Summary Card
Overview
Rotation flaps are curvilinear pivotal flaps that incorporate both pivotal and advancement movements, making them ideal for triangular defect repair.
Indications & Contraindications
Rotation flaps are indicated for lateral facial, cheek, chin, and scalp reconstruction and can be contraindicated in cases of residual malignancy, and high hemorrhage risk.
Design & Execution
The success of a rotation flap depends on precise defect triangulation, appropriate flap circumference, and optimal pivot point positioning to ensure proper tension distribution and closure.
Design Variations
Ahuja’s and Sandhir’s flaps adjust the pivot point to improve reach and tension distribution, allowing for shorter flaps in lax skin while ensuring optimal scar placement along aesthetic subunits.
Complications
Postoperative care should focus on hematoma prevention, tension distribution, and vascular monitoring to ensure optimal healing. Limited movement and sun protection can reduce complication
Updated by: Dr Waruguru Wanjau, Educational Fellow.
Verified by thePlasticsFella ✅
Overview of Rotation Flap Design
Rotation flaps are curvilinear pivotal flaps that incorporate both pivotal and advancement movements, making them ideal for triangular defect repair.
Rotation flaps are curvilinear pivotal flaps commonly used to reconstruct defects without creating a secondary donor site. Their design prioritizes tension distribution, flap geometry, and pivot positioning to optimize defect coverage (Baker, 2022).
Principles of Rotation Flap Design
- Curvilinear pivotal flap that moves around a fixed pivot point.
- Best suited for triangular defects (Baker, 2022).
- Reduces tension by redistributing forces along a curved arc.
- Particularly useful for areas at risk of distortion, such as the eyelid and lips.
Rotation flap design is illustrated below.
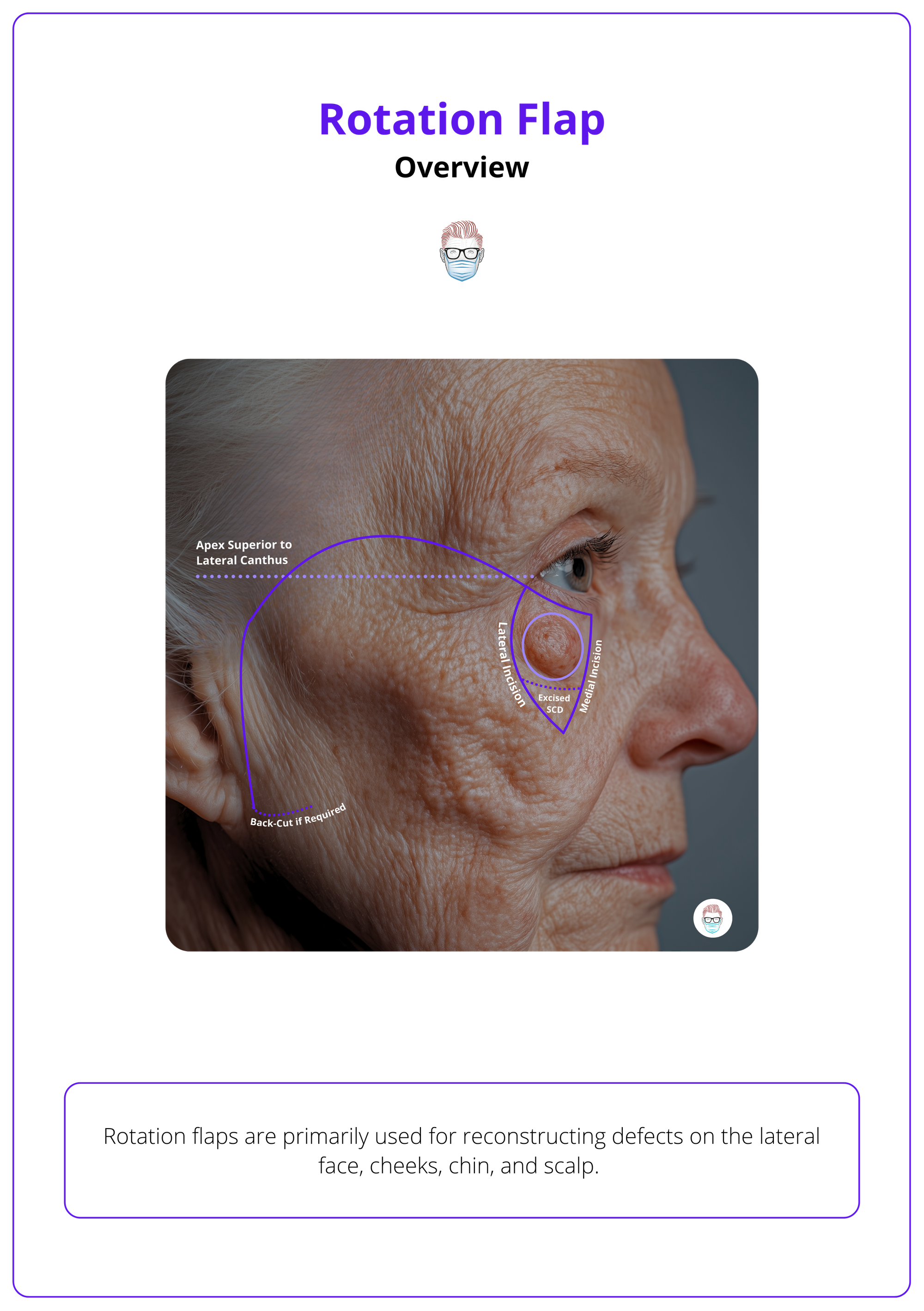
Rotation flaps redirect tension around free margins, minimizing distortion in delicate areas like the eyebrow and lips (Prohaska, 2023).
Indications & Contraindications of Rotation Flap
Rotation flaps are primarily used for reconstructing defects on the lateral face, cheeks, chin, and scalp. They are relatively contraindicated in cases of residual malignancy, high hemorrhage risk, and active smoking.
Rotation flaps are ideal when primary closure is not possible due to excessive tension or risk of distortion. They are commonly used for,
- Scalp
- Lateral Face
- Cheeks
- Chin
These flaps are particularly useful for redirecting tension around free margins, preventing distortion in areas such as the eyebrows and lips.
