Summary Card
Penile Anatomy
The penis contains unique erectile tissues — corpora cavernosa and corpus spongiosum (enveloping the urethra) — with specialized structures essential for reconstructive procedures.
Causes of Penile Tissue Loss/Dysfunction
Penile tissue loss may result from benign or malignant conditions, infections, circumcision complications, burns, trauma, and fibrosis (such as Peyronie’s disease).
Penile Reconstruction
The primary aim of penile reconstruction is to construct a phallus with a neo-urethra that enables standing urination and sufficient bulk to support a prosthesis for penetrative intercourse.
Penis Replant
Penis reimplantation is indicated for sharp, non-avulsive injuries with controlled contamination and ischemia time.
Penile Prosthesis Implantation
In patients with impotence and penile fibrosis, a penile prosthesis may be the only viable solution for restoring erectile function..
Primary Contributor: Dr Waruguru Wanjau, Educational Fellow.
Reviewer: Dr Suzanne Thomson, Educational Fellow.
Penile Anatomy
The penis contains unique erectile tissues — corpora cavernosa and corpus spongiosum (enveloping the urethra) — with specialized structures that must be reconstructed.
The penis is structured cylindrically, with two corpora cavernosa situated adjacent to each other and the corpus spongiosum located inferiorly, each enabling erectile function (Kropp, 2019).
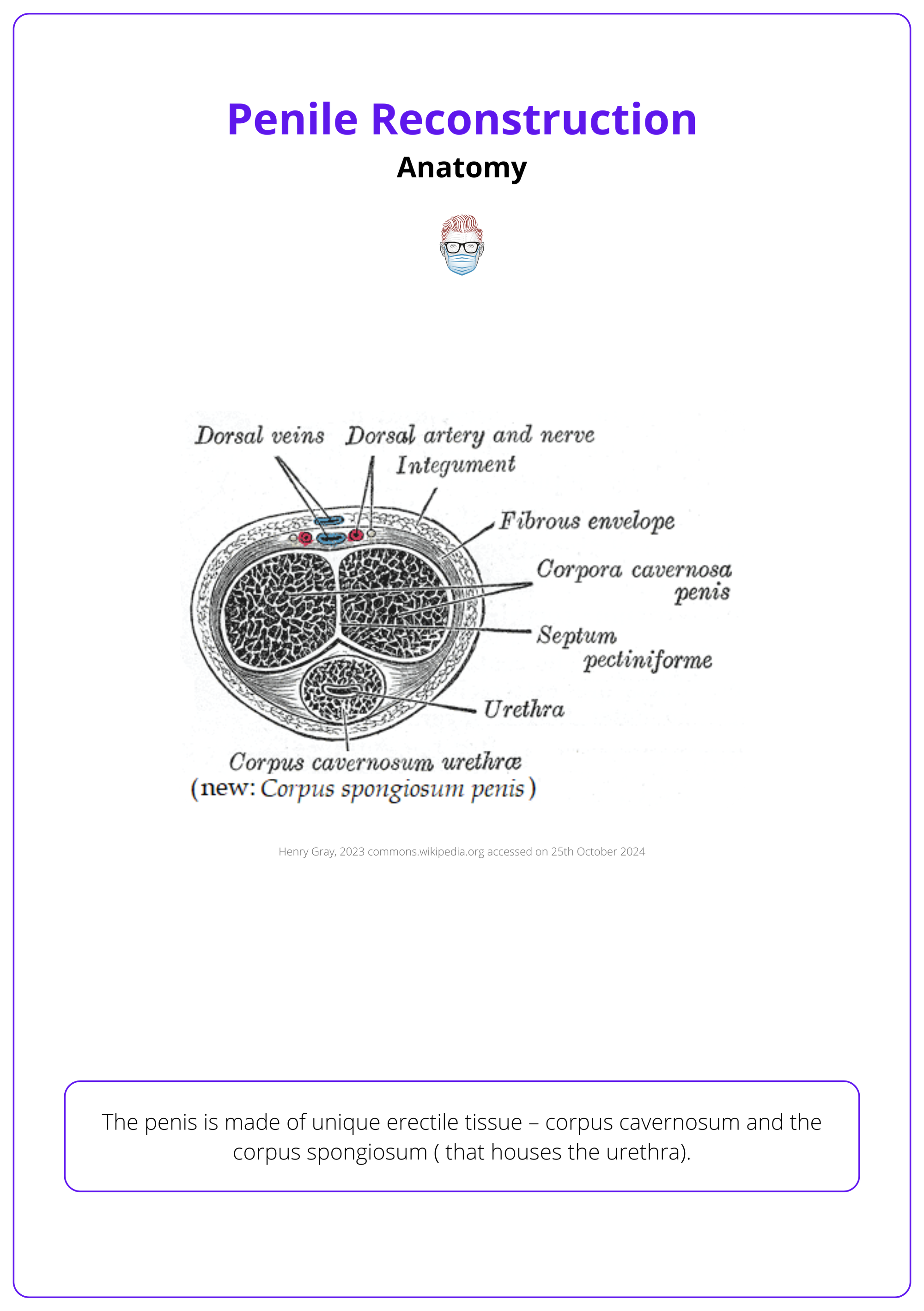
Anatomical Structures
- Urethra: resides within the corpus spongiosum.
