Summary Card
Overview
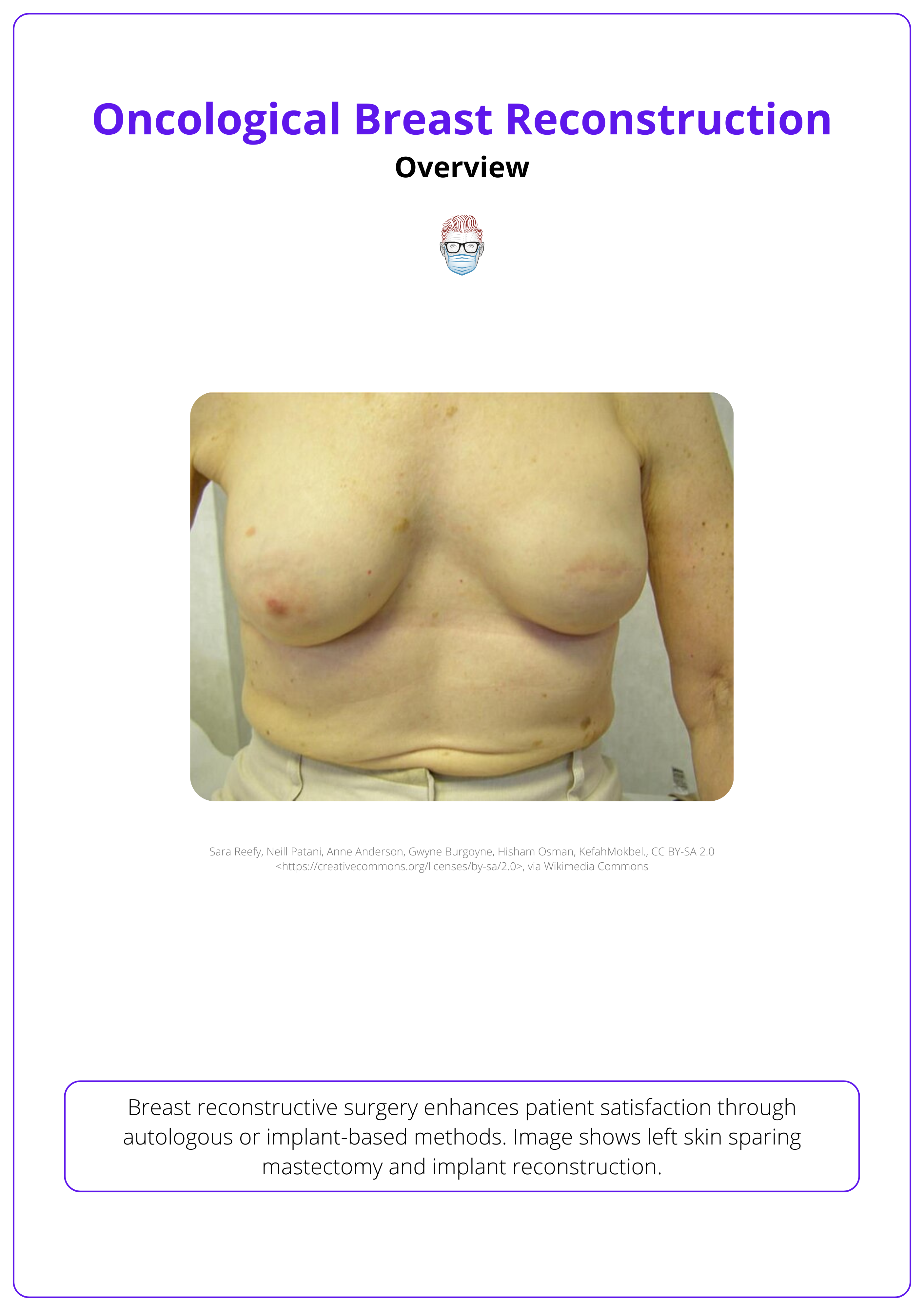
Breast reconstructive surgery enhances patient satisfaction through autologous or implant-based methods.
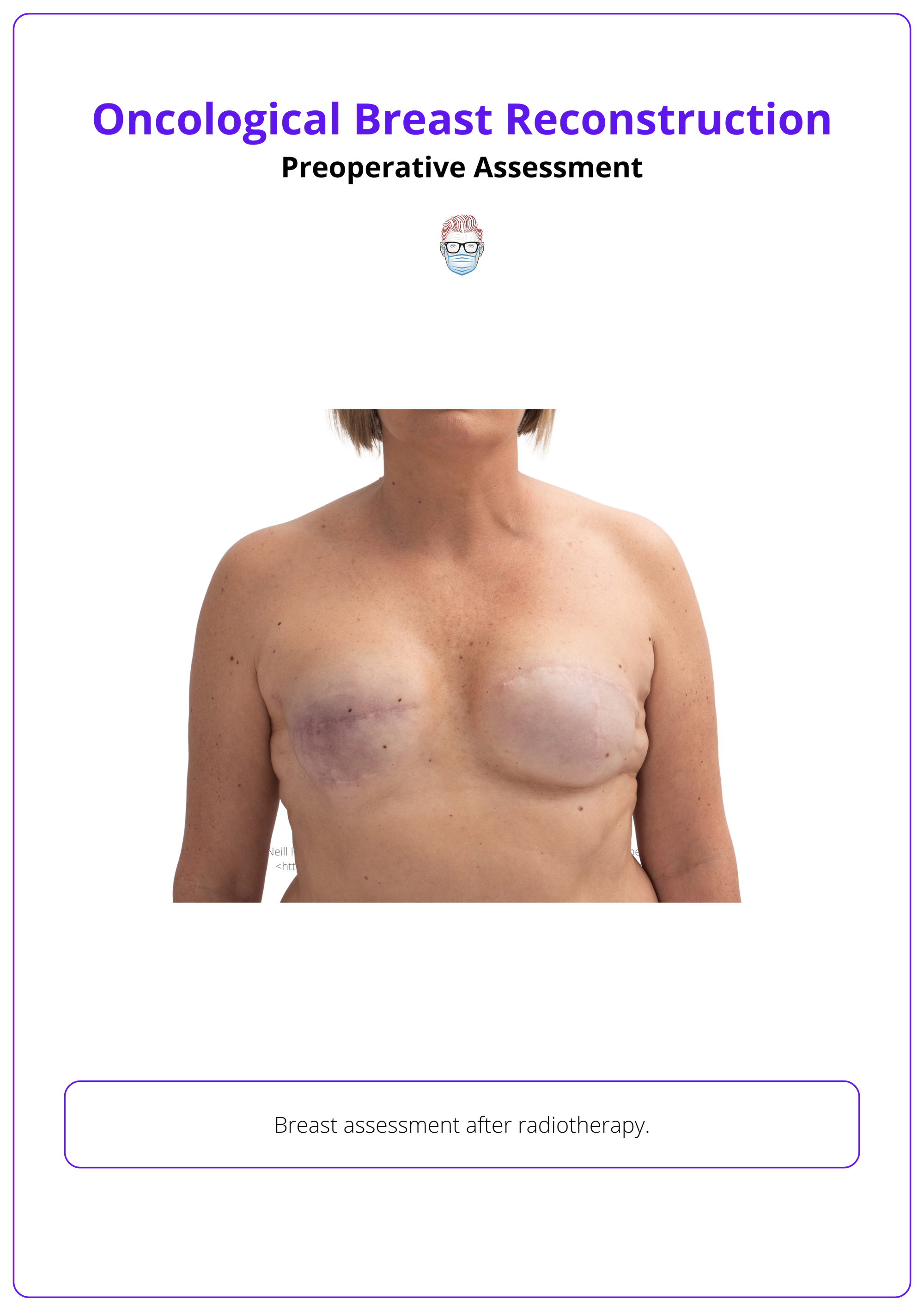
Preoperative Assessment
A thorough clinical assessment is required to evaluate patient needs and individualize reconstructive plans.