The areas and their dimensions are summarized in the table below.
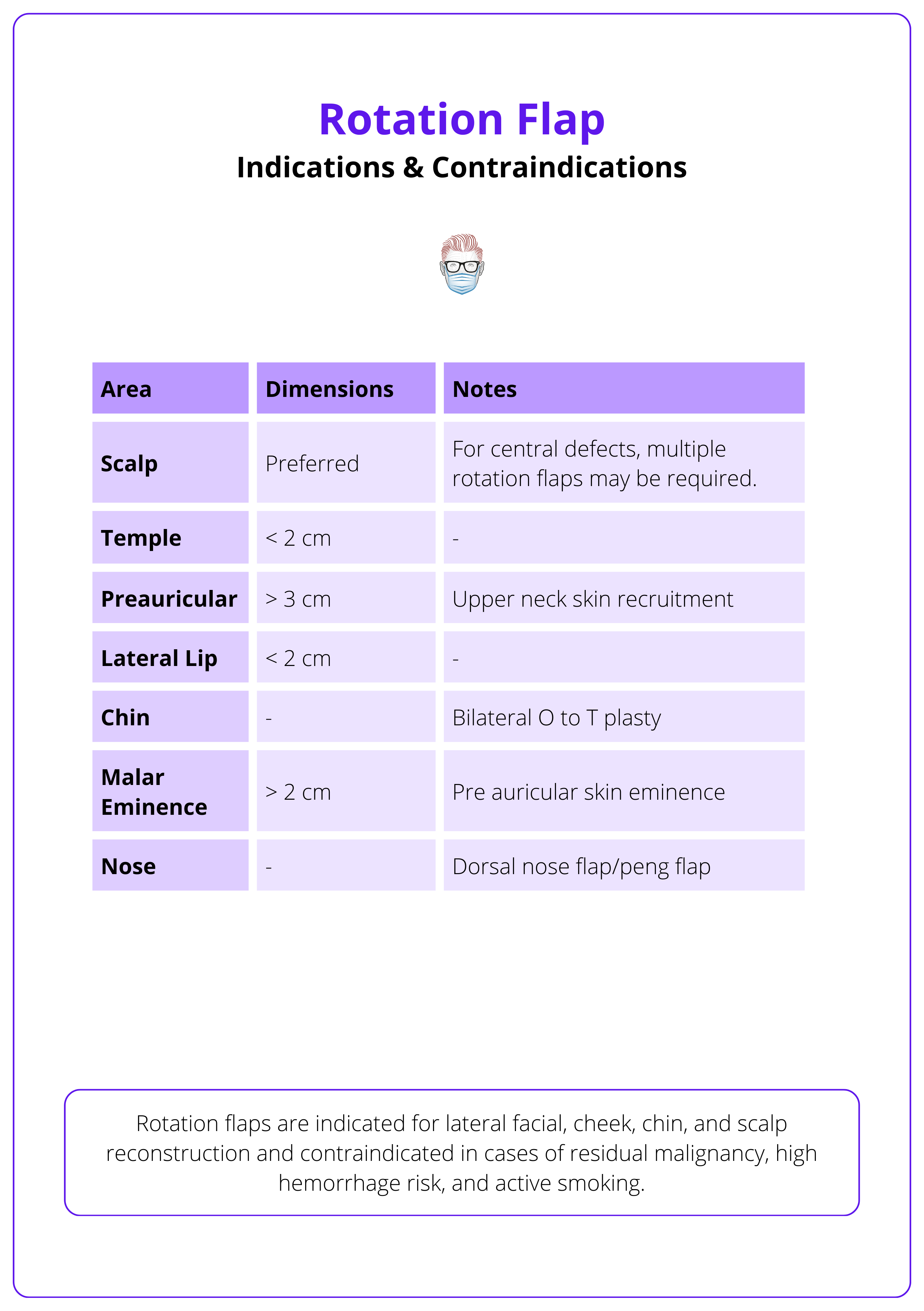
Contraindications
Rotation flaps are contraindicated if a malignancy is not completely cleared and relatively contraindicated in an increased risk of hemorrhage and active smoking.
- Absolute Contraindications: Residual malignancy (requires complete excision, such as Mohs micrographic surgery).
- Relative Contraindications: an increased risk of hemorrhage, particularly in anticoagulated patients, and active smoking, which can compromise vascular supply and healing. Proper rotation flap geometry and tension management are essential to ensure optimal outcomes and minimize complications.
Several named rotation flaps, such as Tenzel and Mustardé flaps, are designed for specific locations and indications.
Design & Execution of a Rotation Flap
The success of a rotation flap depends on precise defect triangulation, appropriate flap circumference, and optimal pivot point positioning to ensure proper tension distribution and closure.
A rotation flap follows a structured design to ensure optimal reach, minimal tension, and reliable closure by triangulating the defect, determining the pivot point, drawing an arc, and making strategic adjustments.
A rotation flap design is illustrated below.
