Summary Card
Overview
Pressure sores are localized injuries to the skin and underlying tissues, primarily over bony areas, caused by prolonged pressure.
Pathophysiology
Pressure sores form through a combination of ischemia and impaired skin integrity, driven by factors like prolonged pressure, shear forces, friction, and moisture.
Risk Factors
The risk of pressure sores is elevated by factors such as infection, age, sensory loss, chronic disease, malnutrition, and incontinence.
Grading
The NPUAP classifies pressure ulcers into 4 stages, with additional categories for unstageable and suspected deep tissue injuries.
Clinical Assessment
Evaluating pressure sores involves taking a comprehensive history, grading the ulcer, and using lab tests and imaging to identify complications such as osteomyelitis.
Prevention
Preventing pressure sores involves regular repositioning, use of pressure-relieving devices, proper transfer techniques, skincare, nutritional support, and patient education.
Management
Stages 1-2 typically require conservative treatment, while stages 3-4 may need debridement, antibiotics, NPWT, and surgical reconstruction.
Reconstruction by Anatomic Site
Flap selection is guided by the ulcer’s location and the requirement for durable, long-lasting coverage.
Primary Contributor: Dr Kurt Lee Chircop, Educational Fellow.
Reviewer: Dr Waruguru Wanjau, Educational Fellow.
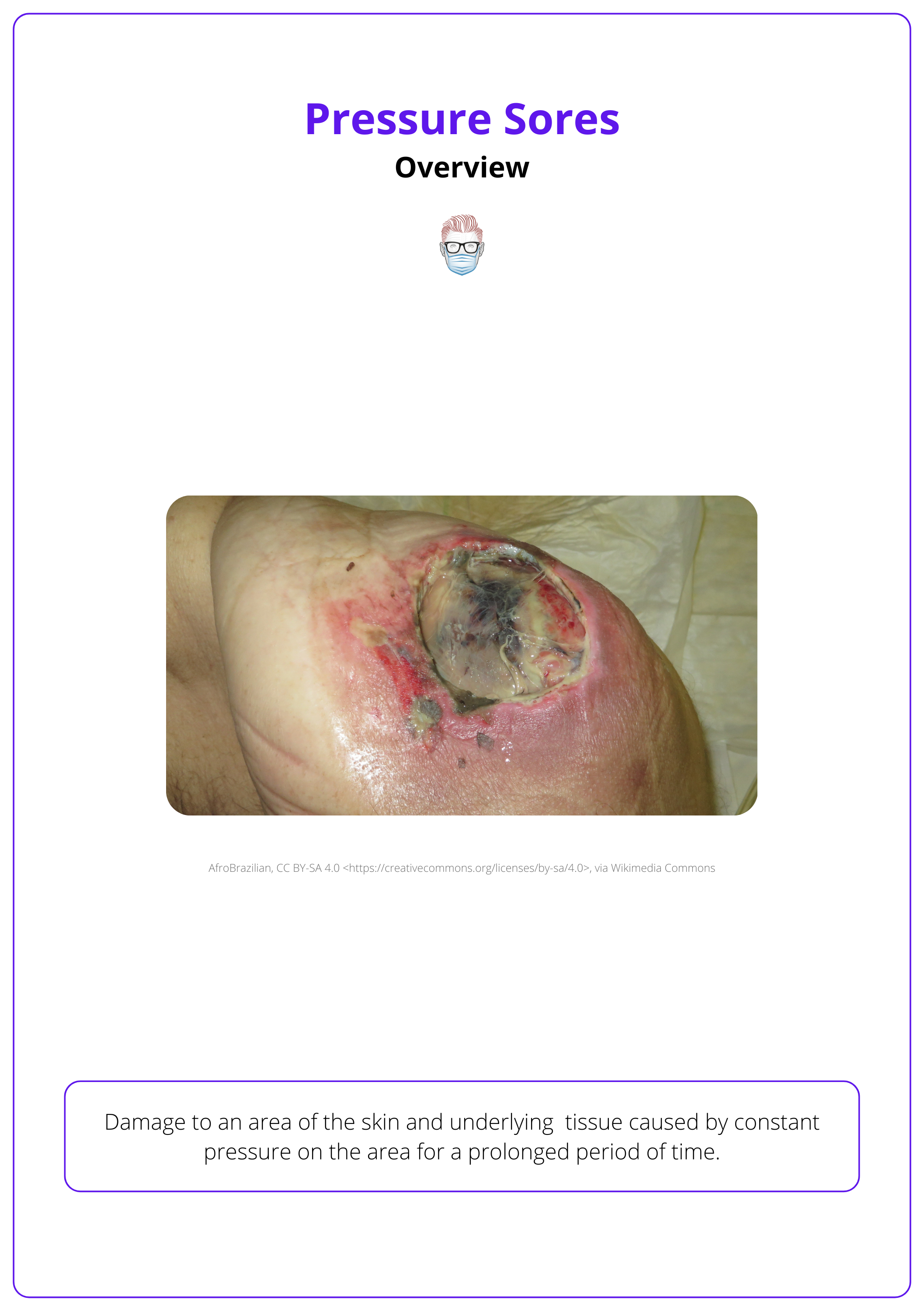
Overview of Pressure Sores
Pressure sores are localized injuries to skin and underlying tissue caused by prolonged pressure, often over bony prominences.
Pressure sores, also known as pressure ulcers or bedsores, occur when prolonged pressure disrupts blood flow, leading to ischemia and tissue damage. Commonly seen over areas like the sacrum, hips, and heels.
Pressure sores disproportionately affect high-risk populations, with rates varying by care setting. For example:
- Elderly Patients: 66% with femoral neck fractures develop sores (Jaul, 2013).
- Quadriplegic Patients: 60% experience pressure ulcers (Bennett, 2000).
- Care Setting: long-term care up to 24% (Bennett, 2000), home care up to 17% (Kottner, 2019).
A common site for pressure ulcers is depicted in the image below.