- Dartos Fascia: Encloses the penis beneath the skin.
- Buck’s Fascia: Encloses the corpora cavernosa and corpus spongiosum.
Blood Supply
- Common Penile Artery: arises from the internal pudendal artery (branch of internal iliac artery and branches into:
- Deep Cavernosal Arteries: In the corpora cavernosa & branches into helicine arteries to support erectile tissue.
- Bulbourethral Artery
- Dorsal Artery (supplies the glans)
- Venous Outflow: Venous drainage occurs through emissary veins within the tunica albuginea.
Innervation
- Sensory and Motor: Supplied by the pudendal nerve.
- Erectile Function: Innervated by cavernous nerves, enabling erectile response.
The penis has separate blood supplies for the glans and shaft. The shaft skin is nourished by a dermal plexus, while the dorsal artery supplies the glans (Brown, 2023).
Causes of Penile Tissue Loss/Dysfunction
Penile tissue loss can result from various benign and malignant conditions, infections, circumcision complications, burns, trauma, and fibrosis, including Peyronie’s disease.
Penile tissue loss or dysfunction arises from a variety of causes, affecting the glans, shaft, and scrotum in unique ways. Each area has specific vulnerabilities and typical conditions that may lead to tissue damage, impacting function and requiring targeted management.
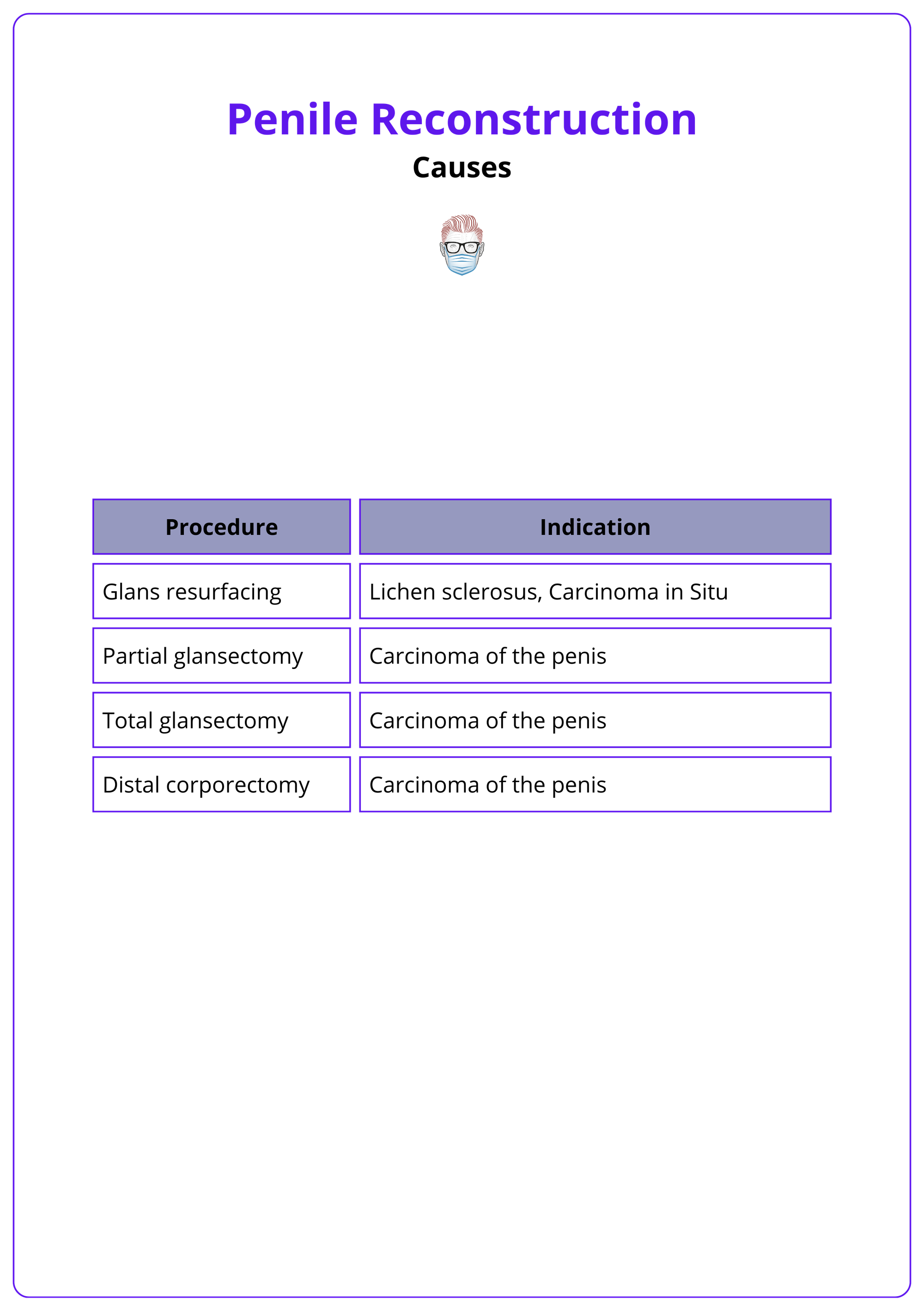
Glans
Common causes of tissue loss in the glans include chronic inflammatory conditions, early-stage cancer, and surgical intervention.
- Lichen Sclerosus: Chronic inflammation leading to scarring and tissue loss.
- Carcinoma In Situ (CIS): Early-stage cancer that may require excision.