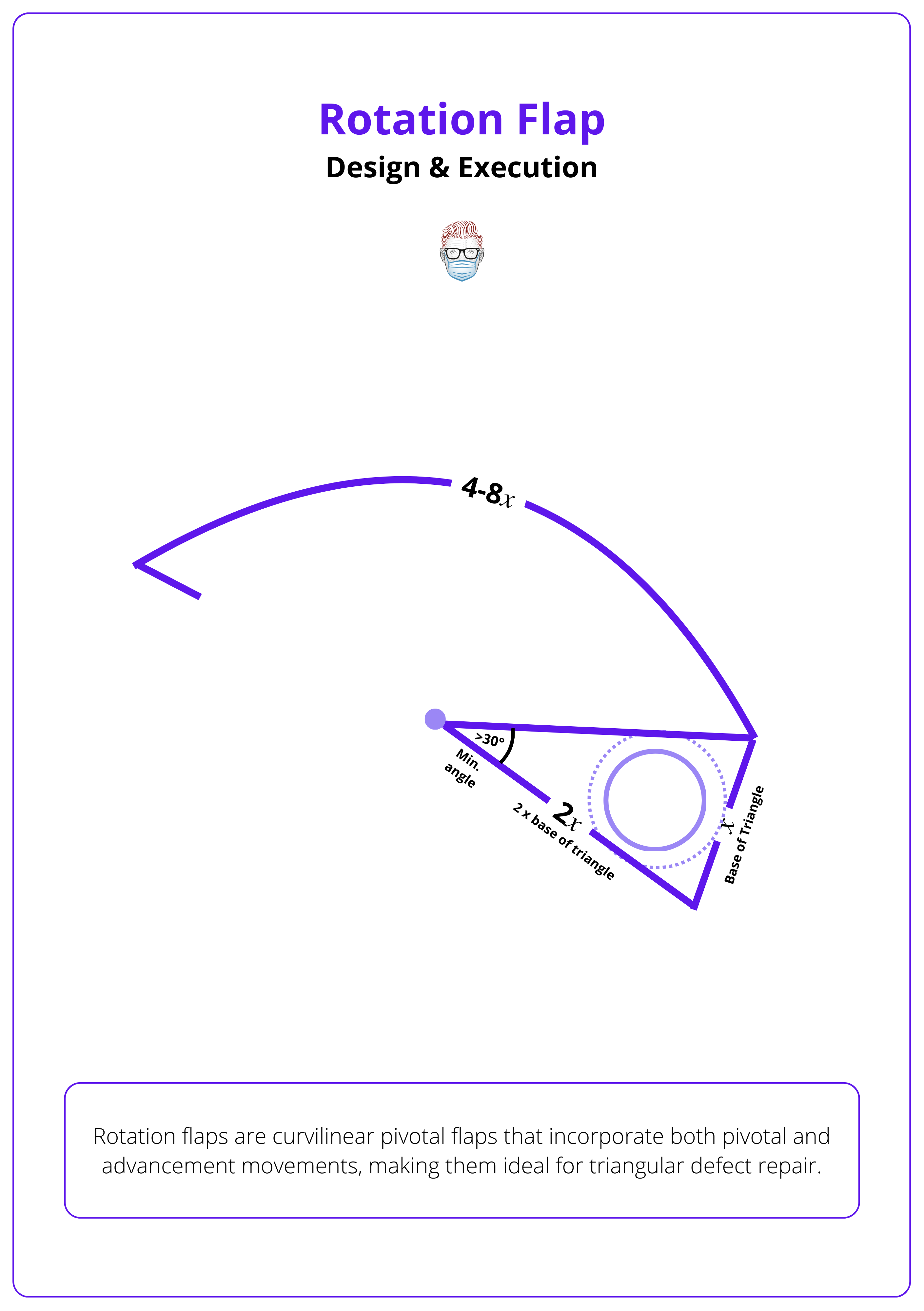
Step 1: Triangulate the Defect
Isosceles triangle is more symmetrical and aligns better with semicircular flaps than a right-angled triangle (Lo, 2008). Key factors include:
- Base of Triangle: Slightly wider than the defect, this is 𝑥.
- Sides of Triangle: Sides ~2× defect width, this is 2𝑥.
Step 2: Identify Pivot Point
The geometrical pivot point is the center of the semicircular flap, ideally aligned with the apex of the triangulated defect. There is often confusion about pivot points, as there are two additional types.