Timing
Breast reconstruction timing and method depend on patient factors and radiation plans, balancing aesthetics, complexity, and recovery.
Decision-Making Process
Creating a tailored breast reconstruction plan involves balancing oncologic needs, radiation therapy, patient anatomy, and willingness for staged procedures.
Autologous Breast Reconstruction
Autologous flap reconstruction following mastectomy remains the gold standard approach, with high levels of patient satisfaction.
Implant-Based Breast Reconstruction
Implant-based breast reconstruction is less invasive with shorter recovery but may require more maintenance and has risks.
Secondary Breast Reconstruction
Secondary revision procedures enhance aesthetic outcomes and correct deformities, making them a standard part of the process.
Primary Contributor: Dr Kurt Lee Chircop, Educational Fellow.
Reviewer: Dr Waruguru Wanjau, Educational Fellow.
Overview of Oncological Breast Reconstruction
Oncoplastic breast surgery combines tumor resection, through partial or complete removal of the breast gland, with reconstruction using either alloplastic or autologous techniques
Oncological breast reconstruction requires a patient-centered approach involving careful decision-making tailored to individual needs. Key factors include tumor size, location, and patient-specific considerations, which help guide critical decisions regarding,
- Timing of Reconstruction: Immediate reconstruction performed at the time of mastectomy versus delayed reconstruction performed after cancer treatment.
- Type of Reconstruction: Options include alloplastic (implant-based) or autologous (tissue-based) reconstruction methods.
- Cancer Treatment:
- Mastectomy removes all breast tissue, indicated for large/multicentric tumors or high-risk patients (e.g., BRCA mutations). Types include total, skin-sparing (preserves skin), & nipple-sparing (retains NAC and skin).
- Lumpectomy is tumor excision with a margin of healthy tissue typically followed by radiation.
- Adjuvant/neoadjuvant chemotherapy, radiotherapy, and long-term hormone therapy (e.g., Tamoxifen, Anastrozole) are integral to surgical planning.
The image below illustrates a left skin-sparing mastectomy and implant reconstruction.
Preoperative Assessment in Oncoplastic Breast Reconstruction
A comprehensive preoperative assessment guides the choice of reconstructive options by evaluating oncological, anatomical, and patient-specific factors.
History
- General Health: Assess obesity, smoking, prior thromboembolic events, and hypercoagulable conditions.
- Oncological Background: Include tumor size, location, prior treatments, and planned adjuvant therapies (e.g., radiation). Radiation can affect flap viability and timing.
- Hormonal Therapy: Evaluate the impact of medications like tamoxifen on surgical planning and assess for hypercoagulable risks.
- Family History: Discuss genetic risks, offering testing and prophylactic options for patients with a history of breast or ovarian cancer.
Physical Examination
A thorough physical examination is essential for planning oncoplastic breast reconstruction. Key factors include the breast footprint, soft tissue (conus), and skin envelope (Blondeel, 2009).
- Footprint: The breast’s outline on the chest wall, defined by the inframammary fold (IMF), anterior axillary line, and sternal midline.
- Soft Tissue (Conus): Determines the three-dimensional breast shape and volume, with lower pole fullness and maximum projection at the nipple-areola complex.
- Skin Envelope: Maintains breast shape. Excess skin causes ptosis, deficiency results in flattening, and quality impacts contour stability.
These factors should be evaluated alongside formal measurements & assessments.
Breast Assessment
- Breast Size, Ptosis, and Asymmetry: Key for symmetry and reconstruction planning.
- Skin Quality and Tethering: Includes scars and radiation effects that may impact reconstruction.
- Pinch Test Measurement: Measures skin thickness at the superior pole and IMF to determine implant suitability (Tepper, 2010).
The image below illustrates a post-radiotherapy breast assessment.
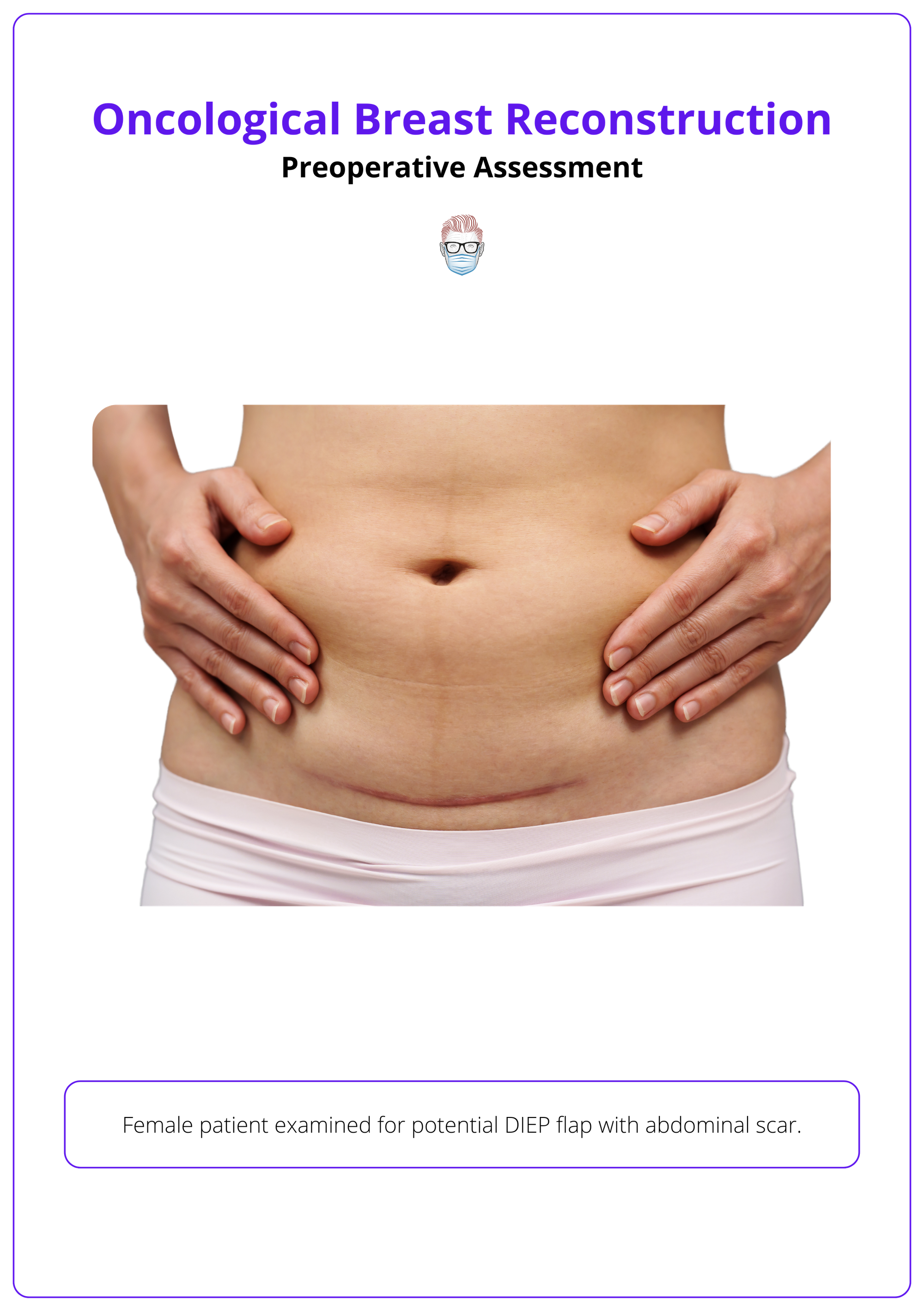
Donor Site Evaluation
- Abdomen: Assess for adequate soft tissue volume and prior scarring. Liposuction history is not a contraindication, but prior abdominoplasty typically is.