- Surgical Procedures: Partial or complete removal of the glans may be necessary in severe cases (Garaffa, 2013).
Surgical procedures involving partial or complete excision of the glans are illustrated in the table below (Garaffa, 2013).
Penile Shaft
Tissue loss or dysfunction in the shaft can result from trauma, infections, surgical complications, and fibrosis.
- Trauma and Burns: Injury from accidents, burns, or animal bites can lead to significant tissue damage.
- Necrotizing Fasciitis: A rapidly progressing infection causing extensive tissue destruction.
- Surgical Excision and Excessive Circumcision: Tissue loss from removal of lesions or over-removal during circumcision.
- Complications from Hypospadias/Epispadias Surgery: Scarring and dysfunction following corrective procedures.
- Peyronie’s Disease: Fibrosis resulting in scar tissue formation, which affects structure and function.
Scrotum
Scrotal tissue loss commonly arises from severe infections, trauma, or surgical procedures.
- Necrotizing Fasciitis: extensive tissue damage specific to the scrotal area.
- Trauma and Surgical Excision: Tissue loss due to direct injury or the removal of bulky tumors affecting the scrotal or penile region.
Glans
Common causes of glans tissue loss include,
- Lichen Sclerosus
- Carcinoma In Situ (CIS) of the glans penis
Necrotizing fasciitis (NF) is traditionally classified by anatomical region. Fournier’s gangrene, a form of NF, affects the scrotum, penis, or perineum (The Plastics Fella, 2024).
Penile Reconstruction
The primary aim of penile reconstruction is to construct a phallus with a neo-urethra that enables standing urination and sufficient bulk to support a prosthesis for penetrative intercourse.
