Summary Card
Definition
Schwannomas are benign tumors arising from Schwann cells, often causing pain, numbness, or weakness due to nerve compression.
Clinical Features
Schwannomas are encapsulated peripheral nerve tumours, within the epineurium and often associated with a single nerve fascicle.
Investigations
Schwannomas are best characterised by T2 weighted MRI.
Management
Surgical excision is indicated for symptomatic lesions or uncertain diagnosis. The recurrence of a Schwannoma is extremely rare and the prognosis is excellent.
Primary Contributor: Dr Suzanne Thomson, Educational Fellow.
Reviewer: Dr Kurt Lee Chircop, Educational Fellow.
Definition of Schwannomas
Schwannomas are benign tumors arising from Schwann cells, which form the myelin sheath around axons.
A Schwannoma is a benign, isolated peripheral nerve lesion with no malignant potential. These benign tumors develop from Schwann cells, which form the myelin sheath around axons and are crucial for effective nerve signal transmission.
These tumors typically originate from a single nerve fascicle within the protective endoneurium layer.

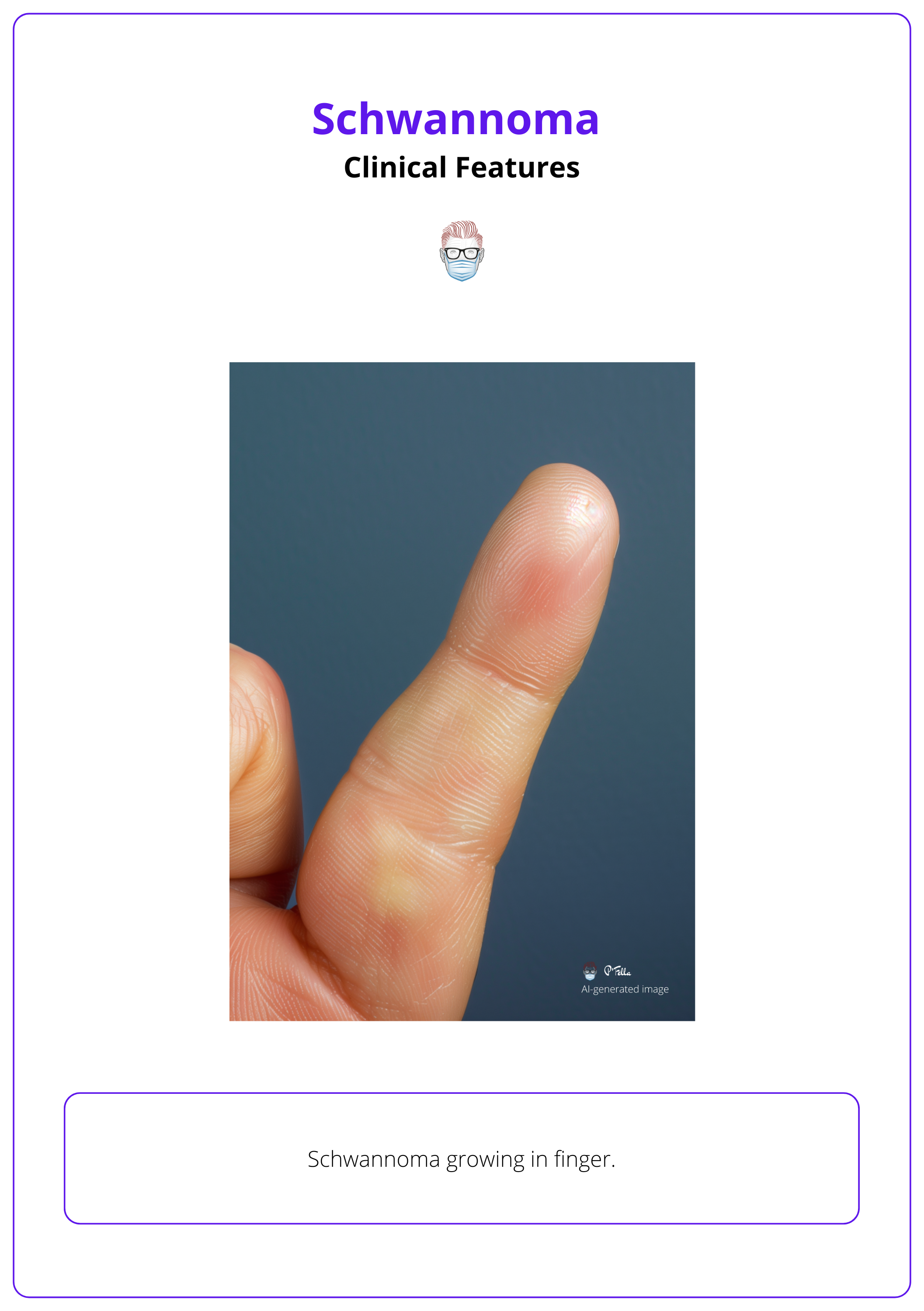
Clinical Features of Schwannomas
Schwannomas are typically solitary, painless, slow-growing lesions that can cause radiating pain upon palpation. Their growth may displace and compress adjacent nerves, causing pain, numbness, or weakness.
