Summary Card
Definition
Rare median nerve compression in the proximal forearm, mostly in middle-aged females.
Anatomy
Median nerve compression at five distinct locations causes pronator syndrome.
Clinical Features
Typically presents with forearm pain, positive Tinel sign at the elbow, and no night symptoms.
Management
Primarily conservative treatment with rest and splinting. Surgical decompression is reserved for cases that fail to resolve with conservative measures.
Primary Contributor: Dr Kurt Lee Chircop, Educational Fellow.
Reviewer: Dr Waruguru Wanjau, Educational Fellow.
Definition of Pronator Syndrome
Pronator Syndrome is a compressive neuropathy of the median nerve in the proximal forearm.
Pronator Syndrome is a compressive neuropathy of the median nerve at the level of the elbow, as it passes from the arm to the forearm.
It is a rare form of neuropathy of the median nerve. Key facts include:
- An incidence of <10% of all median nerve entrapments.
- Tends to affect females in the 5th decade of life
- Increased risk with well-developed arm muscles (Ruiz, 2023).
The basic anatomy of pronator syndrome is illustrated below.
Pronator syndrome is commonly associated with medial epicondylitis.
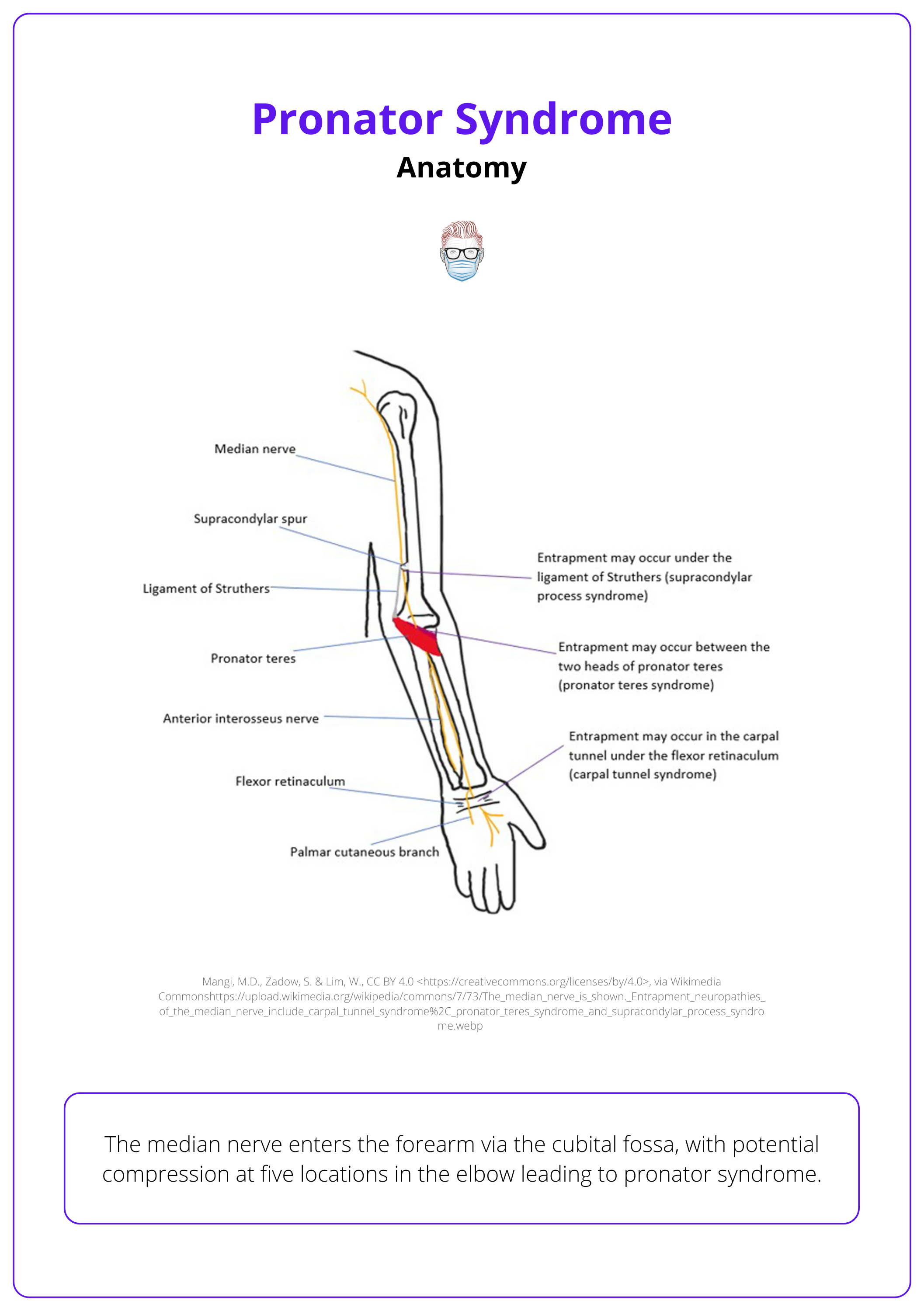
Anatomy of Pronator Syndrome
The median nerve enters the forearm via the cubital fossa, with potential compression at five locations in the elbow leading to pronator syndrome.
Median nerve is formed from the medial and lateral cords of the brachial plexus, representing C6-T1 nerve roots.
Its course in the upper limb is:
- Travels through the axilla and down the arm, lateral to brachial artery.