Pressure sores do not directly increase mortality but worsen morbidity. Malnourished and immobile patients are especially vulnerable, facing delayed recovery and functional decline (Jaul, 2013).
Pathophysiology of Pressure Sores
Pressure sores form through a combination of ischemia and impaired skin integrity, driven by factors like prolonged pressure, shear forces, friction, and moisture.
Pressure sores result from external mechanical forces and physiological responses, where prolonged pressure causes ischemia, and shear, friction, and moisture weaken defenses, leading to oxygen deprivation, oxidative stress, and tissue breakdown.
External Mechanical Forces
More specifically, the mechanical forces involved,
- Prolonged Pressure: Sustained pressure exceeding capillary closing pressure (60–70 mm Hg) compresses blood vessels, leading to ischemia and tissue necrosis within as little as two hours (Gefen, 2007)
- Shear Forces: Displacement of skin layers relative to underlying tissues distorts blood vessels and causes deep tissue injury.
- Friction: Continuous rubbing erodes the skin’s protective layers, increasing vulnerability to breakdown and ulceration.
- Moisture: Excess moisture from perspiration or incontinence softens the skin, promoting maceration and weakening the barrier against injury.
Physiological Responses
The cellular effects of these contributing factors result in progressive tissue breakdown - including,
- Ischemic Necrosis: Prolonged pressure restricts oxygen and nutrient delivery to tissues, leading to cell death and necrosis.
- Reperfusion Injury: sudden return of blood flow to ischemic tissue generates oxidative stress and reactive oxygen species (ROS), which exacerbate cellular damage.
- Tissue Deformation: Shear forces mechanically distort cells, damaging membranes and causing structural trauma that worsens deep tissue injury (Stekelenburg, 2007).
Pressure exceeding capillary closing pressure (approximately 60–70 mm Hg) for two hours can cause irreversible tissue damage (Ray, 2020).
Risk Factors of Pressure Sores
Pressure sore risk increases with factors such as infection, age, sensory loss, chronic disease, malnutrition, incontinence, and reduced mobility.