- Alternate Sites: Evaluate thighs, gluteal regions, or lumbar areas for S-GAP, TUG, or stacked flaps (Hamdi, 2013).
The donor site examination is illustrated below.
Additional Measurements
- Chest Circumference: Crucial for implant sizing.
- BMI: High BMI increases complication risk, while low BMI may limit autologous tissue options.
This integrated approach ensures accurate evaluation of both the breast and donor sites, guiding individualised reconstructive plans.
Use CT angiography or MRA to map perforators and assess tissue perfusion, especially for complex reconstructions.
Timing of Oncological Reconstruction
Reconstruction timing is determined by cancer stage, planned adjuvant therapies, and patient-specific factors to optimize safety, aesthetics, and recovery.
The decision on reconstruction timing — immediate, delayed, or delayed-immediate — depends on individual oncologic and patient factors. Each approach has unique benefits and challenges, and the optimal choice requires collaboration between surgical teams.
Immediate Reconstruction
Immediate reconstruction is performed at the time of mastectomy. There is continual discussion in the literature regarding the impact on complication rates and enhanced psychological outcomes.
- Benefits: Immediate reconstruction reduces the psychological impact of mastectomy, avoids multiple surgeries, and preserves the inframammary fold and skin envelope (Albornoz, 2013).
- Outcomes: Strong patient-reported outcomes, including improved body image and satisfaction, are associated with immediate reconstruction combined with symmetry procedures (Colwell, 2014).
- Technical Considerations: Adequate perfusion of the mastectomy flap is critical for success, particularly with implant-based methods (Phillips 2016). Intraoperative angiography can aid in assessing flap viability and decision-making (Kalus, 2016).
- Radiation Considerations: Contralateral symmetry procedures during initial surgery can account for post-radiation fibrosis by reconstructing the cancer side larger.
A postoperative patient with a left-sided immediate unilateral DIEP flap reconstruction is illustrated below.
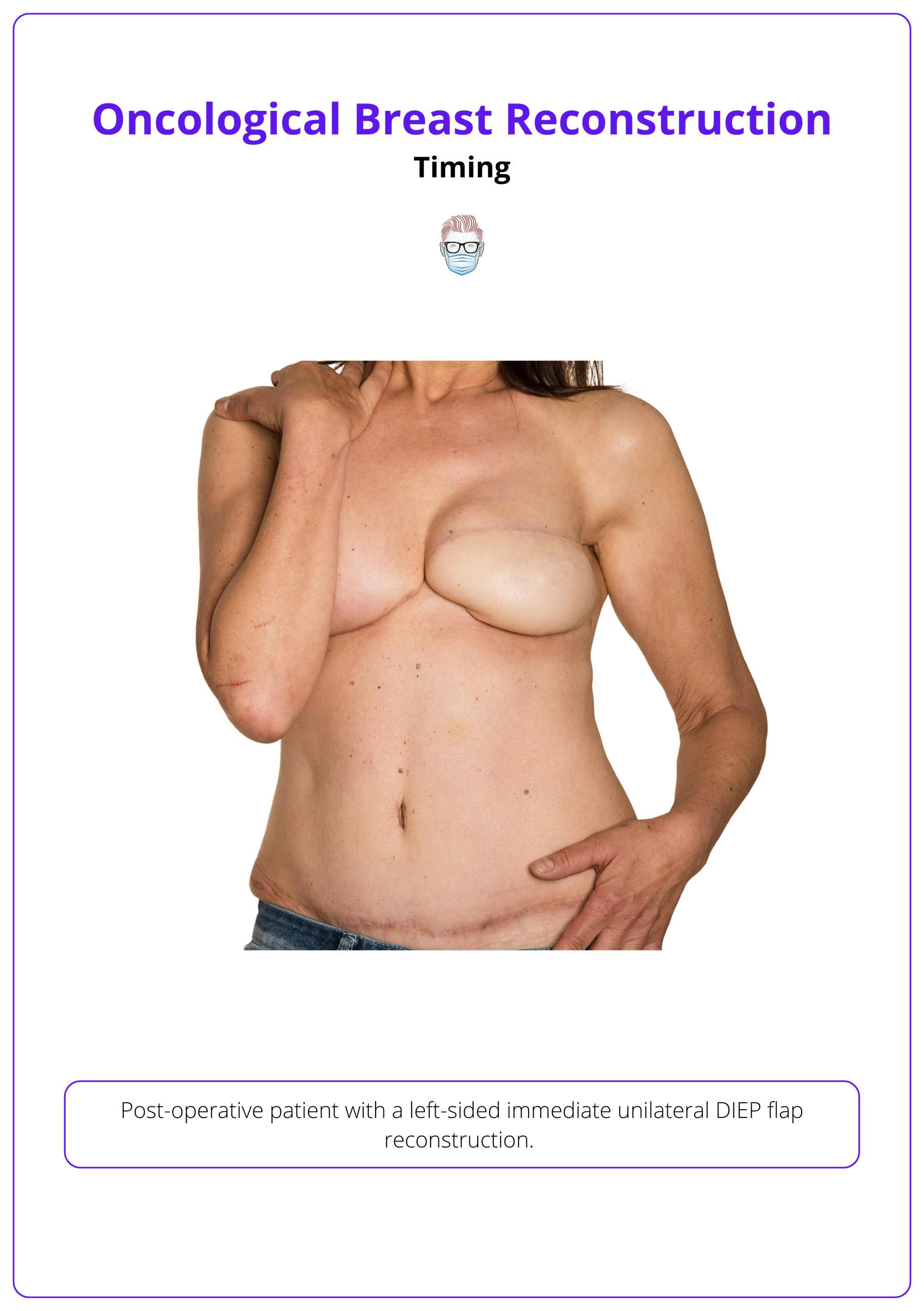
Requires well-perfused mastectomy flaps for successful outcomes, especially in implant-based methods.