- Enters forearm via the cubital fossa and comes to lie between FDS + FDP muscle bellies, after passing between the two heads of pronator teres.
- Gives off anterior interosseous nerve in the forearm + palmar cutaneous branch before passing through the carpal tunnel terminating as the recurrent and palmar digital branches (Drake, 2020).
Compression at the elbow, giving rise to pronator syndrome, may occur at 5 distinct locations:
- Between the ulnar and humeral heads of pronator teres: commonest aetiology.
- Supracondylar process: a residual bony structure of the distal humerus present in 1% of the population.
- Ligament of Struthers: connective tissue band extending from the supracondylar process to the medial epicondyle.
- Bicipital aponeurosis (Lacertus fibrosus): thickened aponeurosis of the biceps brachii at the elbow.
- FDS aponeurotic arch (Balcerzak, 2022).
Additional rarer sites of nerve compression:
- The accessory head of the flexor pollicis longus (Gantzer muscle)
- Exostoses of the radius
- The ulnar segment of the flexor carpi ulnaris muscle
- The brachialis muscle and its fascial bands (Balcerzak, 2022).
The anatomy of the upper limb concerning pronator syndrome is illustrated below.
Ligament of Struthers is not to be confused with Arcade of Struthers, which is a thin aponeurotic band in the arm originating from the brachial fascia, that can cause an ulnar nerve entrapment (Loukas, 2010).
Clinical Features of Pronator Syndrome
Pronator syndrome presents as median nerve distribution parestheisa, pain in the volar arm, and positive tinel signs in the volar forearm.
