In this week's edition
- ✍️ Letter from P'Fella
Only 20% stick with plastic surgery: What’s behind the drop-off? - 🤓 The Sunday Quiz
How well do you know giant cell tumours of the tendon sheath? - 🖼️ Anatomy Illustration of the Week
Henry Gray’s original drawing of the hand. - 🎓 theFellow's Corner
This week's feature: Glomus tumors - clinical scenario. - 📖 What Does the Evidence Say
Should we actually operate on Enchondromas? - 🔥 Articles of the Week
Hand tumours of soft tissue and bone, malignant melanoma in hand, & pediatric hand and wrist ganglion cysts: 3 articles with 1 sentence summaries. - 💕 Feedback
Suggest ideas & give feedback!
A Letter from P'Fella
Only 20% Stick with Plastic Surgery: What’s Behind the Drop-Off?
I’ve been looking at some interesting numbers recently, and one thing really stands out: Only 20.3% of medical students who start with an interest in plastic surgery actually stick with it through to graduation. It’s a surprising stat when you consider how dynamic and rewarding our field can be. So what’s going on? Let’s unpack it.
1. Why the Drop-Off?
When students first enter med school, many of them don’t fully understand the scope of each specialty. Plastic surgery often isn’t fully appreciated until later — by then, they might have already committed to another field. It’s like walking into a restaurant for a salad, only to realize halfway through that they serve the best steak in town — but you’re already full.
2. Late Exposure & Misconceptions
Most students think of plastic surgery as just cosmetic work, not realizing it involves critical reconstructive procedures — trauma, cancer reconstruction, hand surgery. By the time they see this diversity, many have already built connections in other fields. Without seeing the broader picture early on, students often move on.
3. Mentorship Matters
