Summary Card
Overview
NAC reconstruction uses flaps, grafts, tattooing, and combined techniques for aesthetic restoration after cancer, trauma, or surgery.
Goals
The goal of NAC reconstruction is to match the opposite nipple in size, color, position, and projection, achieving a natural appearance.
Anatomy
The nipple features dense fibrous tissue and smooth muscle fibers, connected to 15-20 lactiferous ducts. The pigmented areola houses lubricating Montgomery glands.
Indications
NAC reconstruction is indicated post-mastectomy, for congenital issues, trauma, and gender-affirming surgery; contraindications include active cancer and poor health ± smoking.
Preoperative Marking and Positioning
Preoperative NAC marking uses key landmarks to ensure symmetry, positioning the nipple 19-21 cm from the sternal notch.
NAC Reconstruction Techniques
Nipple reconstruction uses flap techniques and augmentation methods, while areolar reconstruction can be done simultaneously or delayed, such as with 3D tattooing.
Areolar Reconstruction Techniques
Areolar reconstruction can be done at the time of nipple reconstruction or as a delayed procedure (e.g. 3D tattooing).
Primary Contributors: Maitumelo Imeldah Motoroko, Maxim Devine, and Richard Zinn
Overview of NAC Reconstruction
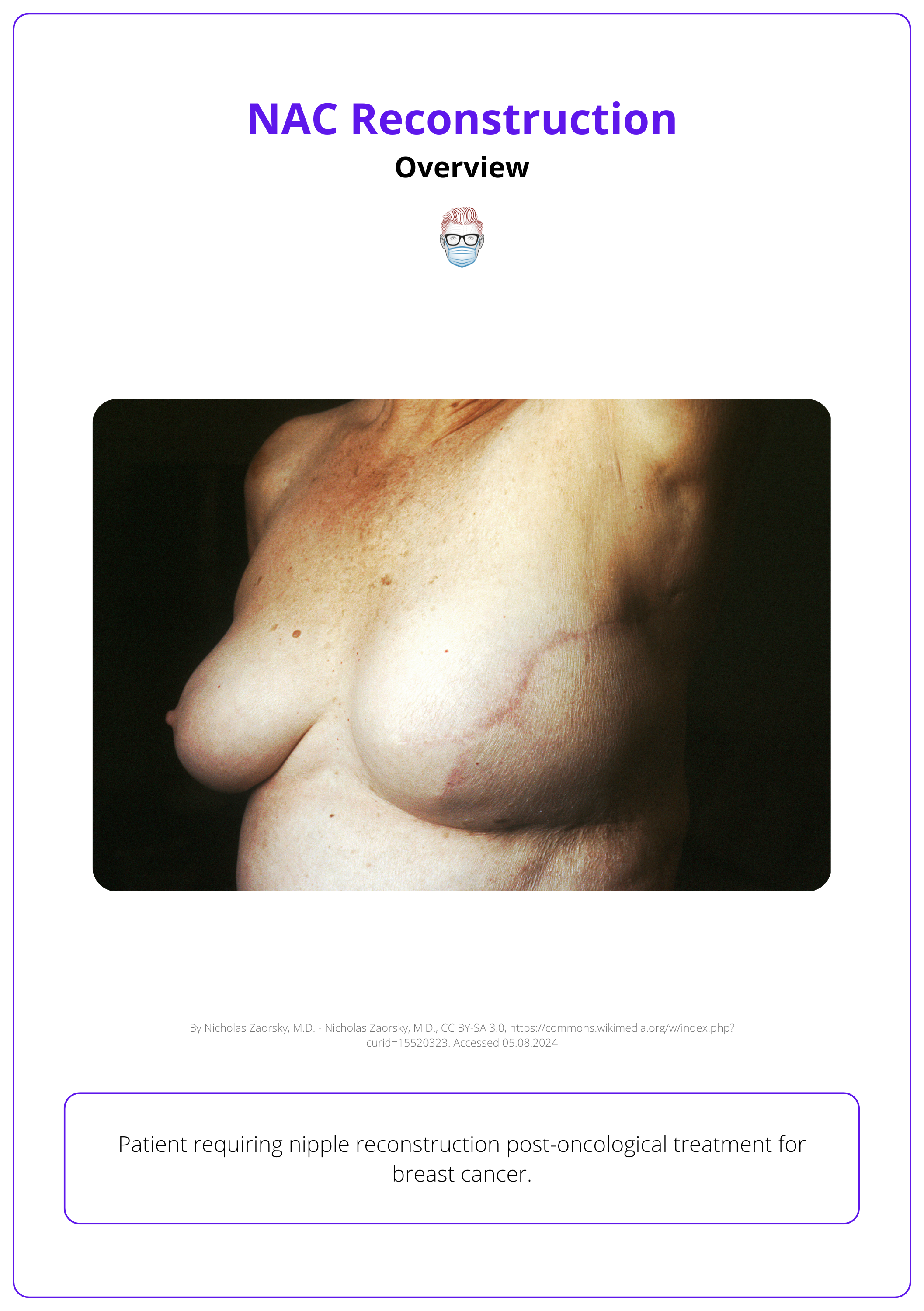
NAC reconstruction uses flaps, grafts, tattooing, and combined techniques for aesthetic restoration after cancer, trauma, or surgery.
