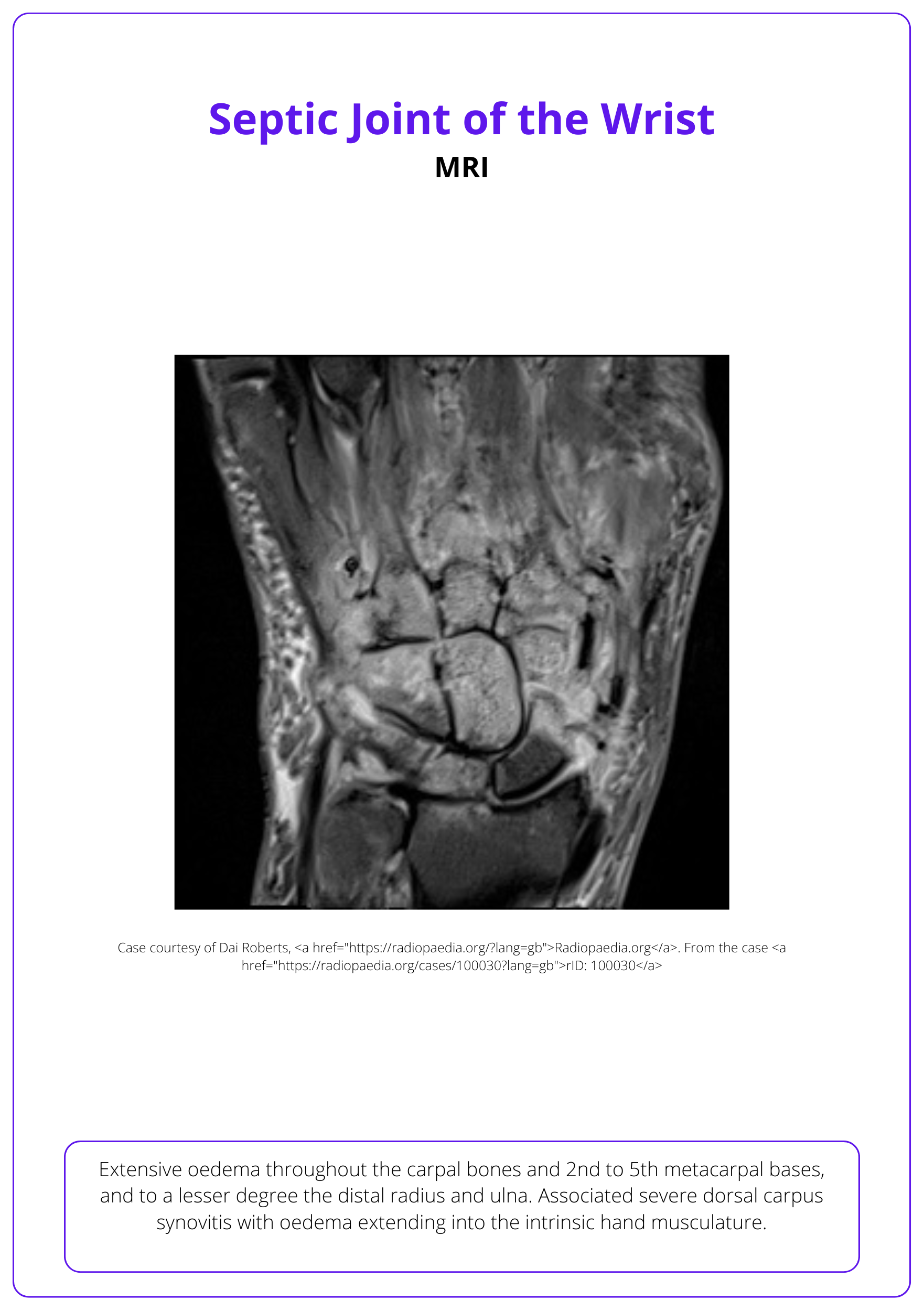
MRI:
When necessary can visualize joint effusion, its distribution, and the destruction of soft tissues and osteochondral structures of the joint.
This can be visualised in the image below.
The below figure illustrates the algorithm for the workup of patients with acute onset of joint pain (Chenoweth, 2020).