The real key here is mentorship. Early guidance and exposure to the full range of what we do can make all the difference. Getting students into the OR or giving them a chance to interact with surgeons early on could prevent them from drifting away.
Over the next 6 months, we’re launching a massive initiative targeting medical students with a three-pronged approach: theory, practice, and mentorship. The first step? A comprehensive student manual and guide tailored for those interested in plastic surgery.
Email tara@theplasticsfella.com if you are interested in getting involved.
The takeaway? We’re losing talented future surgeons because they don’t see the full picture soon enough. Let’s change that through early exposure and mentorship. If you're interested in building our textbook for students, email tara@theplasticsfella.com.
Lot of Love,
P'Fella ❤️
The Sunday Quiz
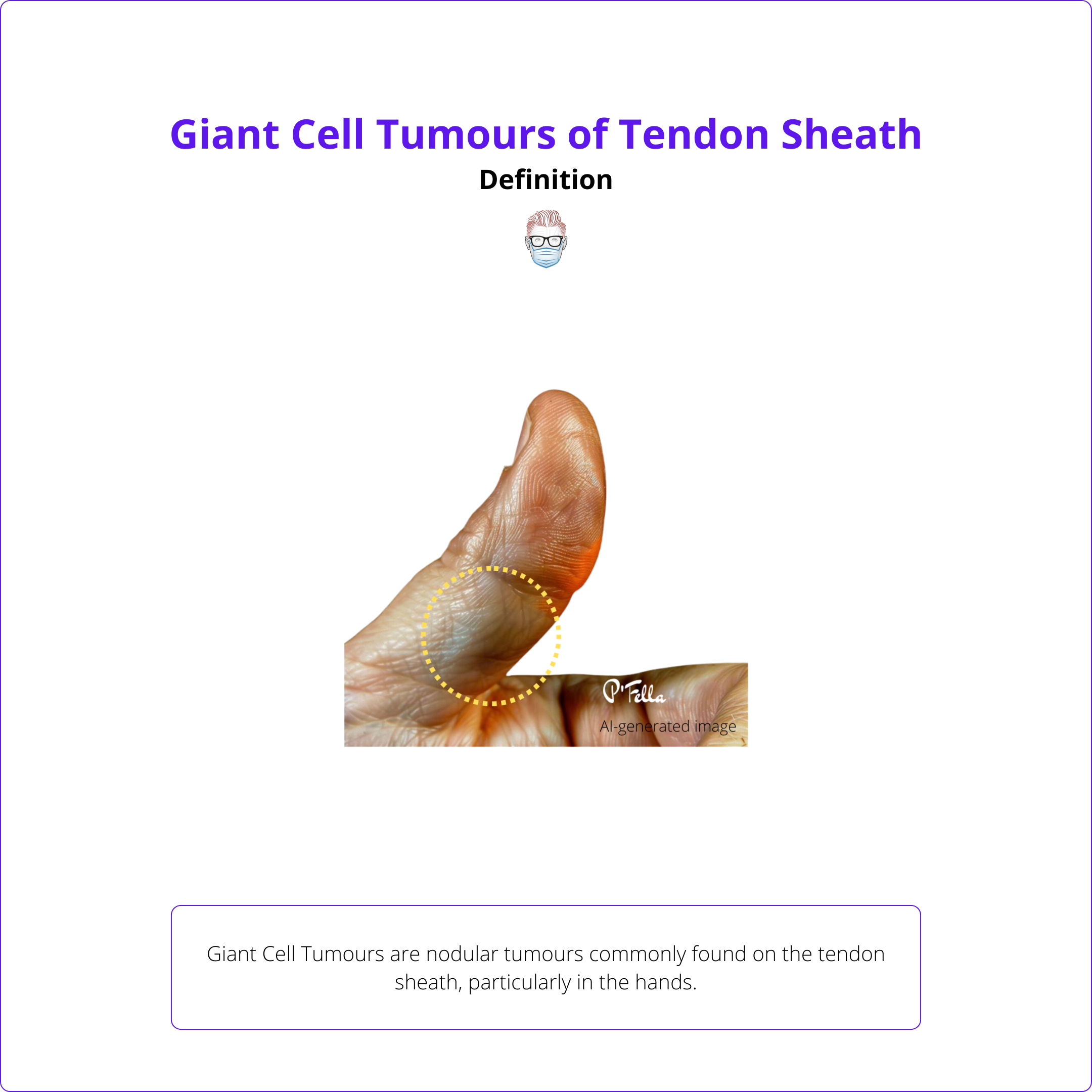
How Well Do You Know Giant Cell Tumours of the Tendon Sheath?
Welcome to the next round of The Weekly Quiz.
Each edition of thePlasticsPaper includes a quiz question designed to challenge and engage our readers. Keep your wits about you and join in every week — the winner at the end of six rounds will earn you a $100 voucher.
Anatomy Illustration of the Week
Henry Gray’s Original Drawing of the Hand
This section we feature an anatomical illustration. This edition looks at Henry Gray’s original drawing of the hand.
👇
the Fellows' Corner
This Week's Focus: Glomus Tumours - Clinical Scenario
In case you've missed out, here's a reminder to check out our fresh articles, clinical cases, and surgical techniques.
Read below for an overview of our Clinical Scenario on Glomus Tumours.
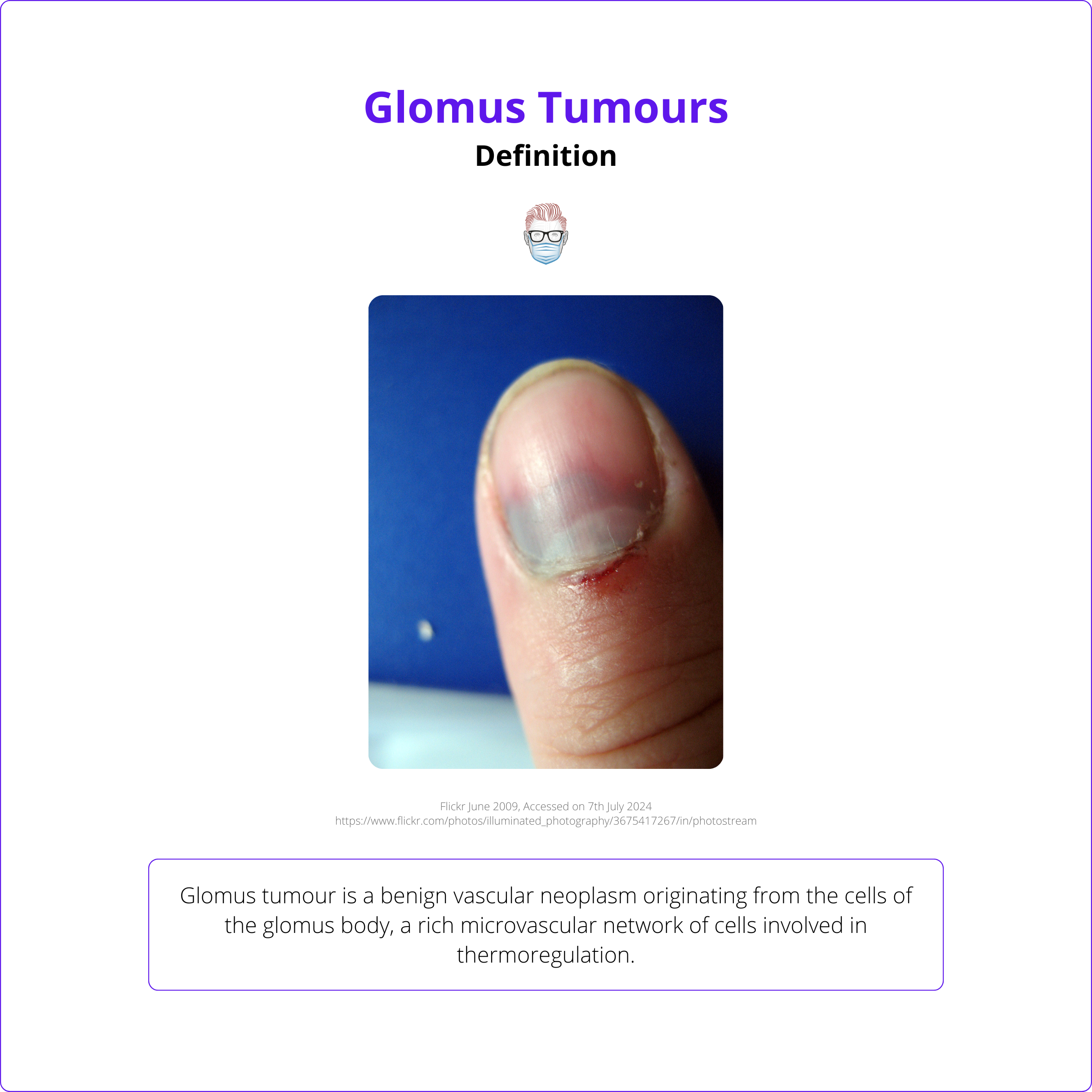
Glomus Tumours - Clinical Scenario
- Understand the classical presentation of a glomus tumour.