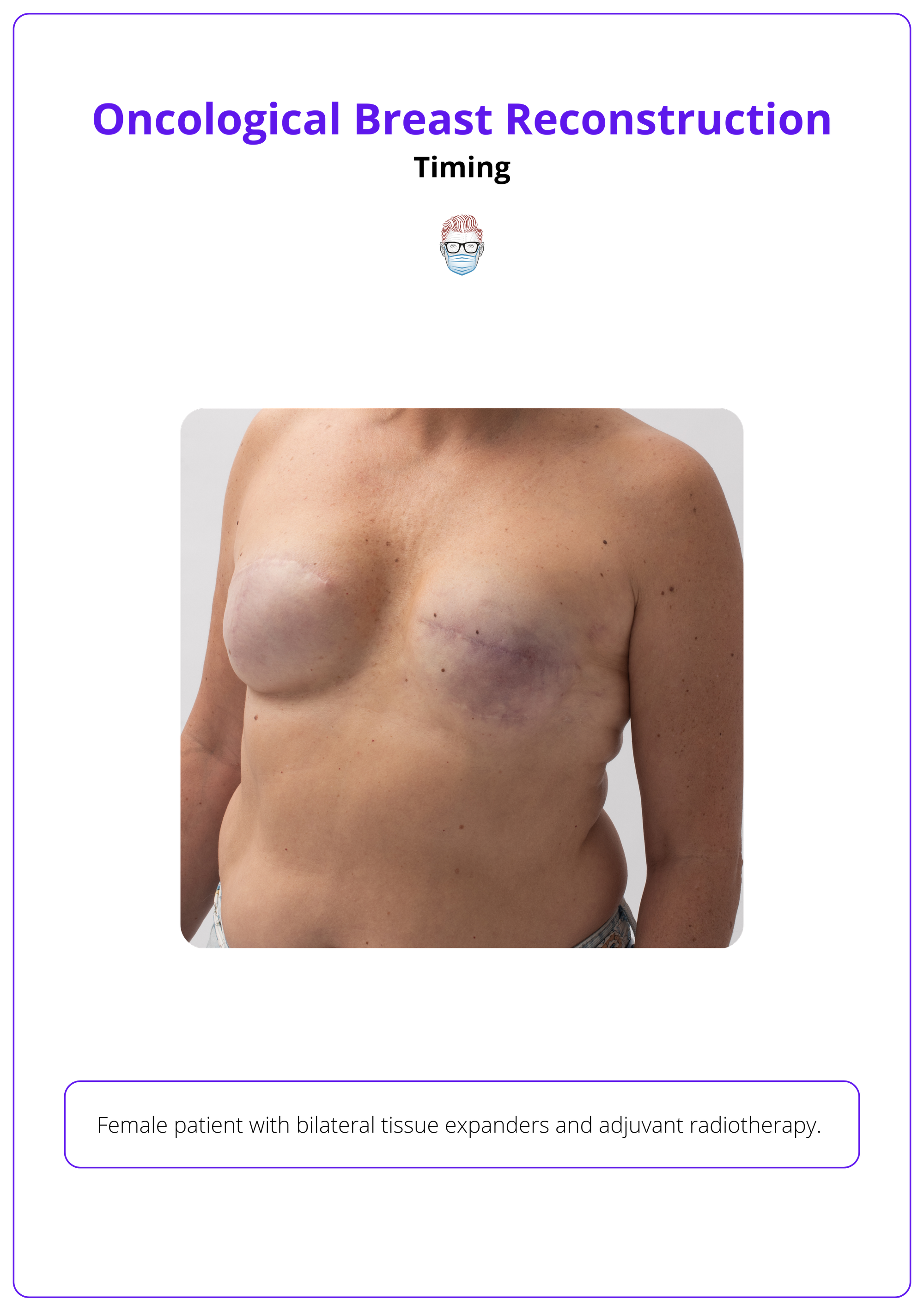
Delayed Reconstruction
Delayed reconstruction is performed in a separate operation after mastectomy, often reserved for high-risk patients or those requiring radiotherapy.
- Indications: Patients with poor wound healing potential (e.g., active smokers) or post-mastectomy radiotherapy requirements benefit from delayed reconstruction to minimize complications (El-Sabawi, 2016).
- Challenges: Radiation-induced skin fibrosis often necessitates autologous flaps for volume and aesthetic restoration (Muresan, 2017).
- Complications: Complication rates are higher compared to immediate reconstruction (e.g., 57% vs. 24%), highlighting the need for careful patient counseling (Davila, 2013).
Delayed-Immediate Reconstruction
This hybrid approach involves placing a tissue expander during mastectomy, with final reconstruction delayed until after radiotherapy completion.
- Advantages: Balances the aesthetic benefits of immediate reconstruction with oncologic safety (Olsen, 2017).
- Flexibility: Allows for clear margin assessment and radiotherapy before the final reconstruction, reducing risks of major complications while maintaining good aesthetic outcomes (Sbitany et al., 2017).
A patient with bilateral tissue expanders and adjuvant radiotherapy is illustrated below.
Single-stage reconstruction avoids a second surgery but can stress the skin envelope, especially in cases of skin reduction or poor skin quality (Roostaeian, 2012).
Decision-Making Process for Oncoplastic Breast Reconstruction
Tailored breast reconstruction balances oncologic needs, radiation therapy, anatomy, and patient preferences to achieve optimal outcomes.
Creating a patient-specific reconstruction plan requires integrating cancer treatment needs, anatomical considerations, patient goals, and psychosocial factors.
1. Oncologic Requirements
- Breast-Conserving Surgery: Smaller tumors may only require minor reconstructions, often achieved with local tissue rearrangement.
- Mastectomy Candidates: Larger tumors, multicentric disease, or extensive nodal involvement often necessitate mastectomy. Reconstruction options should account for oncologic safety, such as margin clearance and future treatment plans (e.g., re-excision risks).
2. Anticipated Radiation Therapy
- No Radiation: Immediate implant or autologous reconstruction is appropriate, offering aesthetic and psychological benefits.
- Radiation Expected: Delayed autologous reconstruction minimizes complications such as capsular contracture, fibrosis, or implant failure. Hybrid options, such as delayed-immediate reconstruction, may be beneficial for uncertain radiotherapy plans.
3. Patient Anatomy and Body Habitus
- Ample Donor Tissue: Autologous techniques, like DIEP or PAP flaps, are ideal for patients with sufficient abdominal, thigh, or gluteal tissue.
- Low Body Fat: Thin or low-BMI patients may benefit from implant-based reconstruction, though contour irregularities or rippling may require fat grafting.