Nipple Areolar Complex (NAC) Reconstruction, first introduced in the 1940s using grafting techniques, has expanded to include local flaps, tattooing, combination methods, and tissue engineering (Braza et. al, 2024).
Common indications for NAC reconstruction include:
- Oncology/Cancer excision
- Post-traumatic events
- Developmental pathology
- Cosmetic breast surgery complications
The image below illustrates a patient requiring an NAC reconstruction.
Goals of NAC Reconstruction
The goal of NAC reconstruction is to match the opposite nipple in size, color, position, and projection, achieving a natural appearance.
The main goal of NAC reconstruction is to create a symmetrical nipple-areolar complex that matches the opposite side in size, colour, position, and projection for a natural appearance.
Key objectives include:
- Symmetry: Align the reconstructed nipple and areola with the opposite side, or the overall breast aesthetics.
- Projection: Ensure adequate nipple projection to enhance the breast's three-dimensional appearance.
- Pigmentation: Match the reconstructed NAC’s color to the patient's natural pigmentation, using tattooing or grafts as needed.
- Durability: Maintain the NAC's shape, size, and projection over time, preventing flattening or pigment loss.
- Minimizing Complications: Use careful surgical techniques to reduce risks like infection, necrosis, and scarring.
- Sensation: preserve/restore sensation in reconstructed NAC if possible.
The image below illustrates the goals of NAC reconstruction.
Tailor the reconstruction to the patient’s specific cultural and personal preferences regarding NAC appearance, including size, shape, and colour (Farhadi, 2006).
Anatomy of NAC Reconstruction
The nipple features dense fibrous tissue and smooth muscle fibers, connected to 15-20 lactiferous ducts. The pigmented areola houses lubricating Montgomery glands.
A clear understanding of the nipple-areolar complex (NAC) anatomy, including the distinction between the nipple and areola and their neurovascular components, is crucial for effective reconstruction.
Areolar
The pigmented area around the nipple, typically 38-50mm in diameter, contains Montgomery glands that secrete oil to protect and lubricate the nipple during breastfeeding.
Nipple
The nipple is a central, protruding structure composed of dense fibrous tissue and smooth muscle fibers, connected to approximately 15-20 lactiferous ducts, each linked to a lobe of the mammary gland. The smooth muscle fibers, both circular and longitudinal, enable the nipple to become erect in response to stimuli like cold, touch, or arousal.