Pressure sores develop when patient-specific factors, such as impaired mobility and comorbidities, combine with external mechanical forces. Understanding these risk factors allows for targeted prevention and management strategies (Jaul, 2018).
- Infection: Sepsis reduces perfusion, increasing necrosis risk.
- Age: Reduced elasticity and moisture in elderly skin
- Sensory Loss: Paralysis or nerve damage impairs pressure detection.
- Chronic Disease: Diabetes, vascular disease, & anaemia.
- Malnutrition: Weakens skin and delays repair.
- Incontinence: Moisture from urine or faeces softens skin.
- Altered Consciousness: Impaired mobility prevents pressure relief.
Risk Assessment
The Braden Scale standardized global measure that evaluates six key categories to assess a patient’s risk for pressure sores (Chen, 2017). Scores range from 6 (highest risk) to 23 (lowest risk).
Categories Assessed
- Sensory Perception
- Skin Moisture
- Activity
- Mobility
- Friction and Shear
- Nutritional Status
Each category is scored individually, with a total score indicating overall risk. Lower scores indicate higher susceptibility to pressure sores.
Common organisms found in infected pressure sores include Staphylococcus aureus, Proteus mirabilis, Escherichia coli, Pseudomonas aeruginosa, and Enterococcus spp.
Grading of Pressure Sores
The NPUAP classifies pressure ulcers into four stages, with additional categories for unstageable ulcers and suspected deep tissue injuries.
Pressure sores are categorized based on the depth and severity of tissue damage, helping guide management and prognosis. The National Pressure Ulcer Advisory Panel (NPUAP) provides a standardized grading system, which includes four primary stages and two additional classifications for complex cases (Downie, 2016).
- Stage 1: Non-blanchable erythema on intact skin, localized redness.
- Stage 2: Partial-thickness skin loss involving epidermis & dermis, often a shallow ulcer or blister.
- Stage 3: Full-thickness tissue loss extending into the subcutaneous layer, sometimes with tunneling or undermining.
- Stage 4: Full-thickness tissue loss with exposed bone, tendon, or muscle, increasing infection risk and potential osteomyelitis.
The table below summarises these stages and their features.
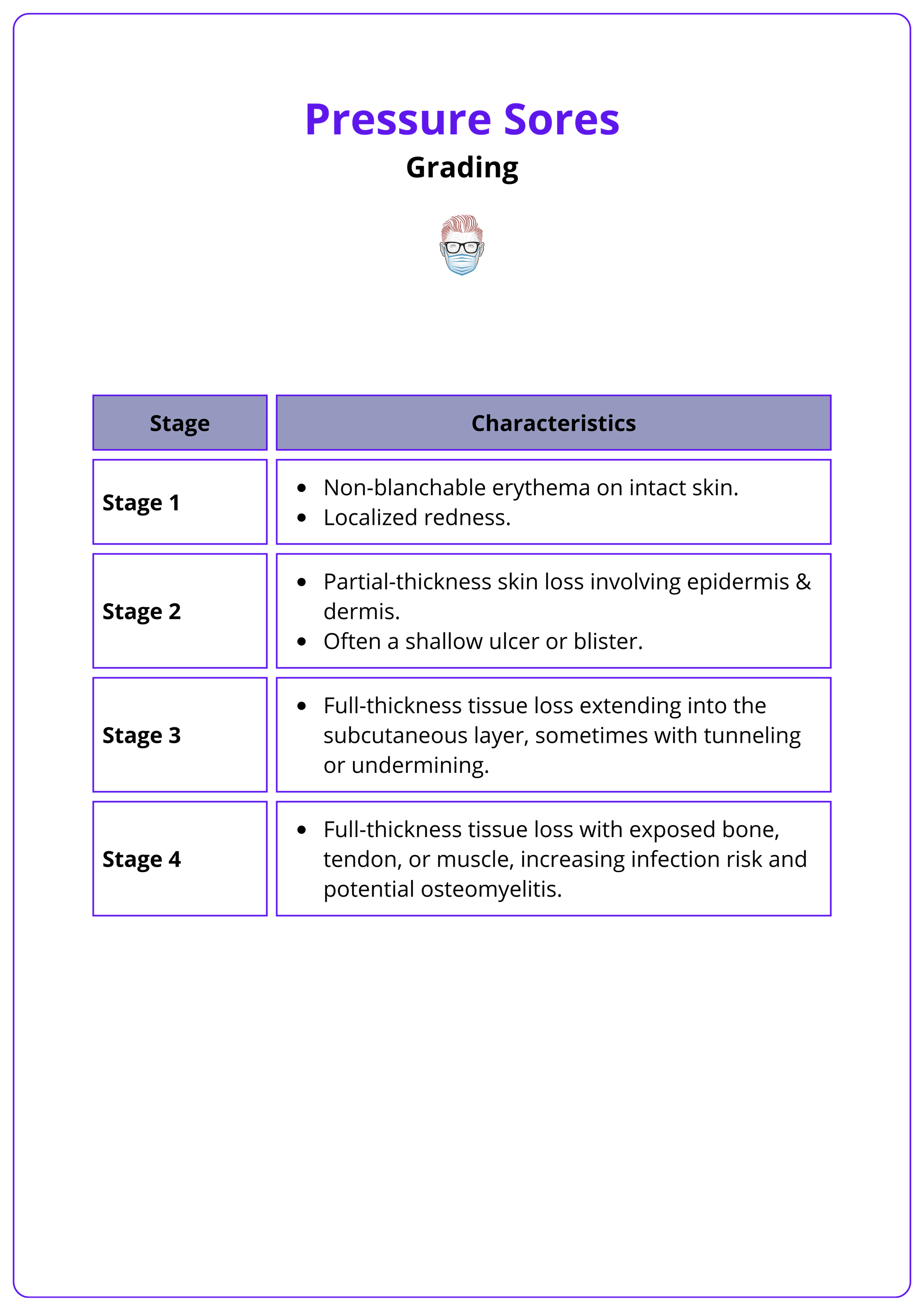
