Summary Card
Definition
An acquired condition causing progressive wasting of skin, soft tissue and bone.
Clinical Features
Progressive unilateral wasting in the trigeminal region begins in early adolescence and stabilises over time.
Management
Radiological investigations help support the diagnosis and reconstruction to restore atrophied function and structures.
Definition of Progressive Hemifacial Atrophy
Progressive hemifacial atrophy is a rare, acquired disorder marked by unilateral, sporadic wasting of the facial skin, soft tissues, and bone, with unknown aetiology and typically no family history.
Progressive hemifacial atrophy is an acquired condition characterised by gradual wasting of facial skin, soft tissue and bone. The majority of cases are unilateral, sporadic and without a family history.
The exact aetiology is relatively unknown. The image below further describes the definition and origin of progressive hemifacial atrophy.
Clinical Features of Progressive Hemifacial Atrophy
Progressive hemifacial atrophy is the progressive wasting of skin, soft tissue, and one in the trigeminal regions. Other features include pigmentation, coup de sabre, and seizures.
Progressive hemifacial atrophy is characterised by progressive soft tissue and bone wasting. General speaking, there are "rules of thumb", which include:
- Distribution of the trigeminal nerve.
- Gradually progresses and then gradually stops over time.
- It is irreversible without intervention.
- Signs begin to manifest in early adolescence and stop in adulthood.
The image below illustrates the clinical features of progressive hemifacial atrophy.
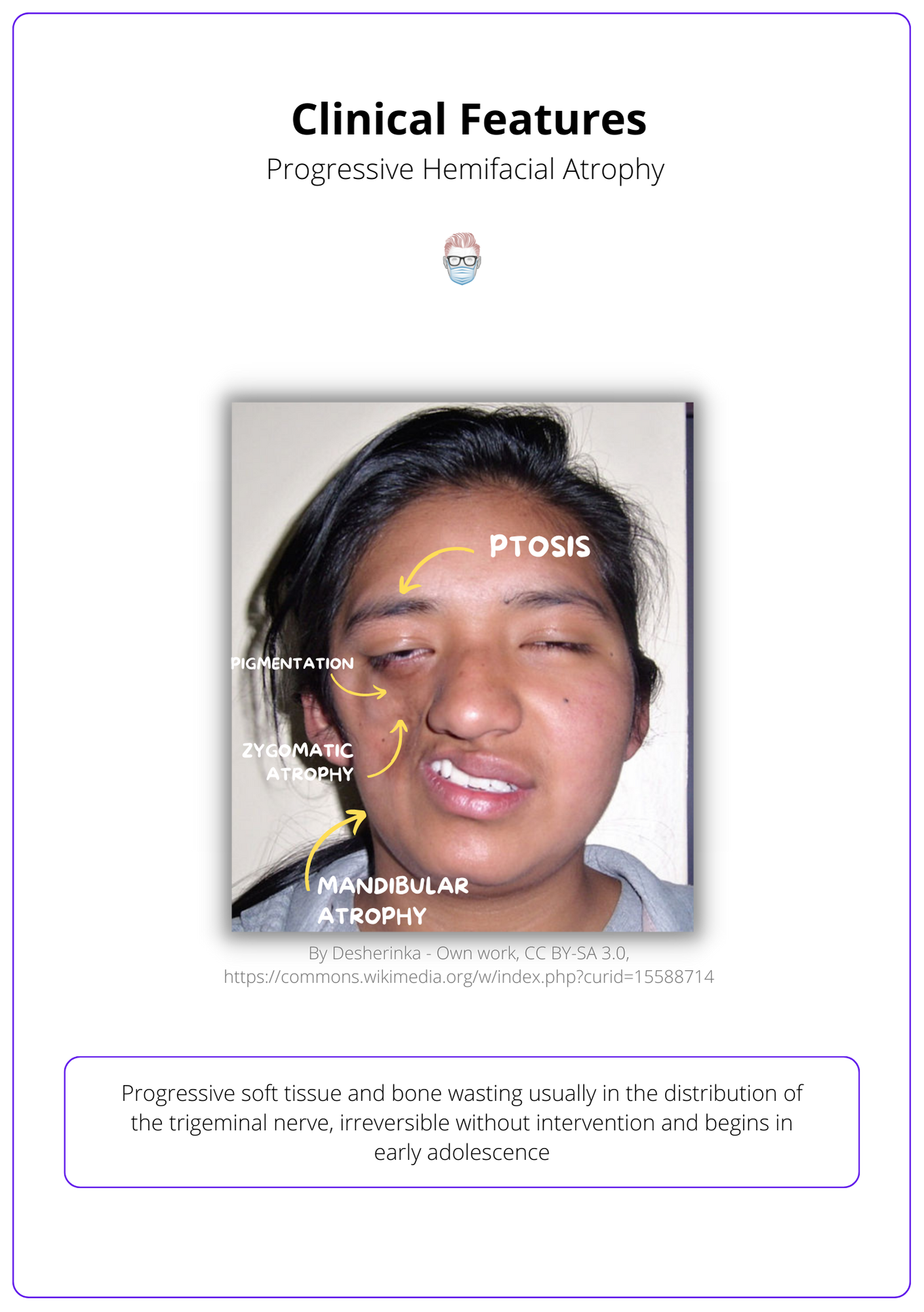
Clinical features of progressive hemifacial atrophy include:
- Hair: loss or change in colour
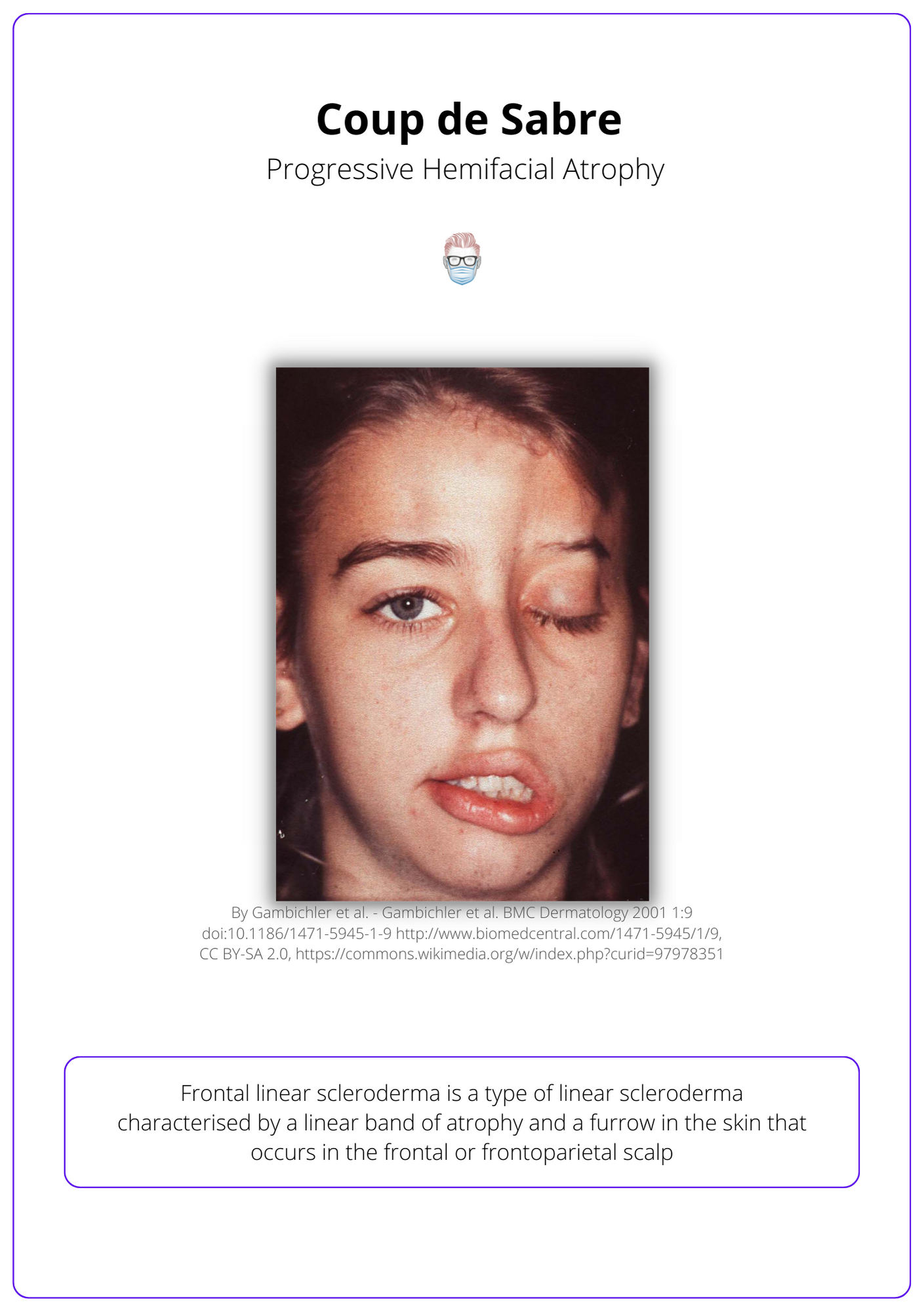
- Forehead: 'coupe de sabre' (forehead depression extending into hairline)
- Eyes: ptosis, enophthalmos, heterochromia irides (2 different eye colours)
- Cheek: Zygomatic atrophy, atrophy of masticators
- Mandible: Micrognathia
- Skin: pigment changes
- Mouth: Malocclusion, tongue or palate atrophy
- Non-physical signs: seizures
The image below illustrates coup de sabre of progressive hemifacial atrophy.
Management of Progressive Hemifacial Atrophy