Overview of Penile Reconstruction
The ultimate goal is a phallus that meets cosmetic and functional standards, with an integrated neo-urethra for voiding and sufficient structure to house prosthetic cylinders for adequate rigidity (Garaffa, 2013).
- Functional Length and Skin Adequacy: Ensure sufficient penile length and skin coverage to allow unrestricted erections.
- Protective Sensation: Achieve protective sensation to prevent chronic skin breakdown.
- Standing Voiding Capability: Enable spontaneous voiding while standing, with urine flow from the phallic tip.
- Erectile Function
Tailor reconstruction to patient expectations, habitus, and history. Thick adipose may limit thigh/forearm flaps; abdominal scars may exclude infraumbilical flaps (Garaffa, 2013).
Glans Reconstruction
For patients undergoing glansectomy, reconstructive techniques—such as skin grafts, and urethral & tissue flaps —can help restore both form and function. (Smith, 2007 & Garaffa, 2013).
- Split-Thickness Skin Graft (STSG): Applied to the denuded corpora to restore coverage post-glansectomy. Risks include graft loss and overgrowth at the external urethral meatus, which may require urethral dilation.
- Urethral Flap: The urethra is reshaped and inverted to form a “pseudo-glans,” restoring glans structure. A minor ventral curvature may occur due to bowstringing if the urethra is shortened during the process.
- Alternative Flaps: Additional options include flaps from urethral mucosa, rectus abdominis muscle, or palmaris longus tendon, chosen based on the extent of tissue needed. (Smith, 2007 & Garaffa, 2013).
Most patients retain sexual and urinary function, with the majority able to resume penetrative intercourse approximately three months post-surgery.
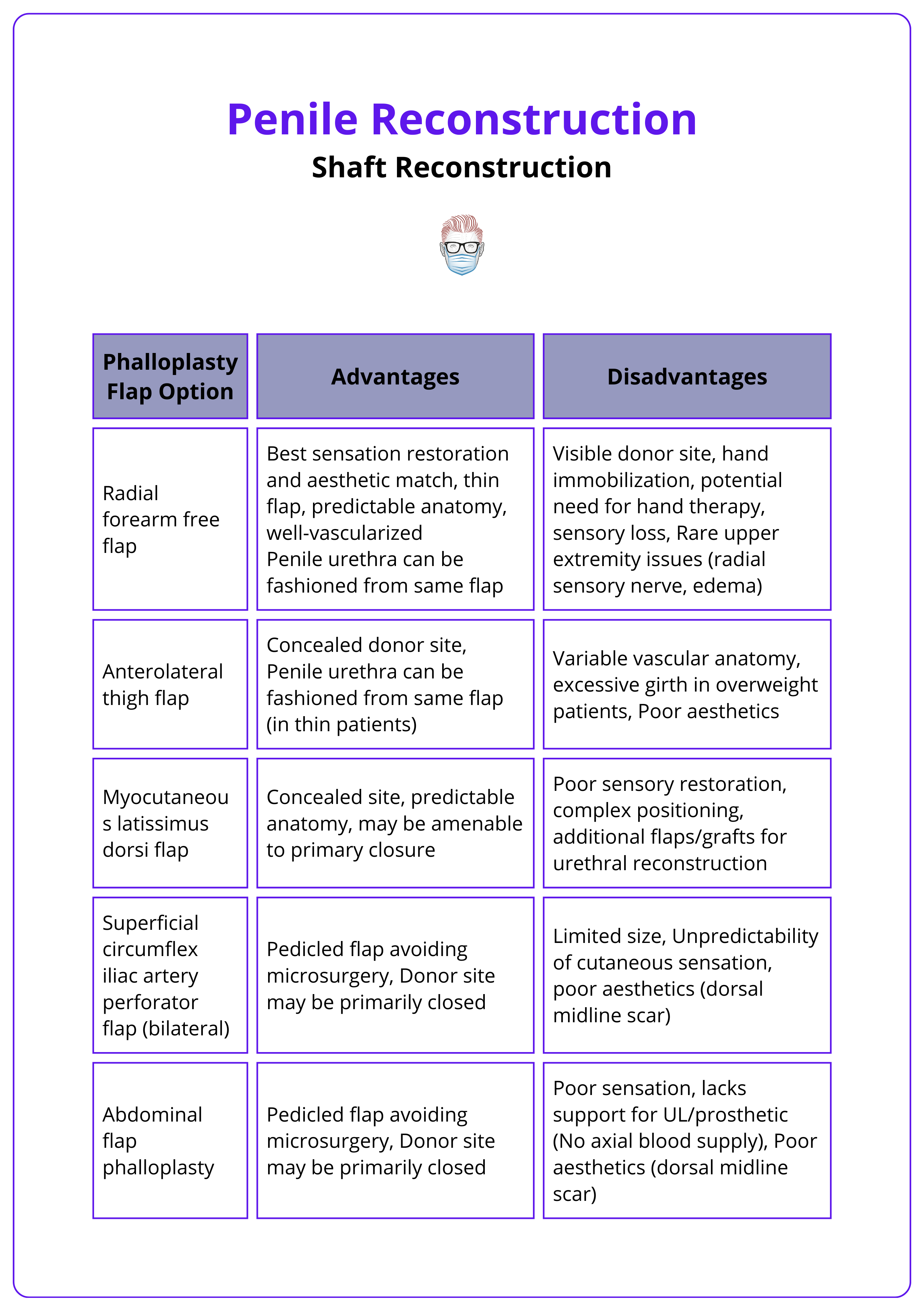
Shaft Reconstruction
Shaft reconstruction prioritizes preserving any existing penile stump to maintain function and appearance. When full phalloplasty is required, flaps like the radial forearm free flap (RFFF) and anterolateral thigh (ALT) flap are used to restore form and function.
Types of Shaft Reconstruction
Shaft reconstruction techniques are tailored to the extent of tissue loss, ranging from skin grafts to structural modifications that enhance length and appearance.
- Skin-Only Reconstruction: STSG commonly used but may contract over time. FTSG from non-hair-bearing areas are preferred, as they provide better cosmetic outcomes.