4. Patient Preferences and Psychosocial Factors
- Willingness for Staged Procedures: Patients comfortable with multiple procedures may benefit from two-stage implant reconstruction or delayed flap techniques for improved outcomes.
- Single-Stage Preference: Direct-to-implant or immediate autologous reconstruction offers faster results with minimal operative stages (Berlin, 2019).
- Psychosocial Goals: Patients with a strong focus on body image and natural feel may prefer autologous techniques, while those prioritizing shorter recovery or minimal surgeries may opt for implant-based options.
5. Additional Considerations
- Comorbidities: Active smokers, diabetics, or patients with poor healing potential may require delayed reconstruction for reduced risk.
- Symmetry Goals: Consider contralateral procedures (reduction, augmentation, mastopexy) to enhance symmetry.
Autologous Breast Reconstruction
Autologous reconstruction remains the gold standard, providing natural aesthetics, high patient satisfaction, and versatile options for diverse patient needs.
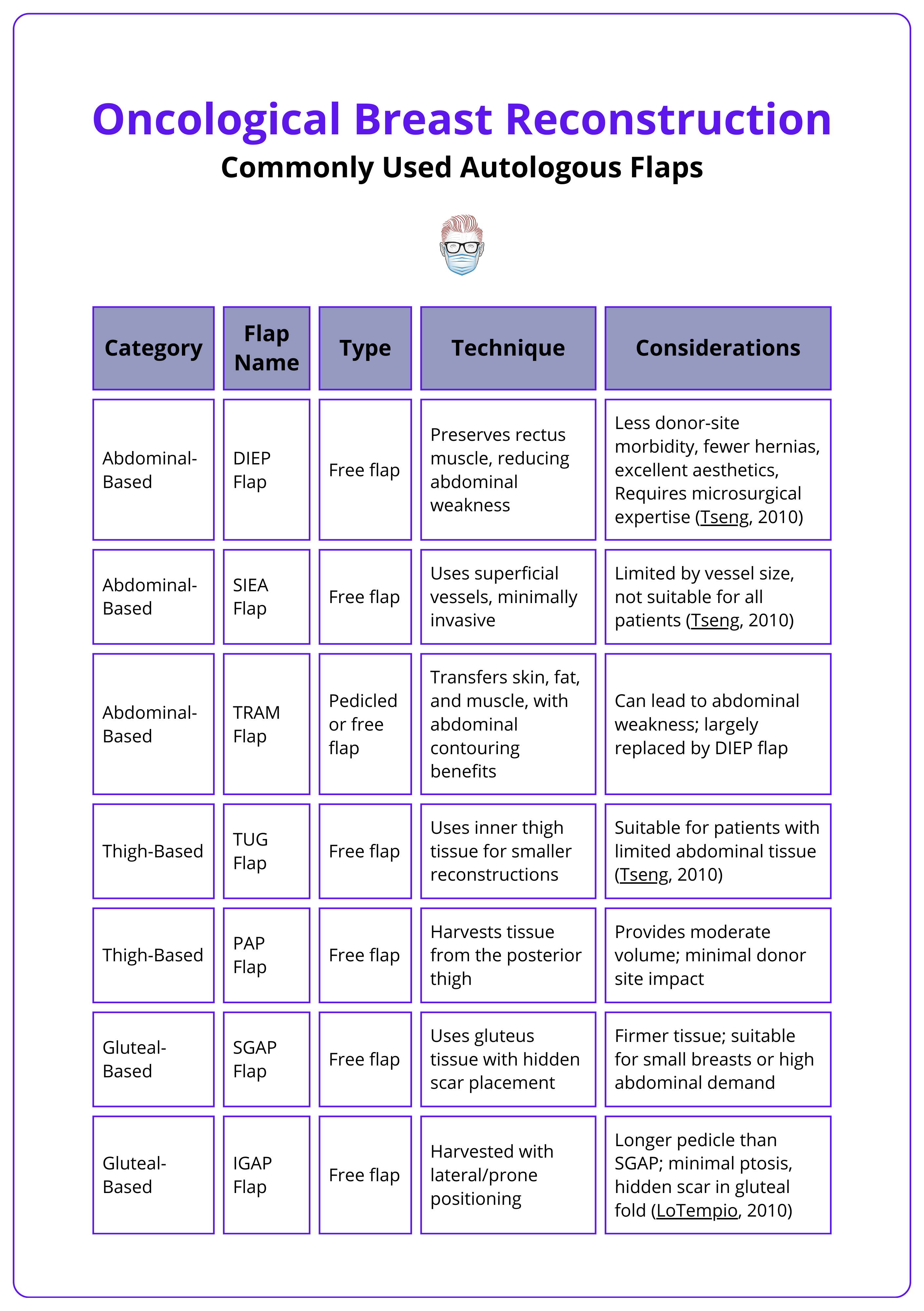
Autologous reconstruction recreates the breast mound using the patient’s own tissue, offering natural aesthetics and long-lasting results. Techniques include local and free flaps from the abdomen, back, and gluteal regions, as well as free fat transfer (Macadam, 2017).
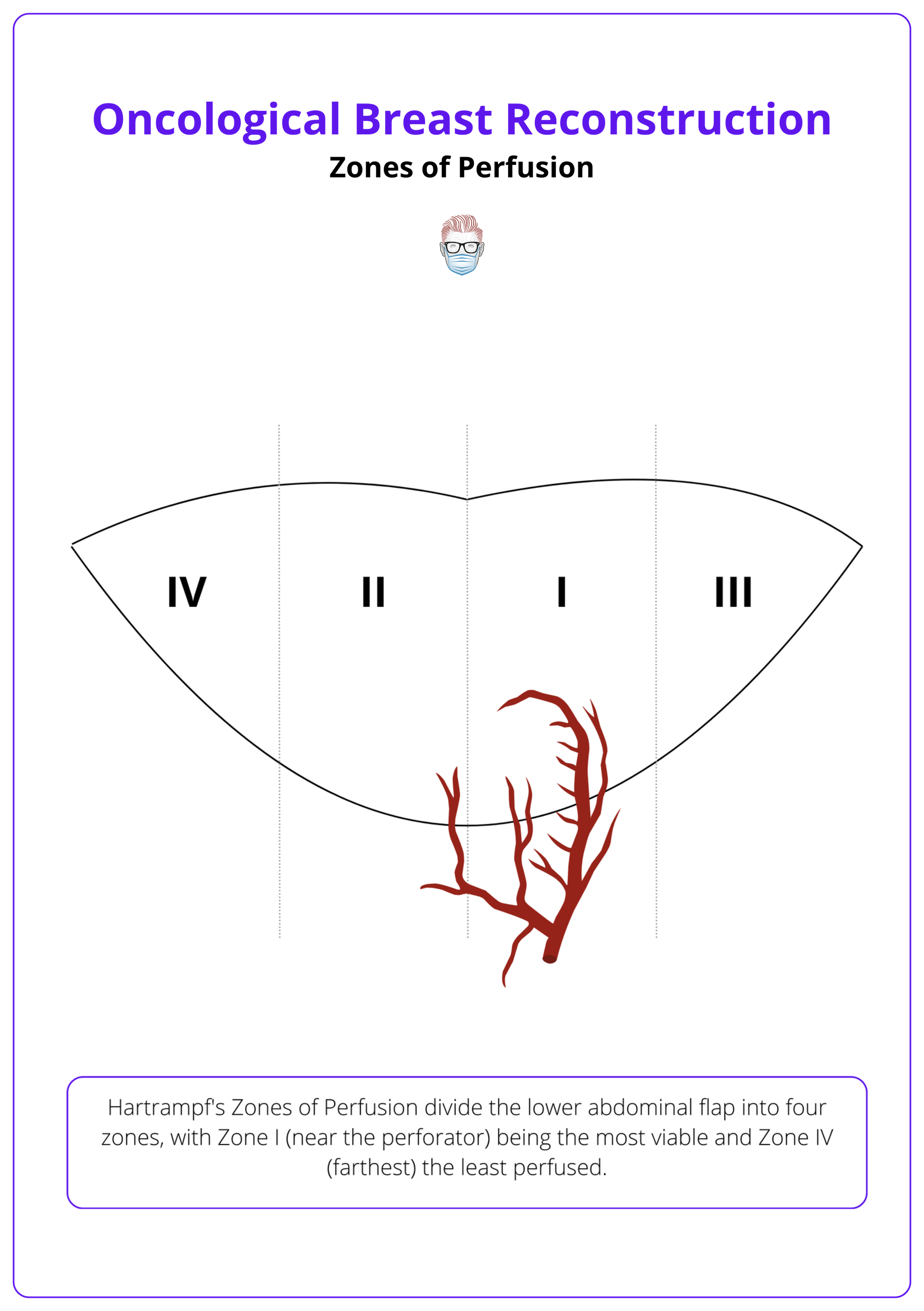
Abdomen-Based Flaps
Abdominal flaps are the first-line option due to their volume, pliability, and similarity to breast tissue.