Typical Presentation
Schwannomas are benign tumors originating from Schwann cells, presenting with several distinct clinical features:
- Solitary Nature: Typically appearing as solitary, painless, and slow-growing lesions.
- Palpation or compression of the lesion can produce radiating pain in a specific nerve distribution.
- Mass Effect: The tumor's growth can displace and compress adjacent nerves, leading to pain, numbness, or weakness, depending on its location.
- Location Variability: These tumors are most commonly found in the retroperitoneal and abdominal wall areas, though they occur less frequently in the head, neck, and extremities. (Lam, 2019)
The lesion is often mobile in a transverse direction but not longitudinally.
Genetic Associations
Schwannomas frequently manifest in individuals with genetic disorders such as:
- Neurofibromatosis: NF1 is Characterized by early childhood onset, presenting with café-au-lait spots, Lisch nodules, and other systemic symptoms.
- Schwannomatosis: Often involves multiple schwannomas without the presence of vestibular tumors.
There are 4 descriptions of nasal tip schwannoma in the literature (presumably associated with the anterior ethmoidal nerve) that can be managed with open rhinoplasty technique (Fujita, 2006).
Differential Diagnosis
Differentiating schwannomas from other nerve tumors is crucial, as these can be benign or malignant:
Benign Tumors
- Neurofibromas: These are the most common peripheral nerve tumors. Specific types, such as plexiform, intraneural, and large nerve neurofibromas, are considered pre-malignant.
- Lipomas: Occurring both intra- and extraneural, these tumors can cause compression neuropathies and displacement. Intraneural lipomas, encapsulated by the epineurium, may impair blood supply leading to atrophy of Schwann cells and axons.
Malignant Tumors:
- Malignant Peripheral Nerve Sheath Tumors (MPNST): These rare tumors account for less than 1% of all sarcomas and are notable for their rapid growth, pain, and poor prognosis. They typically respond poorly to chemoradiotherapy.
The plural form is Schwannomata, but Schwannomas is more commonly used.
Investigations for Schwannomas
US and MRI are useful in characterising Schwannomas, hyperintense well-circumscribed lesions on T2 weighted MRI.
Schwannomas are a radiological and histological diagnosis confirmed after a high index of clinical suspicion.
Radiological
MRI is the preferred imaging modality, providing detailed information on nerve structure and tumor biology (Eraky 2023). More specifically:
- T2-weighted MRI: Schwannomas typically appear as hyperintense, well-circumscribed lesions.
- Ultrasound (US): is useful in the initial characterisation of Schwannomas. Non-invasive and readily accessible.
- CT and X-ray are not useful in the characterisation of Schwannoma due to their inability to provide detailed information about soft tissue structures.
Histopathology
Histological diagnosis can be obtained through excisional or tru-cut biopsies.
- Excision Biopsy: Considered the diagnostic modality of choice. Provides definitive diagnosis through histopathological examination.
- Tru-Cut Biopsy: Useful when resection is associated with significant morbidity or when malignancy is suspected. (Hems, 2024). Minimally invasive and can help in preoperative planning.
On anaylsis of these histology specimens:
- Stain positively for S100 and SOX10 immunostains.