- Functional Pivot Point: Origin of the line of tension, determining how the flap moves.
- Anteriorly Displaced Pivot Point: Increases closing tension, making flap advancement more difficult.
Increasing triangle length reduces defect width and angle, increasing flap radius and facilitating closure.
Step 3: Draw An Arc
There is no fixed flap size, but classical references (McGregor, 2000 & Smith, 1979) suggest a flap circumference of 5–8× the defect width or 4–5× the defect base length. This “5× rule” comes from π, since the flap follows a semicircular path when it rotates.
- Arc Length = π×radius (where radius = 2𝑥 and π ≈3)
- Therefore, Arc Length = 3 x 2𝑥 = 6𝑥
However, some tissue is lost at the base, reducing the effective arc length to ~5𝑥. Rotation arcs beyond 90° provide diminishing tension relief.
As flap circumference increases, the benefit of tension reduction decreases.
Step 4: Incision & Elevation
Incising and elevating the flap properly ensures vascular preservation and mobility. Key factors include,
- Incision Path: Follow the semicircular design, ensuring smooth rotation.
- Elevation Plane: Elevate the flap in the subdermal or subgaleal plane to preserve vascularity.
- Undermining: Improves flap movement but should be wide yet controlled to avoid disrupting blood supply.
- Rotate: Gently rotate the flap into the defect, ensuring even tension distribution.
Inferiorly-based flaps are preferred as they promote lymphatic drainage and reduce post-op edema.
Step 5: Alterations to Reduce Tension
Reducing tension improves flap mobility and closure. Key techniques include,
- Back-Cut: Moves pivot point closer, increases reach; use cautiously in vascularly compromised areas.
- Burow’s Triangle Excision: Small triangular excision near pivot; modestly improves mobility.
- Z-Plasty: Placed at flap base to increase mobility; may replace Burow’s triangle excision (Baker, 2022).
- Undermining: Enhances movement; must balance range of motion with vascular preservation.
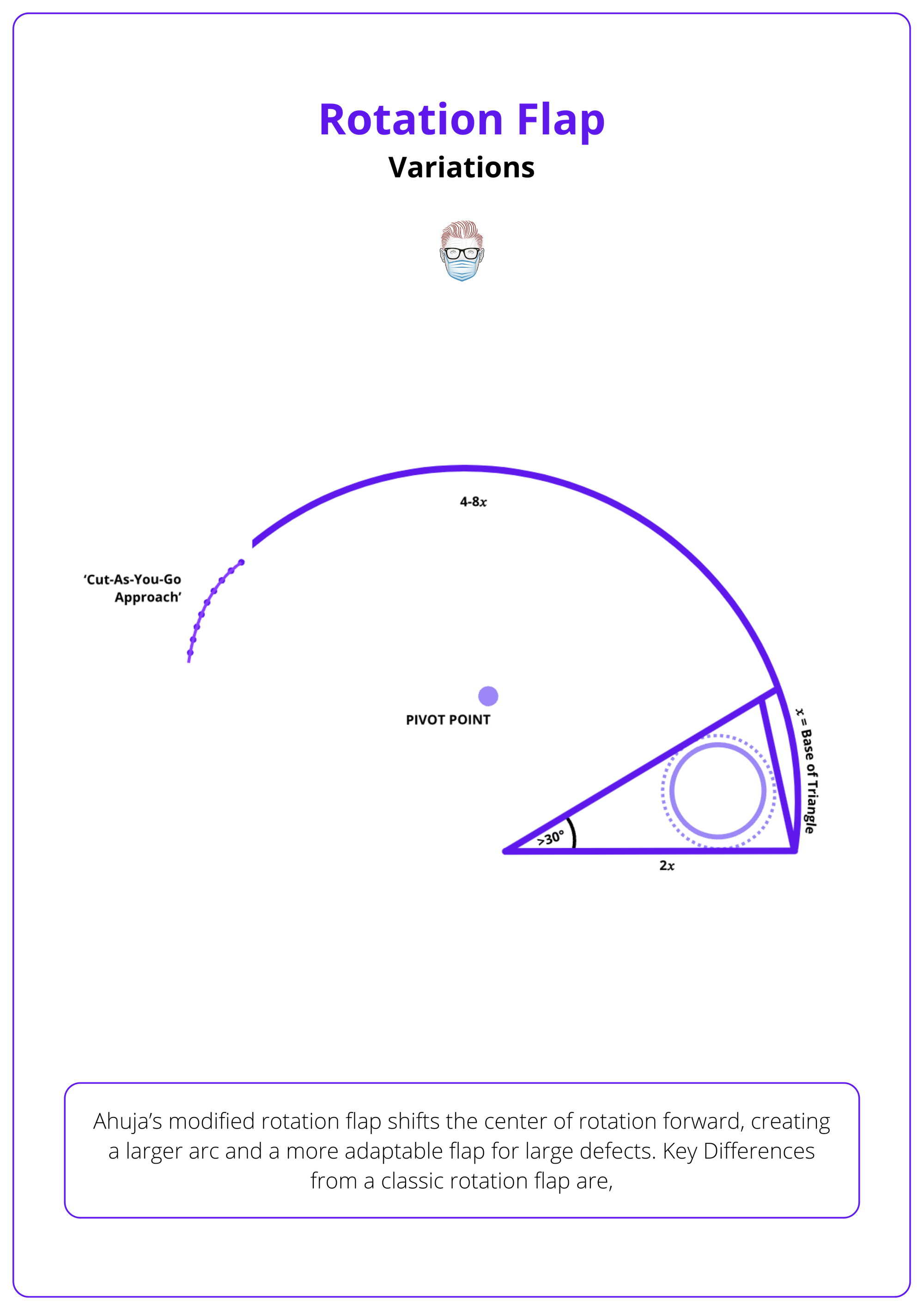
Variations of Rotation Flap Design