Additional Classifications
- Unstageable Ulcers: Full-thickness tissue loss where the wound depth is obscured by slough or eschar. Typically staged as III or IV after debridement.
- Suspected Deep Tissue Injury: Purple discoloration or blood-filled blister on intact skin. Final staging is determined after the wound evolves.
Stable eschar on the heels should not be debrided, as it acts as a natural biological cover, protecting against infection (Rivolo, 2016).
Clinical Assessment of Pressure Sores
Pressure sore evaluation requires a detailed history, wound staging, and targeted diagnostics to assess severity and complications like infection or osteomyelitis.
A thorough clinical assessment of pressure sores identifies risk factors, evaluates wound severity, and detects complications. This includes gathering a detailed patient history, conducting a focused examination, and utilising laboratory and imaging studies to guide management.
History
Focus on factors that predispose to pressure sores or hinder healing.
- Mobility: Prolonged immobility or frequent transfers.
- Incontinence: Chronic moisture exposure weakening skin barriers.
- Comorbidities: Conditions like diabetes, vascular disease, and poor nutrition.
Physical Examination
- Ulcer Grading: Use the NPUAP classification to stage the pressure sore.
- Wound Details: Identify undermining, tunneling, induration, and signs of infection such as purulence, erythema, or odor.
- Overall Health: Look for systemic signs of delayed healing and evaluate fitness for surgical intervention.
Pressure sores often develop over the sacrum (40%), heel (30%), ischial tuberosity, and trochanter (15–20%), with less common sites including the scalp, elbow, shoulder, and scapula (Gefen, 2013).
Investigations
- Bloods: Complete blood count, albumin, and inflammatory markers.
- Wound cultures to identify pathogens and antibiotic sensitivity.
- MRI or CT: Essential for identifying osteomyelitis, abscesses, or deep tissue involvement.
The image below illustrates the clinical assessment of a left buttock ulcer extending to the ischial tuberosity.

Prevention of Pressure Sores
Preventing pressure sores requires regular repositioning, pressure-relieving devices, proper skincare, nutritional support, and patient education.