- These tumors are encapsulated
- Pathognomonic presence of Antoni A (spindle cells and eosinophilic cytoplasm) and Antoni B (relatively acellular) areas.
Of note, several pathological subtypes such as "ancient type" schwannomas have been described, all strongly positive for S100 and Sox10 on immunostaining.
Heterogeneity in T2 weighted MRI signal indicates Schwannoma and reflects the Antoni A (low signal) and B (high signal) areas within the lesion. The target sign is characteristic of neurofibroma.
Management of Schwannoma
Schwannoma resection is indicated for pain and mass effect symptoms. Careful dissection allows these encapsulated tumours to be "shelled out".
Schwannomas are generally considered to have no malignant potential, making the primary indications for excision:
- Pain
- Mass effect symptoms
Surgical management of Schwannomas carefully dissects or "shells out" these encapsulated tumors from the surrounding nerve, often with excellent preservation of function. In the overwhelming majority of cases, the lesion can be completely removed, and any preoperative neurologic symptoms are likely to improve.
Practical tips for surgery include:
- Utilize optical magnification and microsurgical techniques to reduce the risk of postoperative neurologic deficit.
- Be aware that interfascicular involvement may complicate dissection.
- The incidence of postoperative neurologic deficit ranges from approximately 5% to 15%, with a significantly higher risk associated with procedures performed after incisional biopsy or in cases of recurrence.
Recurrence of Schwannomas is uncommon, although multiple lesions in a single peripheral nerve have been described.
Schwannoma surgery can be likened to peeling the layers of an onion skin. A microscope or a high-powered loupes and beaver blade allow meticulous dissection.
Conclusion
1. The Anatomy of a Peripheral Nerve: You've learned about the peripheral nervous system (PNS), including motor and sensory neurons, nerve axons, Schwann cells, and the protective layers (endoneurium, perineurium, and epineurium).
2. Clinical Characteristics and Histopathology of Nerve Tumors: You understand the key features of benign and malignant nerve tumors, particularly Schwannomas, including their presentation, genetic associations, and histopathological characteristics.
3. Pathogenesis of Schwannomas: You've explored how Schwannomas originate from Schwann cells, their growth patterns, and the symptoms they cause due to nerve compression.
4. Diagnostic Investigations for Schwannomas: You are familiar with the imaging techniques used to characterize Schwannomas and the role of biopsy techniques in diagnosing these tumors.
5. Management and Prognosis of Schwannomas: You've gained insight into the management strategies for Schwannomas, including indications for surgical excision, the typical excellent prognosis post-resection, and the rarity of recurrence.
Further Reading
- Hems T, Parafioriti A, Thomas BP, Di Bernardo A. An algorithmic approach to the management of peripheral nerve tumours. J Hand Surg Eur Vol. 2024 Mar 27:17531934241238739. doi: 10.1177/17531934241238739. Epub ahead of print. PMID: 38534080.
- Fujita K, Yuzuriha S, Noguchi M. 'Cyrano de Bergerac' nose deformity caused by the schwannoma of the nasal tip. J Plast Reconstr Aesthet Surg. 2006;59(11):1252-4. doi: 10.1016/j.bjps.2006.03.059. Epub 2006 Jun 6. PMID: 17046644.
- Lam R, Hunt BL, Arreola-Owen O. Abdominal Wall Schwannoma. Fed Pract. 2019 Mar;36(3):129-133. PMID: 30983853; PMCID: PMC6453606.
- Graf A, Yang K, King D, Dzwierzynski W, Sanger J, Hettinger P. Lipomas of the Brachial Plexus: A Case Series and Review of the Literature. Hand (N Y). 2019 May;14(3):333-338. doi: 10.1177/1558944717735946. Epub 2017 Oct 23. PMID: 29058949; PMCID: PMC6535949.
- Eraky AM, Beck RT, Treffy RW, Aaronson DM, Hedayat H. Role of Advanced MR Imaging in Diagnosis of Neurological Malignancies: Current Status and Future Perspective. J Integr Neurosci. 2023 May 15;22(3):73. doi: 10.31083/j.jin2203073. PMID: 37258452.