- Describe the pathophysiology of a glomus tumour.
- Provide a differential diagnosis for a painful digit swelling.
- Outline the investigations indicated for a glomus tumour.
- Discuss the treatment options available.
What Does the Evidence Say?
Should We Actually Operate on Enchondromas?
Management typically involves conservative treatment for small, asymptomatic lesions and surgical curettage for symptomatic or expanding lesions (Tang et al., 2015). Curettage without void augmentation is effective and cost-efficient, with low complication rates (Bachoura et al., 2015). However, some surgeons use bone grafts, bioactive materials, or cement for reconstruction (Bickels et al., 2002; Żyluk, 2021).
Pathological fractures do not significantly impact treatment outcomes, and early surgical intervention is recommended for these cases (Zhou et al., 2016). Most patients achieve complete healing and full range of motion post-surgery, regardless of the graft material used (Sassoon et al., 2012). Malignant transformation is rare, occurring mainly in patients with multiple enchondromatosis syndromes (Sassoon et al., 2012; Redgrave et al., 2021).
Overall, surgical management of hand enchondromas yields satisfactory results with low recurrence rates (Żyluk, 2021).
Articles of the Week
3 Interesting Articles with 1 Sentence Summaries
Hand tumors require differentiation between benign and malignant forms, with treatment outcomes dependent on malignancy, recurrence risk, and survival rates.
Malignant melanoma of the hand has significant diagnostic and management challenges, often diagnosed at a later stage and associated with poorer prognosis.
Around two-thirds of pediatric hand and wrist ganglion cysts are resolved spontaneously within two years without surgery or aspiration, with higher resolution rates in hand cysts compared to wrist cysts.


