In this week's edition
- ✍️ Letter from P'Fella
Young docs want balance. Old docs say tough luck. - 🤓 The Sunday Quiz
How well do you know pressure ulcers? - 🖼️ Image of the Week
Grade 4 pressure sore featured. - 🚑 Technique Tip
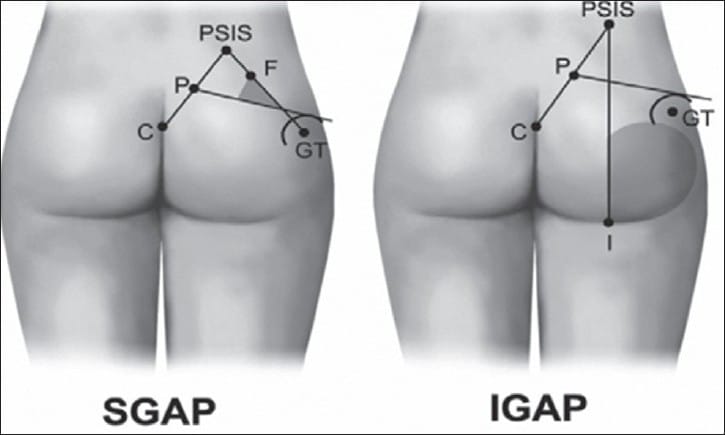
Designing the SGAP flap. - 🎓 The Fellow's Corner
This week's feature: Osteomyelitis. - 📖 What Does the Evidence Say
What's the best flap for a pressure sore? - 🔥 Articles of the Week
Cierny/Mader staging system for osteomyletitis, Necrotisiig fasciitis management, & classic paper from Mathes himself: with 1 sentence summaries. - 💕 Feedback
Suggest ideas & give feedback!
A Letter from P'Fella
Young Docs Want Balance. Old Docs Say Tough Luck.
I just came across an article from the Wall Street Journal titled, "Young Doctors Want Work-Life Balance. Older Doctors Say That’s Not the Job". It’s a hot topic, and it’s stirring up some serious debate — and I want you in on it.
There is a generational clash in medicine. Older doctors argue that long, grueling hours are just part of the job—a rite of passage they endured, so younger doctors should too. But should we keep this tradition simply because “that’s how it’s always been”? Where is this mindset really getting us?
The crazy residency schedules that became tradition weren’t about excellence—they were born from one physician trying to cover up his own issues. And yet here we are, decades later, clinging to this exhausting model like it’s some badge of honor. But let’s face it, the old expectations of endless availability are still very much in play. And those who stick to this mentality often end up in leadership, perpetuating the very culture that drives burnout. Here’s what Twitter thought about this article:
- “If we’re just replaceable cogs, why should we sacrifice everything?” It’s true — why give your whole life to a job that treats you like you’re disposable?
- “Younger doctors have it different.” Crushing student loans, skyrocketing living costs, burnout awareness, and constant tech overload make it impossible to justify the same approach of past generations. The game has changed.
- “We need to invest in future doctors.” Without solid support from day one — better education, recruitment, and training — we’re just stuck in a cycle of poor working conditions and chronic shortages.
- “Autonomy is key.” Many younger attendings say that autonomy makes all the difference. Running their own practice means they can work long hours without feeling like cogs in a machine. But that kind of freedom is hard to come by today, especially for young docs employed by massive health systems.
- “Patient safety should come first.” Who wants a doctor who’s been awake for 24 hours? Exhausted doctors make mistakes. We should all care about changing that.
- “Older doctors have played a part in this mess.” Selling out to private equity, and letting insurers dictate care — these decisions by past generations have made things tougher for today’s doctors. We’re working harder for less, and it shows.
So here’s the big question: How do we strike a balance?
I want to hear what you think. Drop your thoughts above.
With love,
P'Fella ❤️
The Sunday Quiz
How Well Do You Know Pressure Ulcers?
Welcome to the next round of The Weekly Quiz.
Each edition of thePlasticsPaper includes a quiz question designed to challenge and engage our readers. Keep your wits about you and join in every week — the winner at the end of six rounds will earn you a $100 voucher.

Image of the Week
Grade 4 Pressure Sore
In this section, we feature an anatomical illustration. This edition looks at an infected Grade 4 pressure ulcer over the right ischial tuberosity, with exposed bone.

Technique Tip
Designing the SGAP Flap
This edition looks at designing the SGAP flap. You can read more details on the technique here.
the Fellows' Corner
This Week's Focus: Osteomyelitis
In case you've missed out, here's a reminder to check out our fresh articles, clinical cases, and surgical techniques.
Read below for an overview of our article on Osteomyelitis.

Osteomyelitis
Definition
Osteomyelitis is inflammation due to infection of the bone by bacteria, mycobacteria, or fungus.
Aetiology
Osteomyelitis can result from haematogenous seeding, direct inoculation, or contiguous spread. Staphylococcus aureus is the most common pathogen.
Clinical Features
Osteomyelitis presents with pain and reduced movement. Acute cases show systemic signs of infection, while chronic cases may involve overlying skin changes and drainage through a sinus tract.
Investigations
A diagnosis of suspected osteomyelitis is confirmed by positive bone microbiology samples. MRI and FDG-PET are the most sensitive and specific imaging techniques.
Management
Targeted antibiotic therapy is the first choice for acute osteomyelitis. In subacute and chronic cases, aggressive debridement combined with an orthoplastic approach is required for definitive management.
What Does the Evidence Say?
What's the Best Flap for a Pressure Sore?
Factors associated with higher complication risks include low BMI, smoking, ischial location, and preoperative osteomyelitis (Bamba et al., 2017). Flap selection is crucial for successful outcomes, with specific flaps showing high success rates for different pressure sore locations (Foster et al., 1997).
Gluteal perforator flaps have demonstrated excellent results with low recurrence rates (Lee et al., 2006). Despite improvements in surgical techniques, pressure sore recurrence remains a significant challenge, with historical rates as high as 75-77% (Lee et al., 2006).
Articles of the Week
3 Interesting Articles with 1 Sentence Summaries
Chronic osteomyelitis demands surgical biofilm removal and adjunctive antibiotics, guided by the Cierny/Mader staging system, with reconstruction tailored to bone stability and soft-tissue health.
Necrotizing fasciitis is marked by rapid tissue destruction, friable fascia, and gray exudate without pus, requiring urgent surgical debridement and antibiotics.
Explore muscle flaps in osteomyelitis management in Mathes' publication. This approach covers infected wounds and exposed bones using microsurgical techniques for transposing muscle to various sites.