- Corpus Reconstruction: For partial amputations with sufficient length, conservative management may include suspensory ligament division and suprapubic fat pad excision, both of which optimize visible length and enhance the appearance of the penile stump (Garaffa, 2013).
Scrotal Reconstruction
Reconstruction techniques for the scrotum vary based on defect size, location, and desired functional outcomes (Khan, 2013). Options range from direct closure for small defects to grafts, flaps, and tissue expansion.
- Direct Closure: For scrotal defects under 50%, direct closure is often achievable with acceptable cosmetic outcomes. (Selvan, 2009)
- Split-Skin Graft: Used to create a smooth graft bed and shallow intertesticular groove, though contraction at the penoscrotal junction can affect erectile function.
- Tissue Expansion: A two-stage process with Stage 1 placing expanders under the dartos fascia, Stage 2 testicular mobilization, orchidopexy, and defect closure are achieved with a V–Y advancement.
- Advancement Flaps: Based on scrotal vascular supply; three zones of perfusion (two lateral, one central) with lateral supply from the inferior external pudendal artery and central supply from perineal artery branches.
- Fasciocutaneous Flaps: Options include posterior neurovascular pedicled pudendal thigh flaps, modified medial thigh flaps, and medial circumflex femoral artery perforator flaps.
- Myofasciocutaneous Flaps: Incorporate muscles like adductor magnus, longus, semitendinosus, and semimembranosus in flap design.
- Omental Pedicle Flaps: Suitable for large defects when other options are insufficient.
Testicular Relocation was previously performed to the medial thigh, but is now rare due to risks of pain, atrophy, and functional compromise.
Full Penile Reconstruction (Phalloplasty)
Full penile reconstruction aims to restore both urinary and sexual function. Key principles for an ideal reconstruction include establishing urethral continuity and sensory restoration.
Various flaps are available for penile reconstruction, each with specific benefits based on tissue requirements and patient needs. Ideal reconstruction principles are listed below (Chung, 2024).
- Tube-within-a-Tube Construct: This technique is used to create a continuous urethral passage, enabling urination.
- Sensory Neurotization: Restores sensation to improve sexual function and tactile feedback.