Prevention is critical for reducing the incidence and complications of pressure sores, particularly in high-risk individuals. Strategies focus on minimizing pressure, protecting the skin, and optimizing patient care through education and support (Kottner, 2019).
Minimizing Pressure
- Regular repositioning: Every 10 minutes if seated; every 2 hours if supine.
- Bed Elevation: Below 45 degrees to reduce shear on the sacrum.
Protective Measures
- Devices: Pressure-relieving devices, such as specialized mattresses and heel protectors, to evenly distribute pressure.
- Skin: Maintain skin cleanliness and apply moisture barrier creams to prevent breakdown.
Supportive Care
- Nutrition: Adequate caloric and protein intake for skin integrity.
- Spasticity: Address involuntary movements to prevent trauma.
Education
- Patients: Proper repositioning, device usage, and regular skin inspections.
- Caregivers: Proper transfer techniques to minimize shear and friction.
Management of Pressure Sores
Pressure sore management involves offloading, infection control, and wound care. Stages 1–2 is often conservative, while stages 3–4 may require debridement, antibiotics, NPWT, or surgical reconstruction.
Effective management of pressure sores depends on their severity. Initial treatment focuses on pressure offloading and wound care, with advanced therapies reserved for deeper or infected ulcers. Optimizing patient factors like nutrition and addressing comorbidities is critical for successful outcomes (Qaseem, 2015).
Stages 1 and 2
Management of early-stage pressure sores emphasizes conservative care to restore skin integrity and prevent progression.
- Pressure Offloading: Relieve pressure from the affected area to reduce ischemia.
- Daily Wound Care: Clean and dress wounds to maintain a suitable healing environment.
- Patient Optimization: Address nutritional deficits and conditions like anemia.
- Incontinence Control: Manage moisture exposure, potentially with a defunctioning stoma.
Stages 3 and 4
Advanced-stage pressure sores require more aggressive interventions to remove necrotic tissue, control infection, and facilitate wound closure.
- Debridement: Remove necrotic tissue using surgical, enzymatic, or autolytic methods.
- Infection Control: Use systemic antibiotics for signs of cellulitis or osteomyelitis.
- NPWT: Apply negative pressure wound therapy to stimulate granulation tissue formation.
- Surgical Reconstruction: Perform flap reconstruction for non-healing ulcers.
An example of a stage 4 ulcer requiring debridement is shown in the image below.

Avoid potent antiseptics like betadine during dressing changes, as they can irritate the wound.
Reconstruction by Anatomic Site
Flap selection for pressure sore reconstruction is determined by the ulcer's location and the need for durable coverage that withstands mechanical forces and promotes healing.
Reconstructive options vary based on the anatomical site of pressure sores. Each region presents unique challenges due to its vascularity, exposure to pressure, and functional requirements. Flap selection aims to achieve durable coverage while minimizing the risk of recurrence.
Pressure sore reconstructive options are detailed in the table below.