- DIEP Flap: Preserves muscle for reduced donor-site morbidity. Provides excellent outcomes but requires advanced microsurgical skills to avoid complications like fat necrosis or flap loss.
- SIEA Flap: Avoids muscle or fascia harvest but is limited by variable vascular anatomy, feasible in only 30% of patients.
- TRAM Flap (Pedicled and Free): Pedicled relies on the superior epigastric artery; free TRAM uses the inferior epigastric artery for better perfusion and reduced fat necrosis. Risks include hernias and bulging, minimized by muscle-sparing techniques or mesh reinforcement.
The zones of perfusion are illustrated below.
Gluteal-Based Flaps
Gluteal flaps are secondary options for patients lacking adequate abdominal tissue, offering reliable volume but requiring technical expertise.
- Superior Gluteal Artery Perforator (SGAP) Flap: Harvests upper gluteal tissue with scars concealed in clothing. Precise dissection is needed near the piriformis muscle. Risks include contour deformities and asymmetry if donor volume is insufficient.
- Inferior Gluteal Artery Perforator (IGAP) Flap: Uses lower gluteal tissue with scars hidden in the infragluteal crease. Offers a longer pedicle than SGAP but risks sciatic nerve irritation. Careful dissection is required to protect the posterior femoral cutaneous nerve and ensure adequate perfusion.
Autologous reconstruction, like DIEP flaps, delivers higher patient satisfaction and better aesthetic and psychosocial outcomes than implants (Pirro, 2017).
Thigh-Based Flaps
Thigh flaps are versatile and increasingly popular for smaller reconstructions or as supplementary volume.
- PAP Flap: Offers robust volume with well-concealed scars. Pedicle length and vessel caliber make it suitable for larger reconstructions.
- TUG Flap: Suitable for small reconstructions but risks lymphedema and widened scars.
Back-Based Flaps
Back-based flaps provide alternative options for reconstruction when abdominal or thigh tissue is inadequate.
- Latissimus Dorsi (LD) Flap: Reliable regional flap, often combined with implants. May impair shoulder function and is best for patients with limited tissue or prior abdominal surgeries (Sood, 2018).
- Lumbar Artery Perforator (LAP) Flap: Offers pliable tissue and flank contouring but has shorter pedicles and requires multiple position changes, increasing complexity.
Advantages and Limitations
Autologous reconstruction offers significant benefits but comes with notable challenges that require careful patient selection and surgical expertise.
Advantages
- Provides natural-looking, durable results with superior texture and aesthetics.
- Avoids synthetic materials, making it ideal for radiated tissues.
- Fewer revisions compared to implants, ensuring long-term patient satisfaction.
Limitations
- Longer recovery periods due to complex surgical techniques.
- Risk of donor-site complications, including hernias, lymphedema, and fat necrosis.
- Requires advanced surgical expertise, increasing technical demands.
Implant-Based Breast Reconstruction
Implant-based reconstruction offers a less invasive approach with shorter recovery times, suitable for patients seeking quicker results or those without suitable donor sites, but it carries risks such as radiation sensitivity and implant failure.
Implant-based reconstruction is a less invasive option with shorter recovery times, making it ideal for patients seeking faster results or those without suitable donor sites. It carries risks such as radiation sensitivity and implant failure (Colwell, 2020). Key considerations include choosing between single- or two-stage reconstruction and determining the optimal implant pocket.