Urethral complications are frequent, including,
- Strictures and Fistulas: Narrowing or abnormal connections in the urethra can impair function.
- Rigidity Challenges: Difficulties in achieving adequate rigidity for intercourse are common in phalloplasty procedures.
Flaps can be considered for penile reconstruction, see table below.
Full-thickness grafts from non-hair-bearing areas are ideal for patients with good erectile function who prioritize cosmetic appearance and intend to resume penetrative sex (Garaffa, 2013).
Penis Replant
Penis replant is recommended for sharp, non-avulsive injuries with controlled contamination and limited ischemia time.
Penis replantation involves a complex surgical procedure aimed at restoring function and appearance following traumatic amputation. Success depends on careful selection based on injury type, contamination level, and ischemia duration.
Key decision-making requirements include,
- Indications: suitable for sharp, non-avulsive injuries.
- Contraindications: Gross Contamination (high risk of infection), extended Warm Ischemia Time >8 hours.
- Psychiatric Conditions: relative contraindications due to risk of recurrence (Brown, 2023).
Surgical Approach to Penis Replant
A structured, stepwise approach ensures effective replantation by restoring critical structures and functionality (Brown, 2023).
- Debridement and Dissection: Remove nonviable tissue and identify dorsal arteries, veins, and nerves for reattachment.
- Urethral and Corporal Repair: Spatulate and repair the urethra over a Foley catheter, followed by direct repair of tunica albuginea and corpora cavernosa to preserve function.
- Vascular Anastomoses: End-to-end anastomosis of dorsal arteries and veins restores blood flow.
- Closure and Dressing: Close Buck’s fascia and skin loosely to prevent tension, and apply protective dressings.
- Postoperative Care: Foley Catheter retain for 2–3 weeks postoperatively to minimize the risk of urethral stricture.
Order of Repair
The recommended sequence for replantation is urethra → deep arteries → tunica albuginea → corpus cavernosum → dorsal veins → dorsal arteries → dorsal nerves → fascia → skin (Biswas, 2013).
Postoperative edema is common and can increase skin tension; creating multiple skin incisions can help reduce edema. (Chou, 2008)
Penile Prosthesis Implantation
For patients with both erectile dysfunction and extensive penile fibrosis, a penile prosthesis is often the only effective solution for restoring erectile function.
Penile prosthesis implantation is indicated for patients with significant fibrosis where conventional therapies are ineffective. This approach addresses fibrosis causes, requires corporeal reconstruction when tunical defects are present, and entails managing specific implant-related complications.
Indications
Penile prosthesis implantation is recommended for patients with erectile dysfunction stemming from fibrosis where other therapies are ineffective. This can be caused by:
- Acute Conditions: Priapism, Trauma
- Chronic Conditions: Peyronie’s disease, Chronic intracavernous injections
- Iatrogenic: Implant removal, infection, erosion or malfunction
Corporeal Reconstruction
For cases with significant tunical defects during implantation, grafting is often necessary to reconstruct the tunica and support the prosthesis. Autologous Graft Options include,
- Fascia Options: Rectus (Tran, 2008), Fascia Lata, Temporalis Fascia.
- Dermis
- Saphenous Vein
- Tunica Albuginea
Implant-Related Complications
Common complications include,
- Infection of the device
- Erosion of the prosthesis
- Mechanical Failure of the device (Garaffa, 2013)
Preserve native penile tissue whenever possible, reserving total phallic reconstruction as a last option (Garaffa, 2013)
Conclusion
1. Penile Anatomy: The penis consists of two corpora cavernosa and a corpus spongiosum, which houses the urethra. It has distinct fascial layers, blood supply, and innervation for erectile function and reconstruction.
2. Causes of Penile Tissue Loss/Dysfunction: Tissue loss or dysfunction in the penis may result from trauma, infections, cancer, circumcision complications, or fibrosis.
3. Approach and Goals of Penile Reconstruction: Penile reconstruction aims to create a functional phallus with sufficient bulk, a neo-urethra for standing urination, and the potential for a prosthesis.
4. Glans Reconstruction: Following glansectomy, reconstruction techniques include split-thickness skin grafts and urethral flaps. While most patients retain function, graft loss and minor curvature may occur.