Ahuja’s and Sandhir’s flaps adjust the pivot point to improve reach and tension distribution, allowing for shorter flaps in lax skin while ensuring optimal scar placement along aesthetic subunits.
Variations of the classical rotation flap improve mobility, tension distribution, and adaptability, making them ideal for complex reconstructions. Ahuja’s and Sandhir’s modifications are designed to enhance reach, flexibility, and closure reliability, optimizing defect coverage with minimal tension.
Ahuja’s Modified Rotation Flap (1988)
This technique shifts the center of rotation forward, creating a larger arc and a more adaptable flap for large defects. Key Differences from a classic rotation flap are,
- Pivot Point Modification: The triangular defect is mirrored, establishing a new pivot point further from the defect. This allows for a longer, more mobile flap with less tension, making it ideal for large defects.
- Flap Length & Flexibility: The extended arc increases reach, ensuring better defect coverage. The flap end remains adjustable intraoperatively, allowing a cut-as-you-go approach for optimal closure.
This flap design is illustrated below.
Sandhir’s Divine Rotation Flap (1997)
This modification enhances control and flexibility by incorporating geometric shapes into the flap design.
- Geometric Pivot Adjustment: A rectangle and square are added around the defect, with the pivot point recalculated by bisecting these shapes, rather than using the standard fixed pivot.
- Improved Reach & Tension Distribution: The flap rotates from a new pivot point, reducing tension and allowing intraoperative extension if needed.
- Greater Flexibility: The geometric design enhances movement precision, enabling flap length adjustments during surgery for a better fit.
Other Modifications
Several other minor modifications enhance closure, tension distribution, and adaptability for specific anatomical regions.
- Double Rotation Flap: Two opposing arcs extend from the same point, used when a single flap is insufficient; ideal for forehead, lip, and chin defects (Albom, 1978).
- O-Z Rotation Flap: Two counter-rotating flaps create a Z-shaped scar, preferred for scalp defects; not to be confused with Z-plasty.