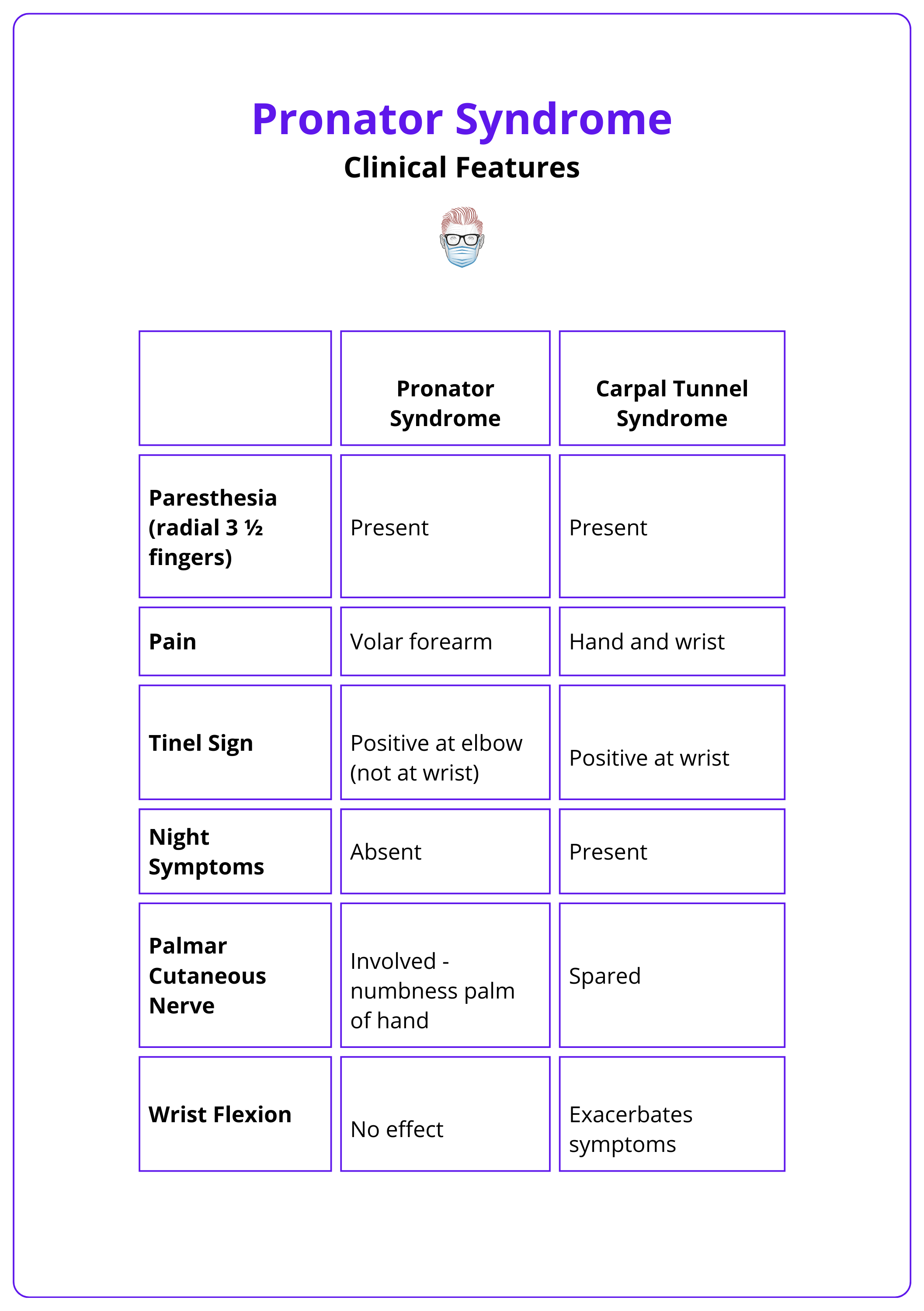
The clinical features of pronator syndrome share similarities with other compressive neuropathies of the median nerve. However, distinct findings help in distinguishing pronator syndrome from its primary differential diagnosis, carpal tunnel syndrome (CTS).
Typical findings include:
- Paresthesia: Tingling or numbness in the radial 3 ½ fingers, often exacerbated by repeated pronation and supination.
- Aching Pain: Felt over the proximal volar forearm.
- Positive Tinel sign in the proximal volar forearm
The palmar cutaneous branch of the median nerve originates 4-5 cm proximal to the carpal tunnel, and is therefore spared in CTS.
A summary of clinical findings of pronator syndrome vs carpal tunnel syndrome is outlined in the table below (Balcerzak, 2022).
Provocative tests for different entrapment sites can aid in the diagnosis, but lack specificity and sensitivity (Adler, 2020):
- Compression at Pronator Teres: Resisted forearm pronation with the elbow extended.
- Compression at Bicipital aponeurosis: Resisted elbow flexion with forearm supination.
- Compression at FDS aponeurotic arch: Resisted contraction of the FDS to the middle finger.
Investigations are performed as part of routine workup but diagnosis remains a clinical one.