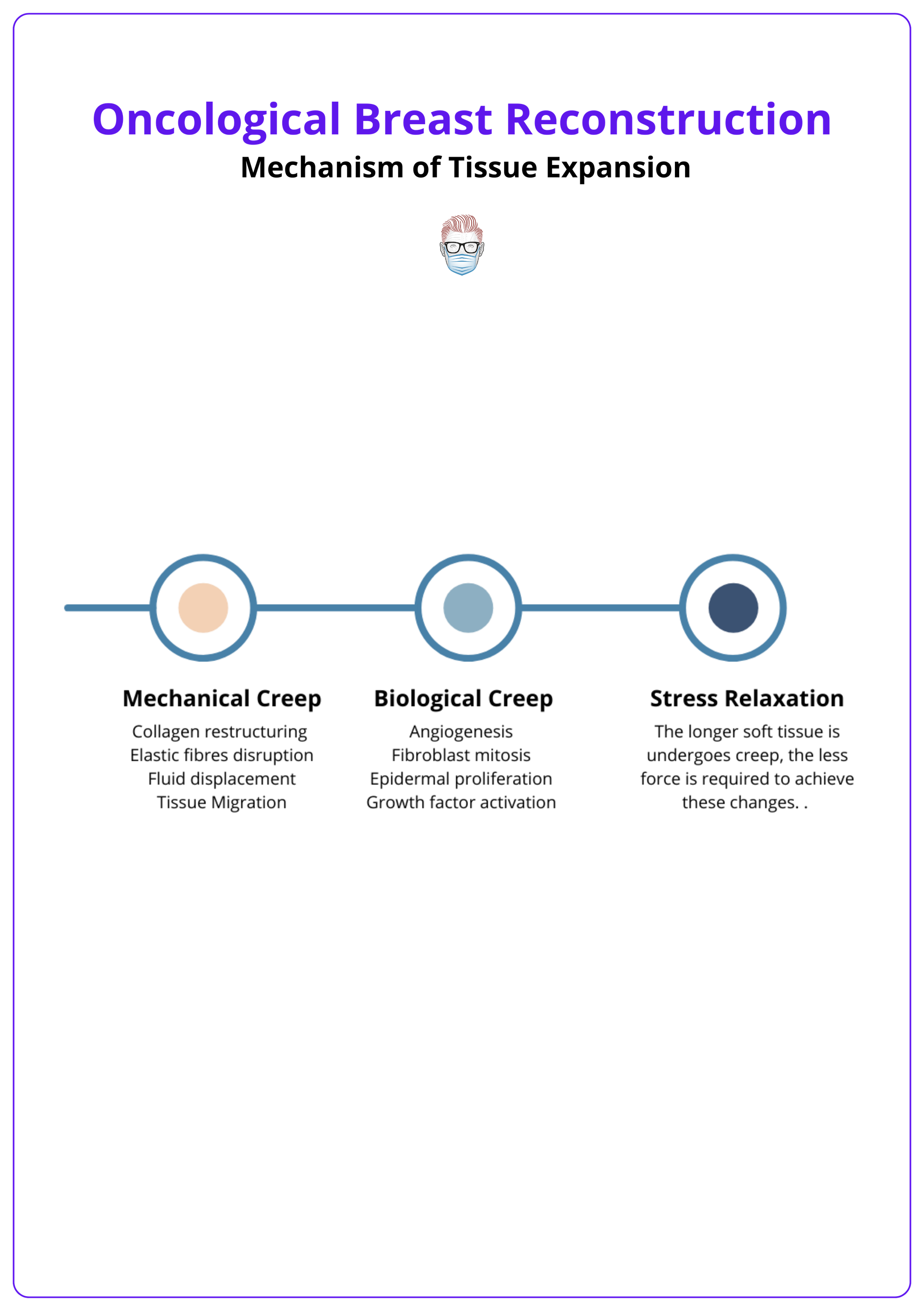
Single vs Two-Stage Reconstruction
Single-stage reconstruction is a direct-to-implant technique. A permanent implant is placed immediately after mastectomy, providing immediate results in suitable patients.
- Indications: Best suited for nipple-sparing mastectomies, older patients, or those seeking to avoid multiple surgeries. Ideal for cases with minimal skin tension, provided intraoperative flap perfusion is carefully assessed.
- Advantages: Fewer operations, faster recovery, and reduced thinning of the skin envelope.
- Challenges: Greater stress on the skin envelope, especially in cases requiring significant skin reduction.
Two-stage reconstruction involves placing a tissue expander initially, followed by a second surgery to replace it with a permanent implant.
- Indications: Recommended for significant size adjustments, compromised skin flaps, or complex symmetry corrections. Safer for higher-risk patients (e.g., smokers, obese) or less experienced surgeons.
- Advantages: Allows flexibility for size adjustments, symmetry corrections, and safer outcomes in radiation-exposed or compromised skin flaps.
- Challenges: Requires two surgeries, extending the overall treatment process.
The mechanism of tissue expansion is illustrated below.
Implant reconstructions need more maintenance, while autologous methods are more cost-effective long-term due to fewer revisions and higher satisfaction (Hansson, 2024).
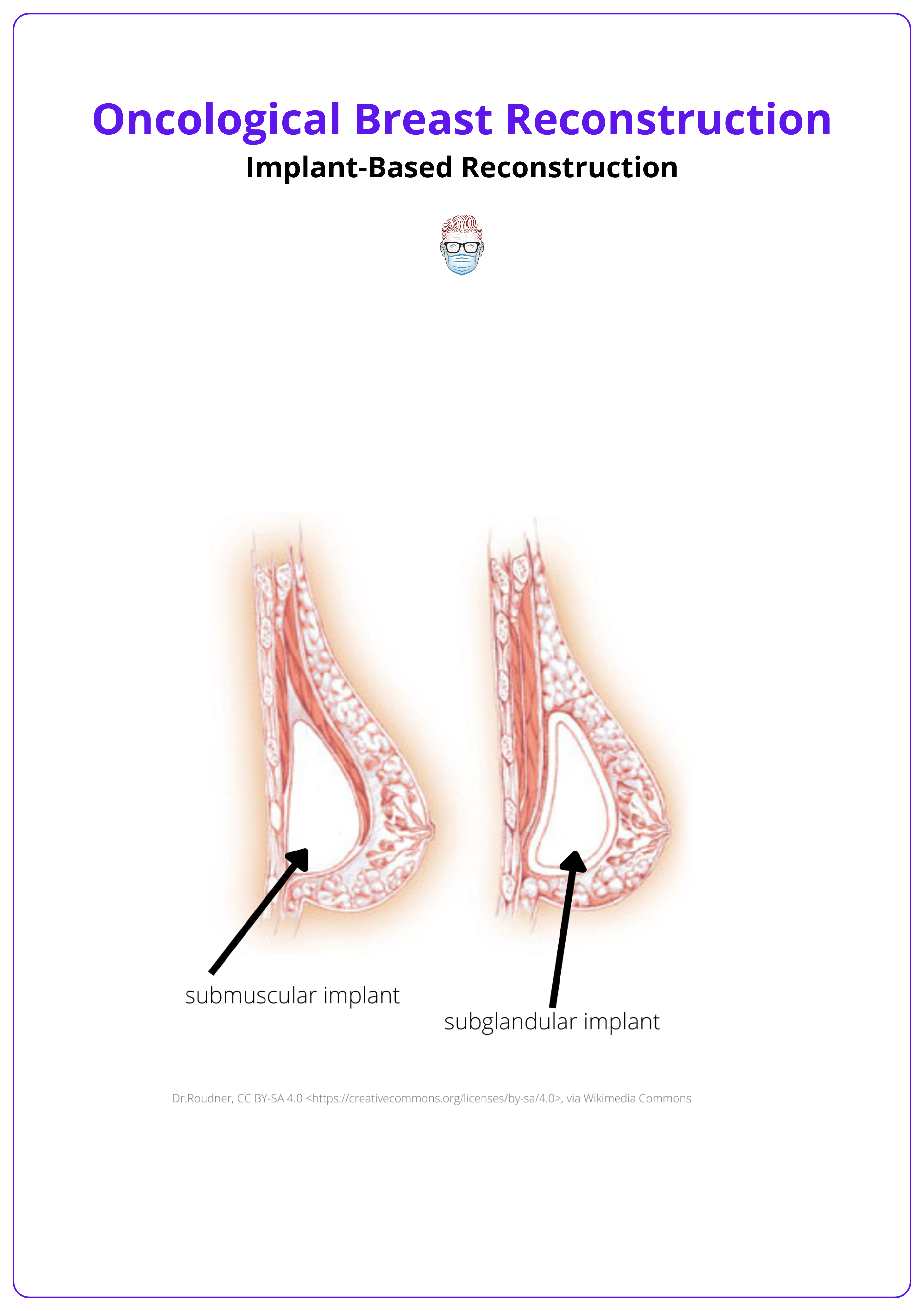
Implant Positioning
Prepectoral reconstruction places the implant above the pectoralis muscle, avoiding muscle elevation.