- Modified Peng Flap: A double rotation flap for nasal defects, pivoting from the nasal root; avoids forehead flaps but may distort nasal symmetry (Prohaska, 2023).
- Tenzel Flap: A semicircular flap involves rotation of skin and orbicularis muscle from the area superior to the lateral canthus to fill defects of the lower lid and incorporates lysis of the lateral canthal tendon to increase tissue mobility → Lower eyelid defects (Tenzel, 1978).
- Mustardé Flap: A similar design in which a broad sweeping rotation is arched superiorly from the lateral canthus, through the temple, and ending in the preauricular sulcus → Large cheek/lower eyelid defects (Mustarde, 1970).
Complications of Rotation Flaps
Postoperative care should focus on hematoma prevention, tension distribution, and vascular monitoring (if needed) to ensure optimal healing. Limited movement and sun protection can reduce complication
Proper tension distribution, vascular monitoring, and postoperative care are essential to prevent complications. Early intervention minimizes the risk of functional and aesthetic issues
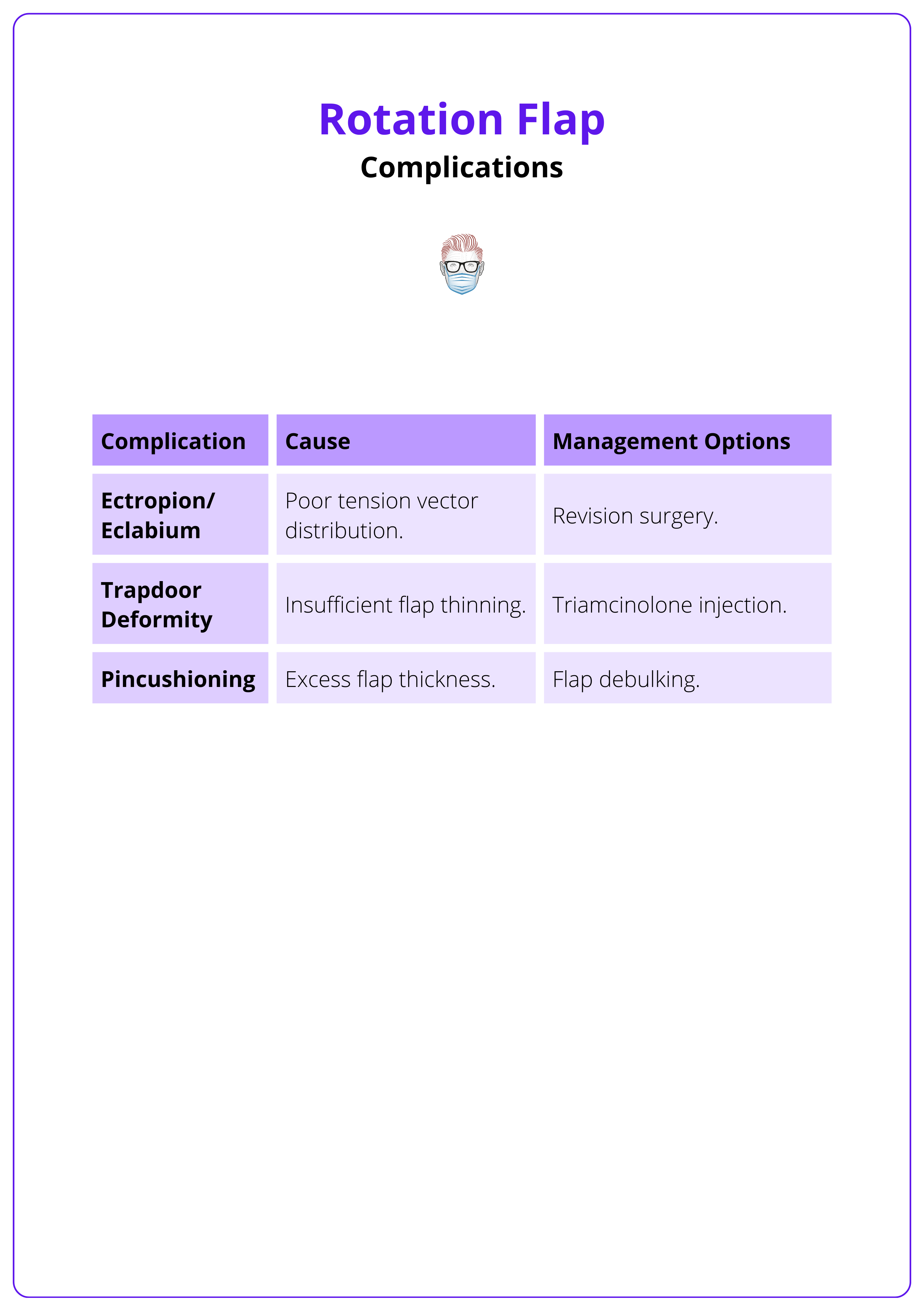
Complications are uncommon but include,
- Haematoma formation, usually in the first 24 hours.