- Radiographs: Elbow X-rays may show a supracondylar process.
- EMG: confirms diagnosis if positive, but is usually equivocal.
Anterior interosseous syndrome (AIN) is another type of compressive median nerve neuropathy characterised by pure motor palsy without sensory symptoms. This key feature differentiates AIN from pronator syndrome, which often presents with predominantly sensory disturbances (Krishnan, 2020).
Management of Pronator Syndrome
Treatment for pronator syndrome is primarily conservative, with surgery considered for persistent symptoms and significant functional impairment.
Treatment is primarily conservative, with surgery being considered only for persistent symptoms and significant functional impairment.
Non-operative
Suitable for patients with mild to moderate symptoms.
- Rest, Splinting, and NSAIDs: Administer for 3-6 months.
- Technique: Splint should prevent forearm pronation/supination.
Operative
Surgical decompression of the median nerve is considered when nonoperative management fails after 3-6 months. Important points include:
- Involves decompression of the median nerve at all five potential compression sites.
- Approach is usually open but endoscopic release has been described (Sos, 2021).
- Complications include scarring, contracture, infection, medial cutaneous nerve injury.
Conclusion
1. Understanding Pronator Syndrome: You've understood Pronator Syndrome and its clinical definition as a rare median nerve compression in the proximal forearm, affecting predominantly middle-aged females.
2. Anatomical Knowledge: You've learned about the anatomy related to Pronator Syndrome, including the five potential compression sites of the median nerve in the proximal forearm.
3. Clinical Recognition: You've explored the clinical features of Pronator Syndrome, such as forearm pain, a positive Tinel sign at the elbow, and the absence of night symptoms, and can differentiate it from other similar neuropathies.
4. Diagnostic Insight: You are familiar with the diagnostic approach for Pronator Syndrome, emphasizing physical examinations, and supported by imaging and electrodiagnostic tests to confirm the diagnosis.
5. Management Strategies: You've understood the primary conservative treatment approaches including rest and splinting, and the criteria for when surgical intervention may be necessary.
Further Reading
- Ruiz, Emmanuel Stephano Bracho. "Pronator Syndrome and Other Nerve Compressions That Mimic Carpal Tunnel Syndrome a Case Report and Literature Review." SAR J Surg 4.3 (2023): 31-35.
- Sos C, Roulet S, Lafon L, Corcia P, Laulan J, Bacle G. Median nerve entrapment syndrome in the elbow and proximal forearm. Anatomic causes and results for a 55-case surgical series at a mean 7 years' follow-up. Orthop Traumatol Surg Res. 2021 Apr;107(2):102825. doi: 10.1016/j.otsr.2021.102825. Epub 2021 Jan 28. PMID: 33516890.
- Drake, Richard L., et al. Gray's Atlas of Anatomy E-Book: Gray's Atlas of Anatomy E-Book. Elsevier Health Sciences, 2020.
- Balcerzak AA, Ruzik K, Tubbs RS, Konschake M, Podgórski M, Borowski A, Drobniewski M, Olewnik Ł. How to Differentiate Pronator Syndrome from Carpal Tunnel Syndrome: A Comprehensive Clinical Comparison. Diagnostics (Basel). 2022 Oct 8;12(10):2433. doi: 10.3390/diagnostics12102433. PMID: 36292122; PMCID: PMC9600501.
- Loukas, Marios, et al. "Sir John Struthers (1823–1899) and his ligament and arcade." Neurosurgery 66.6 (2010): 1170-1173.
- Adler, Jeremy A., and Jennifer Moriatis Wolf. "Proximal median nerve compression: pronator syndrome." The Journal of Hand Surgery 45.12 (2020): 1157-1165.
- Krishnan KR, Sneag DB, Feinberg JH, Wolfe SW. Anterior Interosseous Nerve Syndrome Reconsidered: A Critical Analysis Review. JBJS Rev. 2020 Sep;8(9):e2000011. doi: 10.2106/JBJS.RVW.20.00011. PMID: 32890049.