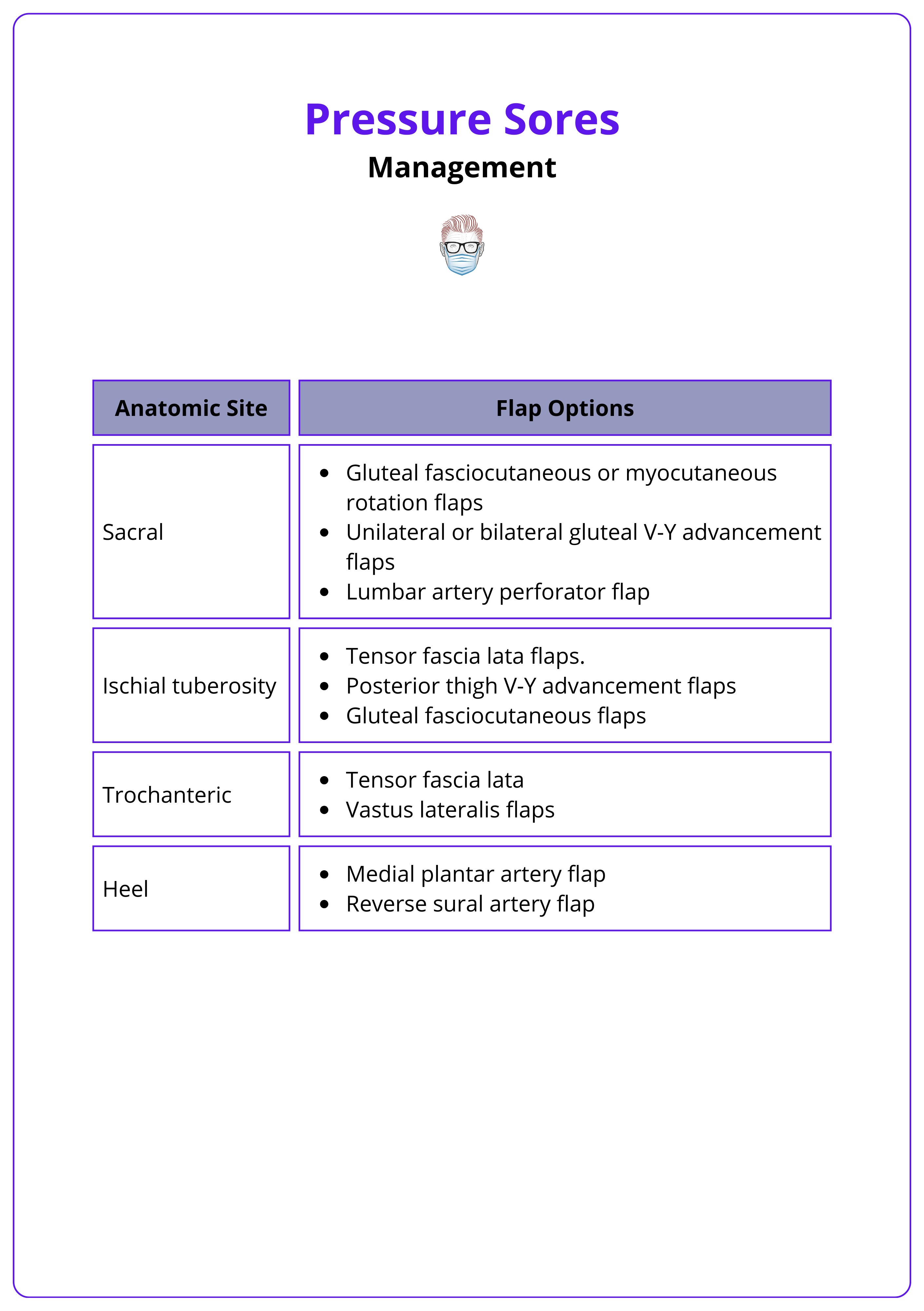
Sacral Region
The sacrum is a common site for large pressure ulcers, often requiring robust flaps for coverage. Typical options include,
- Gluteal fasciocutaneous or myocutaneous rotation flaps for broad defects.
- Unilateral or bilateral gluteal V-Y advancement flaps for midline closures.
- Lumbar artery perforator flaps, particularly for extended defects needing reach and mobility.
Ischial Tuberosity
This region is highly prone to recurrence due to sitting pressure. Flaps commonly used include,
- Tensor fascia lata flaps for large defect coverage.
- Posterior thigh V-Y advancement flaps for stable and durable outcomes.
- Gluteal fasciocutaneous flaps for extensive or recurrent sores.
Trochanteric Region
Trochanteric ulcers often require flaps that can tolerate friction and enhance mobility. Recommended flaps:
- Tensor fascia lata flap for moderate-sized ulcers.
- Vastus lateralis flap for extended defects needing robust coverage.
Heel
The heel is exposed to high mechanical stress, requiring flaps resistant to shear forces. Effective options:
- Medial plantar artery flap for precise plantar coverage.
- Reverse sural artery flap for large or posterior heel defects.
Postoperative Management
Comprehensive postoperative care is critical to successful healing. This involves,
- Bed Rest: Use specialized beds for pressure relief with frequent repositioning.