For a detailed algorithmic approach to the investigatons/work of septic arthritis, please read this article by Chenoweth, 2020.
Treating Septic Arthritis
Treatment of septic arthritis is a combination of surgical treatment, antibiotics, and rehabilitation.
Septic arthritis requires a multi-modal treatment approach of surgical washout/debridement, antibiotics, and rehabilitation.
Surgical Washout
Septic Arthritis is a surgical emergency that requires an urgent washout of the affected joint. Each joint has a particular surgical approach. General principles include:
- Large volume irrigation of the affected joint.
- Debridement of infection/non-viable tissue.
- Delayed treatment of other injuries (eg: An extensor tendon/sagittal band injury in an MCPJ septic arthritis post fight-bite).
- Tissue/Pus sent for microbiology, culture and sensitivity.
If signs of infection continue and inflammatory markers do not show a downward trend then repeat debridement is recommended within 24-48 hours after the index procedure.
Adjuncts to Surgical Treatment
Surgery is the primary treatment. Additional adjuncts can include:
- Antibiotics for 2-4 weeks based on the sensitivities of the cultures.
- Hand Therapy: early active mobilisation to attempt to restore of the function of the affected joint.
Starting rehabilitation for a range of motion exercises following surgery is shown to reduce this stiffness. (Chenoweth, 2020).
Complications
Septic arthritis can cause joint stiffness, chronic infections, and persistent pain, potentially requiring surgical intervention
Complications of septic arthritis relate to the range of movement, chronic infections, and pain. More specifically:
- Stiffness: this is the most common complication. This can relate to soft tissues (eg collateral ligament contractures) or from the articular destruction of the joint (arthritis)
- Chronic/Persistent Infections: osteomyelitis, abscess, multiple surgeries.
- Chronic Pain: this primarily relates to arthritic changes in the joint. In these patients, arthrodesis or arthroplasty of the specific joint may be required.
Treatment of these complications depends on the specific issue. For example, if the articular cartilage is damaged, arthrodesis can be primarily or as a secondary arthrodesis 4−6 wk after the primary revision. Arthrodesis and amputation are significantly higher in diabetic and immunosuppressed individuals (Giuffre, 2011).
Paediatric patients can have an associated growth plate injury.
Conclusion
1. Basics of Septic Arthritis: You have acquired a detailed understanding of the causes, clinical presentation, and diagnostic methods for septic arthritis of the hand, essential for recognizing this condition in clinical settings.
2. Treatment Approaches: You are now familiar with the current treatment strategies for septic arthritis, including the importance of prompt surgical debridement, the appropriate use of antibiotics, and the role of rehabilitation in recovery.
3. Recognized Importance of Early Intervention: The article emphasized the critical nature of early diagnosis and intervention to prevent the progression of the infection and minimize long-term damage to the joint and function.
4. The Role of Rehabilitation: You understand that rehabilitation is crucial in restoring function and range of motion in the affected joint after the initial acute management.
5. Awareness of Complications: You have learned about the potential complications associated with septic arthritis.
Further Reading
- Earwood JS, Walker TR, Sue GJC. Septic Arthritis: Diagnosis and Treatment. Am Fam Physician. 2021 Dec 1;104(6):589-597. PMID: 34913662.
- Lipatov KV, Asatryan A, Melkonyan G, Kazantcev AD, Solov'eva EI, Cherkasov UE. Septic arthritis of the hand: Current issues of etiology, pathogenesis, diagnosis, treatment. World J Orthop. 2022 Jul 18;13(7):622-630. doi: 10.5312/wjo.v13.i7.622. PMID: 36051375; PMCID: PMC9302027.
- Giuffre JL, Jacobson NA, Rizzo M, Shin AY. Pyarthrosis of the small joints of the hand resulting in arthrodesis or amputation. J Hand Surg Am. 2011 Aug;36(8):1273-81. doi: 10.1016/j.jhsa.2011.05.022. Epub 2011 Jun 25. PMID: 21705153.
- Chenoweth B. Septic Joints: Finger and Wrist. Hand Clin. 2020 Aug;36(3):331-338. doi: 10.1016/j.hcl.2020.03.006. PMID: 32586459.