- Advantages: Reduces animation deformity and postoperative pain; optimal for well-vascularized skin flaps.
- Challenges: May require fat grafting to address rippling or contour irregularities.
Subpectoral reconstruction places the implant below the pectoralis muscle, providing superior coverage and lift.
- Advantages: Better superior pole coverage, with ADM enhancing stability and aesthetics.
- Challenges: Associated with animation deformity and higher postoperative pain.
The implant pocket in the subpectoral and subglandular plane is illustrated below.
ADM is used to provide soft-tissue support, reduce capsular contracture rates, and improve implant stabilization and projection. It is beneficial in both one- and two-stage reconstructions.
Secondary Breast Reconstruction
Secondary procedures are often essential in breast reconstruction to correct deformities and enhance aesthetic outcomes, making them a standard part of the reconstructive process.
Secondary breast reconstruction addresses issues arising after initial surgery, including aesthetic refinements, correcting deformities, or managing complications (Beahm, 2007). Common indications include dissatisfaction with results, radiation-induced deformities, capsular contracture, implant malposition, or failed reconstruction techniques.
Inframammary Fold (IMF) Reconstruction
The inframammary fold, a key anatomical landmark, is often disrupted during mastectomy. Restoring this structure is critical for natural breast contours. Techniques include,
- Local Tissue Rearrangement: Skin flaps are used to reconstruct the fold.
- Suture Suspension: The breast is re-suspended along the IMF.
- External Devices: Templates help recreate the contralateral breast’s IMF shape.
Implant Malposition and Deformities
Significant malpositions or deformities may require,
- New Implant Pockets: Adjusting the implant plane to improve position.
- LD Flap: Used in patients with skin deficiencies or radiation-related issues.
- Free Fat Transfer: Smooths contour irregularities and enhances volume.
- Acellular Dermal Matrices (ADM): Provides support and improves aesthetic contours.
Contralateral Breast Symmetry
Achieving balance between the reconstructed and natural breast often requires adjustments,
- Breast Reduction: Reduces the size of the contralateral breast for symmetry.
- Augmentation: Enhances smaller contralateral breasts to match the reconstructed one.
- Mastopexy: Addresses minor sagging for alignment.
NAC Reconstruction
NAC reconstruction is the final stage of breast reconstruction, performed after achieving symmetry and breast stabilization. Option include,
- Local Flaps: Techniques like Skate, Star, and C-V flaps create a three-dimensional nipple structure, though projection may reduce over time.
- Tattooing: Commonly used to recreate areola pigmentation for a realistic appearance.
- Composite Grafts: Inner thigh grafts provide tissue and pigmentation closely resembling the natural NAC.
This final step ensures optimal aesthetic results, tailored to each patient’s unique anatomy and preferences.
Conclusion
1. Purpose of Breast Reconstruction: Oncological breast reconstruction supports patients post-mastectomy or lumpectomy, through autologous, implant-based, or combination methods.
2. Types of Reconstruction: Reconstruction can be autologous, implant-based, or a mix. Timing depends on factors like radiation needs, cancer treatment, and patient anatomy.
3. Preoperative Assessment: Patient history, physical exam, and evaluations of health, body type, and oncologic needs guide reconstruction choices.
4. Decision-Making Factors: These include cancer stage, radiation plans, anatomy, and patient preferences. Patients with more body fat may benefit from autologous options, while others may prefer implants.
5. Autologous Reconstruction: Autologous reconstruction options include abdominal, thigh, and back flaps, tailored to patient anatomy.
6. Implant-Based and Secondary Reconstruction: Implant-based options allow shorter recovery but may need long-term adjustments. Secondary procedures refine outcomes and address complications.
Further Reading
- Czajka, Meghan L., and Christopher Pfeifer. "Breast cancer surgery." StatPearls [Internet]. StatPearls Publishing, 2023.
- Gilmour, A., et al. "Oncoplastic breast surgery: A guide to good practice." European Journal of Surgical Oncology 47.9 (2021): 2272-2285.
- Kummerow, Kristy L., et al. "Nationwide trends in mastectomy for early-stage breast cancer." JAMA surgery 150.1 (2015): 9-16.
- Tepper, Oren M., et al. "Mammometrics: the standardization of aesthetic and reconstructive breast surgery." Plastic and reconstructive surgery 125.1 (2010): 393-400.
- Hamdi, Moustapha. "Oncoplastic and reconstructive surgery of the breast." The breast 22 (2013): S100-S105.
- Blondeel, P. N., Hijjawi, J., Depypere, H., Roche, N., & Van Landuyt, K. (2009). Shaping the breast in aesthetic and reconstructive breast surgery: an easy three-step principle. Plastic and reconstructive surgery, 123(2), 455–462.
- Olsen, Margaret A., et al. "Comparison of wound complications after immediate, delayed, and secondary breast reconstruction procedures." JAMA surgery 152.9 (2017): e172338-e172338.
- Hansson, Emma, et al. "Gothenburg Breast reconstruction (GoBreast) II protocol: a Swedish partially randomised patient preference, superiority trial comparing autologous and implant-based breast reconstruction." BMJ open 14.7 (2024): e084025.
- Berlin, Nicholas L., et al. "Feasibility and efficacy of decision aids to improve decision making for postmastectomy breast reconstruction: a systematic review and meta-analysis." Medical Decision Making 39.1 (2019): 5-20.
- Macadam, Sheina A., et al. "Evidence-based medicine: autologous breast reconstruction." Plastic and reconstructive surgery 139.1 (2017): 204e-229e.
- Sood, Rachita, et al. "Latissimus dorsi flap in breast reconstruction: recent innovations in the workhorse flap." Cancer Control 25.1 (2018): 1073274817744638.
- Tseng, Charles Y., and Joan E. Lipa. "Perforator flaps in breast reconstruction." Clinics in Plastic Surgery 37.4 (2010): 641-654.
- LoTempio, Maria M. M.D.; Allen, Robert J. M.D.. Breast Reconstruction with SGAP and IGAP Flaps. Plastic and Reconstructive Surgery 126(2):p 393-401, August 2010. | DOI: 10.1097/PRS.0b013e3181de236a
- Pirro, Ortensia, et al. "Comparison of patient-reported outcomes after implant versus autologous tissue breast reconstruction using the BREAST-Q." Plastic and Reconstructive Surgery–Global Open 5.1 (2017): e1217.
- Colwell, Amy S., and Erin M. Taylor. "Recent advances in implant-based breast reconstruction." Plastic and Reconstructive Surgery 145.2 (2020): 421e-432e.
- Albornoz, Claudia R., et al. "A paradigm shift in US breast reconstruction: increasing implant rates." Plastic and reconstructive surgery 131.1 (2013): 15-23.
- Beahm, Elisabeth K., and Robert L. Walton. "Revision in autologous breast reconstruction: principles and approach." Clinics in Plastic Surgery 34.1 (2007): 139-162.