The image below illustrates the anatomy of the nipple-areolar complex.
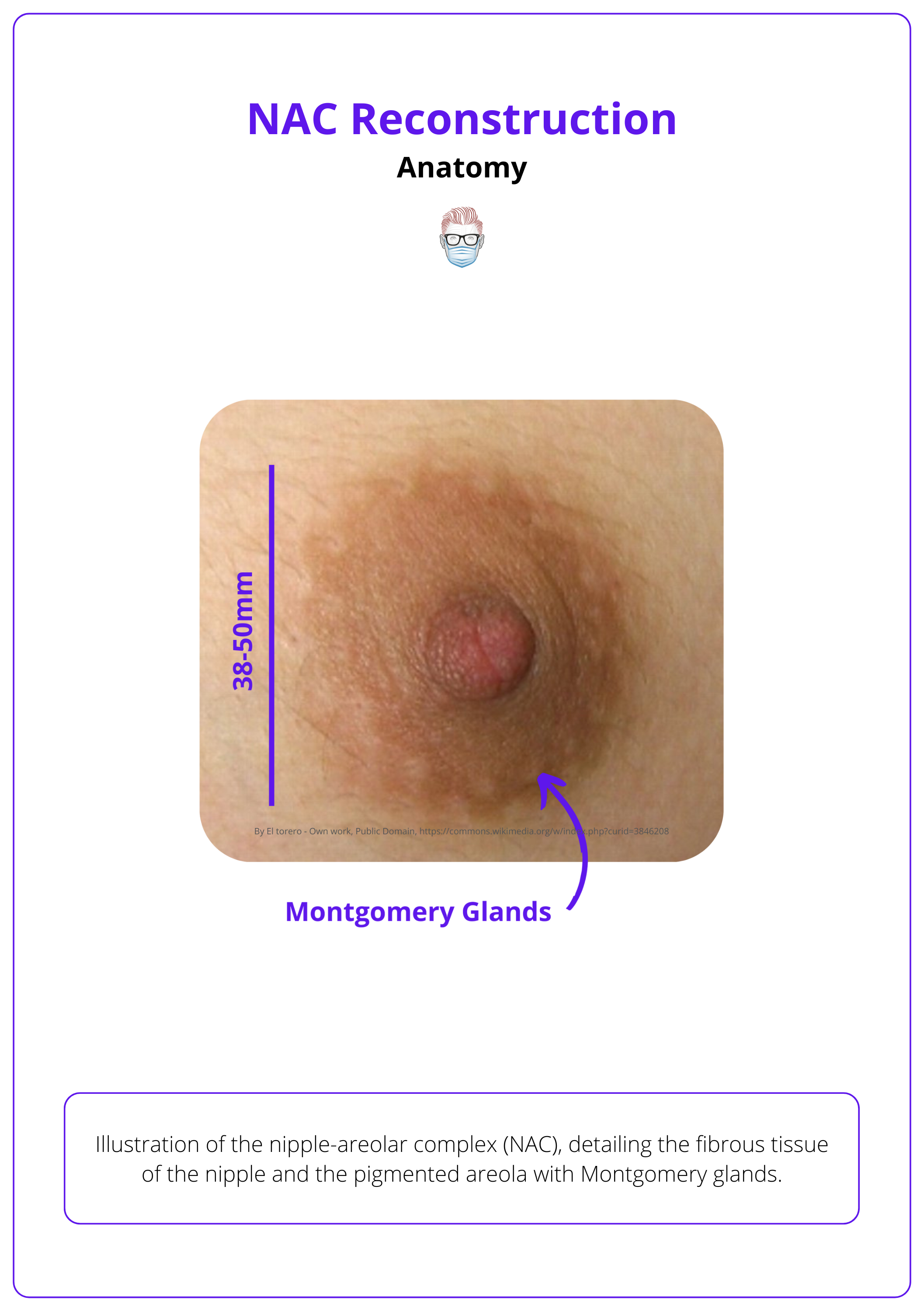
Other anatomical features to consider include:
- Arterial Supply: internal mammary, lateral thoracic, thoracoacromial, & intercostal arteries.
- Venous Drainage: into the internal thoracic and axillary veins.
- Sensation: primarily innervated by the fourth intercostal nerve.
- Autonomic Control: Smooth muscle fibers in the nipple respond to stimuli, enabling erection (Zucca-Matthes et. al, 2016).
Areolar pigmentation can vary widely among individuals.
Indications for NAC Reconstruction
NAC reconstruction is indicated post-mastectomy, for congenital issues, trauma, and gender-affirming surgery; contraindications include active cancer and poor health ± smoking.
NAC reconstruction is considered only after completing breast reconstruction and chemoradiation, with a thorough evaluation of medical history, including prior surgeries, donor site availability, and patient preferences.
Indications
- Post-Mastectomy: Restores breast appearance after mastectomy.
- Breast Reduction/Mastopexy: Repositions or reconstructs NAC after large reductions or complications.
- Congenital Conditions: Corrects anomalies like Poland syndrome.
- Trauma/Burns: Reconstructs NAC lost to injury.
- Gender-Affirming Surgery: Essential for transgender chest reconstruction.
Contraindications
Avoid NAC reconstruction in cases of active cancer treatment, poor tissue viability, or compromised health. Other considerations include psychosocial factors and conditions that may affect healing (smoking, obesity, radiation, nutritional)
Preoperative Marking and Positioning for NAC Reconstruction
Preoperative NAC marking uses key landmarks to ensure symmetry, positioning the nipple 19-21 cm from the sternal notch.
Preoperative marking of the NAC is crucial for achieving a natural, symmetrical outcome in breast reconstruction. Use fixed landmarks such as the sternum, clavicle, and inframammary fold to ensure symmetry.
Identify Landmarks
Several well-established landmarks guide the 'ideal' nipple position:
- 19-21 cm from the nipple to the suprasternal notch
- Midhumeral point
- 8-10 cm from the upper pole of the breast
- Pitanguy's point (Inframammary fold transposed onto the anterior breast)
- Areola diameter: Typically 38-50mm
The image below illustrates the landmarks for 'ideal' nipple positions.