- Ectropion/Eclabium: Caused by poor tension vector distribution; managed with revision surgery.
- Trapdoor Deformity: Results from insufficient flap thinning; treated with triamcinolone injection.(Baker, 2022).
- Pincushioning: Excess flap thickness; corrected with flap debulking.
Complications, their causes, and management are detailed in the table below.
Conclusion
1. Overview: Rotation flaps are pivotal, curvilinear flaps designed to repair triangular defects while minimizing tension and distortion, particularly in delicate areas like the eyelids and lips.
2. Indications & Contraindications: Used for lateral facial, cheek, chin, and scalp defects. Contraindications include incomplete tumor excision, high hemorrhage risk, and active smoking.
3. Flap Design & Tension Management: Proper triangulation, adequate flap circumference, and optimal pivot point positioning reduce closure stress. Tension is managed through back-cuts, Burow’s triangles, Z-plasty, and wide-undermining.
4. Postoperative Care & Complications: Hematoma prevention, activity restriction, and sun protection are key for healing. Common issues include trapdoor deformity and excessive tension.
5. Flap Modifications: Variants like double rotation flaps, O-Z plasty, and Peng/Mustardé/Tenzel flaps improve outcomes based on defect location and complexity.
Further Reading
- Lo CH, Kimble FW. The ideal rotation flap: an experimental study. Journal of Plastic, Reconstructive & Aesthetic Surgery. July 2008:754-759. doi:10.1016/j.bjps.2007.12.032
- Ahuja R. Geometric considerations in the design of rotation flaps in the scalp and forehead region. Plast Reconstr Surg. 1988;81(6):900-906. doi:10.1097/00006534-198806000-00012
- Albom M. Repair of large scalp defects by bilateral rotation flaps. J Dermatol Surg Oncol. 1978;4(12):906-907. doi:10.1111/j.1524-4725.1978.tb00578.x
- Tenzel R, Stewart W. Eyelid reconstruction by the semicircle flap technique. Ophthalmology. 1978;85(11):1164-1169. doi:10.1016/s0161-6420(78)35578-0
- Mustardé J. The use of flaps in the orbital region. Plast Reconstr Surg. 1970;45(2):146-150. https://www.ncbi.nlm.nih.gov/pubmed/5411895.
- Starkman SJ, Williams CT, Sherris DA. Flap Basics I: Rotation and Transposition Flaps. Facial Plast Surg Clin North Am. 2017 Aug;25(3):313-321. doi: 10.1016/j.fsc.2017.03.004. Epub 2017 May 30. PMID: 28676159
- Baker, S.R., 2021. Rotation Flaps Chapter 7, 100-123.e1 Local flaps in facial reconstruction E-book.
- Prohaska J, Sequeira Campos MB, Cook C. Rotation Flaps. [Updated 2023 Aug 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482371/