5. Shaft Reconstruction: Shaft reconstruction involves skin grafts for minor defects and complete phalloplasty using free flaps for full reconstruction, aiming to preserve existing penile tissue whenever possible.
6. Penis Reimplantation: Suitable for clean, sharp injuries with limited ischemia time. Reimplantation involves vascular anastomoses, urethral repair, and staged postoperative care to minimize complications.
7. Penile Prosthesis Implantation: For patients with fibrosis and impotence, prostheses restore function, though complications include infection, erosion, and mechanical failure.
8. Scrotal Reconstruction: Depending on defect size, reconstruction may involve direct closure, skin grafts, flaps, or tissue expansion to optimize aesthetics and function.
9. Peyronie’s Disease: This fibrotic disorder of the tunica albuginea causes penile curvature and pain, managed with plication, grafting, or prostheses in severe cases.
Further Reading
- Garaffa G, Sansalone S, Ralph DJ. Penile reconstruction. Asian J Androl. 2013 Jan;15(1):16-9. doi: 10.1038/aja.2012.9. Epub 2012 Mar 19. PMID: 22426595; PMCID: PMC3739136.
- Brown D. Michigan Manual of Plastic Surgery 3rd edition 2023 Oct page 545-548
- Cavayero CT, Leslie SW, McIntosh GV. Penile Prosthesis Implantation. [Updated 2024 Apr 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
- Smith Y, Hadway P, Biedrzycki O, Perry MJ, Corbishley C, Watkin NA. Reconstructive surgery for invasive squamous carcinoma of the glans penis. Eur Urol. 2007 Oct;52(4):1179-85. doi: 10.1016/j.eururo.2007.02.038. Epub 2007 Feb 20. PMID: 17349734.
- Kropp B, Cohn JE, Wang W, Sokoya M, Ducic Y. Free Tissue Transfer Penile Reconstruction. Semin Plast Surg. 2019 Feb;33(1):24-29. doi: 10.1055/s-0039-1677879. Epub 2019 Mar 8. PMID: 30863209; PMCID: PMC6408249.
- Yao A, Ingargiola MJ, Lopez CD, Sanati-Mehrizy P, Burish NM, Jablonka EM, Taub PJ. Total penile reconstruction: A systematic review. J Plast Reconstr Aesthet Surg. 2018 Jun;71(6):788-806. doi: 10.1016/j.bjps.2018.02.002. Epub 2018 Feb 14. PMID: 29622476.
- Tran VQ, Lesser TF, Kim DH, Aboseif SR. Penile corporeal reconstruction during difficult placement of a penile prosthesis. Adv Urol. 2008;2008:370947. doi: 10.1155/2008/370947. Epub 2008 Nov 4. PMID: 19009028; PMCID: PMC2581727.
- Biswas G. Technical considerations and outcomes in penile replantation. Semin Plast Surg. 2013 Nov;27(4):205-10. doi: 10.1055/s-0033-1360588. PMID: 24872770; PMCID: PMC3842340.
- Chou EK, Tai YT, Wu CI, Lin MS, Chen HH, Chang SC. Penile replantation, complication management, and technique refinement. Microsurgery. 2008;28(3):153-6. doi: 10.1002/micr.20470. PMID: 18286649.
- Chung 2024. Grabb and Smith's Plastic Surgery: 9th Edition September 2024 page 1169, 1211-1217
- Mulhall JP, Schiff J, Guhring P. An analysis of the natural history of Peyronie's disease. J Urol. 2006 Jun;175(6):2115-8; discussion 2118. doi: 10.1016/S0022-5347(06)00270-9. PMID: 16697815.
- Selvan SS, Alagu GS, Gunasekaran R. Use of a hypogastric flap and split-thickness skin grafting for a degloving injury of the penis and scrotum: A different approach. Indian J Plast Surg. 2009 Jul;42(2):258-60. doi: 10.4103/0970-0358.59296. PMID: 20368872; PMCID: PMC2845379.
- Khan, Q., Knight, R.J.W. & Goodwin-Walters, A. Scrotal reconstruction: a review and a proposed algorithm. Eur J Plast Surg 36, 399–406 (2013).