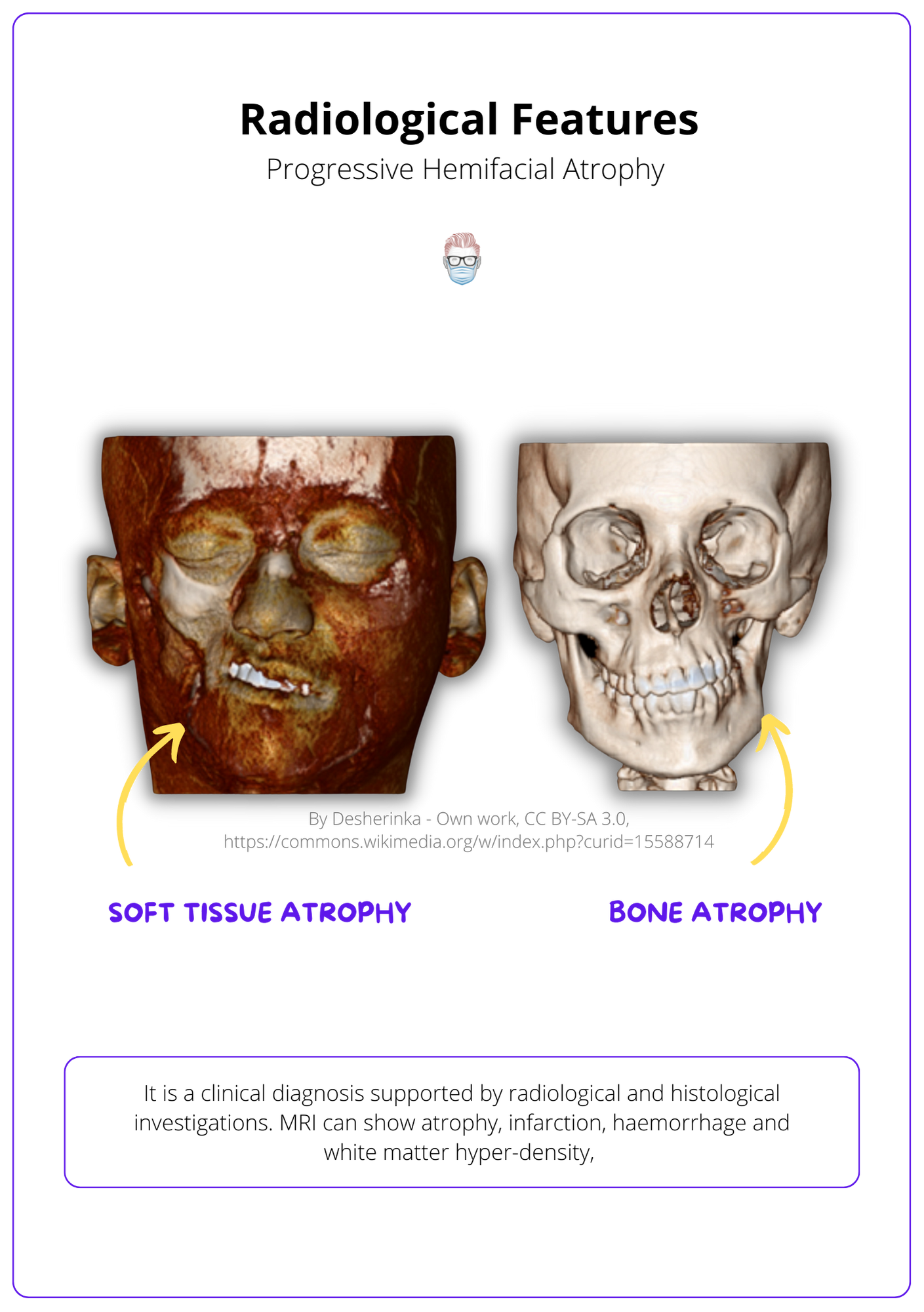
Progressive hemifacial atrophy is a clinical diagnosis supported by MRI and CT scans. Treatment focuses on the reconstruction of atrophied structures and restoration of structures.
The management of progressive hemifacial microsomia is centred on a multi-disciplinary team. Treatment is generally not offered while the condition has not been stable for a period of time.
Investigations
Progressive hemifacial atrophy is a clinical diagnosis supported by radiological and histological investigations.
- MRI: confirm atrophy of soft tissue and bony structures, display infarction, haemorrhage and white matter hyper-density, which can help guide treatment.
- Histology: dermal sclerosis, fat atrophy, decrease in adnexal structures, and perivascular plasma cells and lymphocytes. This is not routine.
- Genetic counselling is not recommended at this time.
The radiological investigations can be visualised below.
Treatment
Treatment is generally not offered while the condition has not been stable for a period of time. These options include:
- Grafts: fat, dermatofat, cartilage
- Flaps: free flaps, muscle transfers, adipofascial flaps
- Bone Reconstruction: Le Fort 1 Osteotomy, Genioplasty
- Implants: Alloplastic augmentation
Conclusion
1. Definition and Epidemiology: You've learned about Progressive Hemifacial Atrophy (PHA), a rare condition characterized by unilateral wasting of facial tissues including skin, soft tissue, and bone, often referred to as Parry-Romberg Syndrome.
2. Clinical Features: You are familiar with the typical clinical manifestations of PHA such as the distinctive "coupe de sabre" appearance, and other symptoms affecting hair, eyes, skin, and facial structures.
3. Diagnostic Approaches: You've explored how PHA is diagnosed primarily through clinical evaluation supported by imaging techniques like MRI and CT scans, which help in assessing the extent of tissue and bone atrophy.
4. Management Strategies: You've gained insight into the treatment options for PHA, focusing on reconstructive techniques to restore facial symmetry and function.
5. Challenges in Management: You understand the complexity of managing PHA due to its progressive nature and the need for treatment to be deferred until the disease stabilizes.