- Infection Control: Administer antibiotics based on wound culture results.
- Spasticity and Bowel Care: Manage spasticity and incontinence to protect surgical outcomes.
- Nutritional Support: Ensure high-protein, high-calorie diets to promote healing.
- Rehabilitation: Implement range-of-motion exercises, seat mapping, and sitting protocols to prevent recurrence
Single-stage reconstruction is ideal, but in staged reconstruction, prioritize closure of larger defects to ensure effective wound coverage and healing.
Conclusion
1. Definition of Pressure Sores: Pressure sores, or bedsores, are localized skin and tissue injuries from prolonged pressure, especially over bony prominences like the sacrum, hips, and heels, leading to ischemia and tissue damage.
2. Risk Factors of Pressure Sores: Major risk factors include immobility, age, sensory loss, malnutrition, incontinence, and chronic diseases like diabetes. The Braden Scale helps assess individual risk levels.
3. Pathophysiology and Mechanism: Pressure sores develop from sustained pressure, shear forces, friction, and moisture, which disrupt blood flow and lead to tissue ischemia, reperfusion injury, and cellular damage.
4. Grading of Pressure Sores: The NPUAP categorizes pressure sores into stages from 1 to 4, based on tissue involvement, with additional categories for unstageable and suspected deep tissue injuries.
5. Prevention of Pressure Sores: Key prevention strategies include regular repositioning, pressure-relieving devices, proper skincare, nutritional support, and educating patients and caregivers on preventive measures.
6. Management of Pressure Sores: Treatment depends on the sore's stage, with conservative care like offloading and dressings for early stages, and debridement, antibiotics, and possible surgical reconstruction for advanced stages.
Further Reading
- Jaul E. (2013). Who determines the treatment for pressure ulcers in the elderly? The Israel Medical Association journal: IMAJ, 15(9), 512–515.
- Qaseem A, Humphrey LL, Forciea MA, Starkey M, Denberg TD; Clinical Guidelines Committee of the American College of Physicians. Treatment of pressure ulcers: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2015 Mar 3;162(5):370-9. doi: 10.7326/M14-1568. PMID: 25732279.
- Braden, Barbara, and Nancy Bergstrom. "A conceptual schema for the study of the etiology of pressure sores." Rehabilitation Nursing Journal 25.3 (2000): 105-110.
- Kottner, Jan, et al. "Prevention and treatment of pressure ulcers/injuries: The protocol for the second update of the international Clinical Practice Guideline 2019." Journal of tissue viability 28.2 (2019): 51-58.
- Gefen A. (2007). The biomechanics of sitting-acquired pressure ulcers in patients with spinal cord injury or lesions. International wound journal, 4(3), 222–231. https://doi.org/10.1111/j.1742-481X.2007.00330.x
- Ray, Carle. Case Analysis of Acute Care Guidelines for the Prevention of Pressure Ulcers. Diss. Walden University, 2020.
- Stekelenburg, Anke, et al. "Role of ischemia and deformation in the onset of compression-induced deep tissue injury: MRI-based studies in a rat model." Journal of Applied Physiology 102.5 (2007): 2002-2011.
- Gefen, A., Farid, K. J., & Shaywitz, I. (2013). A review of deep tissue injury development, detection, and prevention: shear savvy. Ostomy/wound management, 59(2), 26–35.
- Jaul, Efraim, et al. "An overview of co-morbidities and the development of pressure ulcers among older adults." BMC geriatrics 18 (2018): 1-11.
- Chen HL, Cao YJ, Zhang W, Wang J, Huai BS. Braden scale (ALB) for assessing pressure ulcer risk in hospital patients: A validity and reliability study. Appl Nurs Res. 2017 Feb;33:169-174. doi: 10.1016/j.apnr.2016.12.001. Epub 2016 Dec 5. PMID: 28096013.
- Downie, Fiona, and Heidi Guy. "LATEST DEVELOPMENTS IN THE GRADING OF PRESSURE ULCERS." Wounds UK 8.3 (2012).