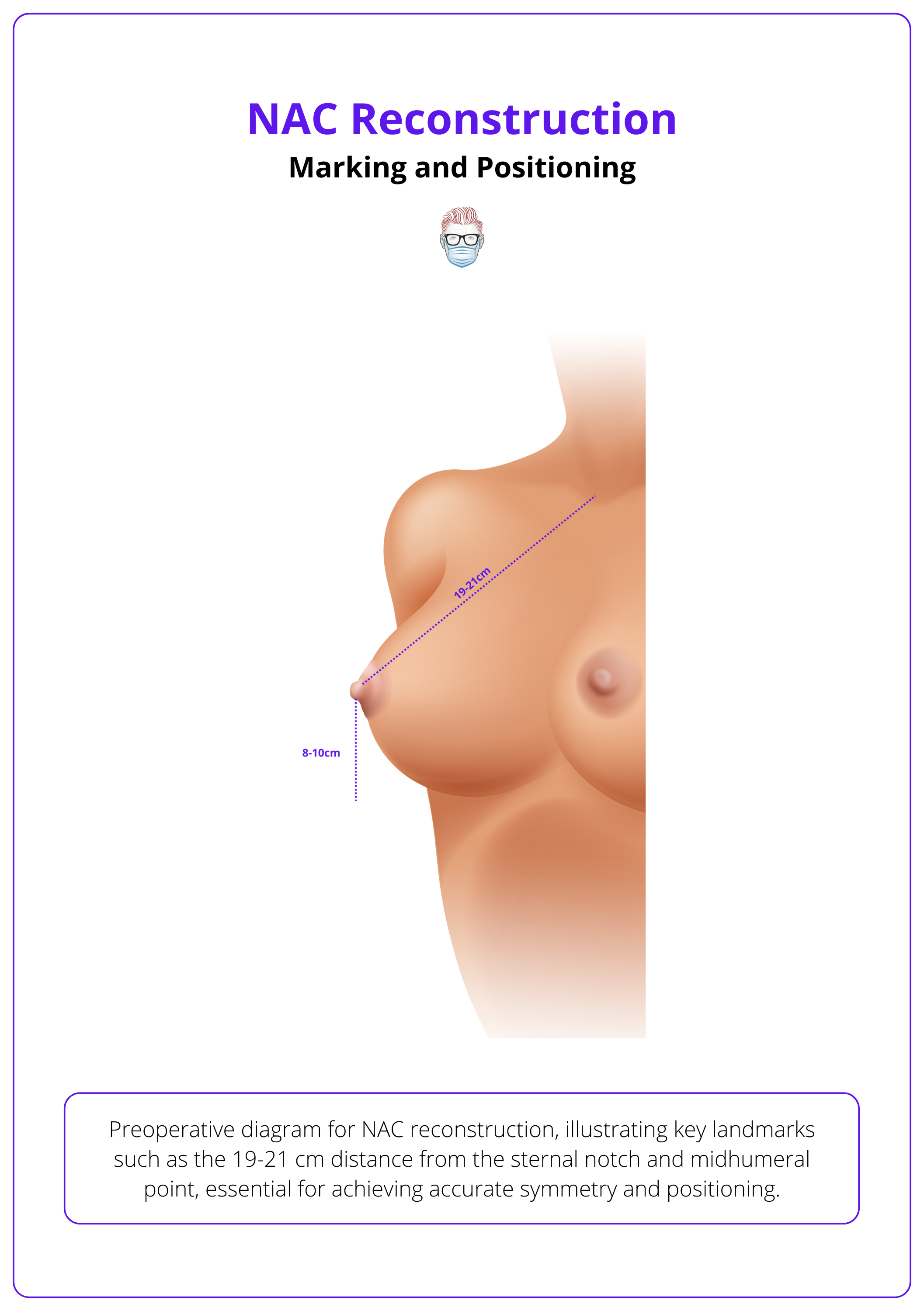
Measure Position
Before designing new nipple-areola complexes, accurately measure the following landmarks:
- Position the patient standing.
- Mark the midline, inframammary fold (IMF), and breast meridian (midclavicular line to nipple).
- Mark the nipple height at the 4th intercostal space, just lateral to the midclavicular line.
- Mark the horizontal location midway between the sternal notch and the lateral border of the breast mound.
Tips for NAC Reconstruction
- Prioritize nipple position over shape.
- Use existing NAC as a reference in unilateral cases.
- Adjust for planned position with contralateral lift.
- Base nipple position on breast shape and size in bilateral cases.
- Confirm placement with the patient in a full-length mirror.
It's easier to lift a low nipple than to lower an excessively high one, which may become visible above the bra cup's upper edge (Paolini et al., 2021).
NAC Reconstruction Techniques
Nipple reconstruction uses flap techniques and augmentation methods, while areolar reconstruction can be done simultaneously or delayed, such as with 3D tattooing.
Nipple-areolar reconstruction involves flap reconstruction, nipple augmentation, and areolar reconstruction.
Flap options include subdermal pedicled, center-based local, and combined subdermal-pedicle with central-core flaps, while augmentation methods include autologous grafting, alloplastic techniques, and allografts.
Flap Reconstruction Techniques
There is no gold standard for NAC reconstruction. Flap options include subdermal pedicled, centre-based local, and combined subdermal-pedicle with central-core flaps.
These techniques are detailed in the table below.
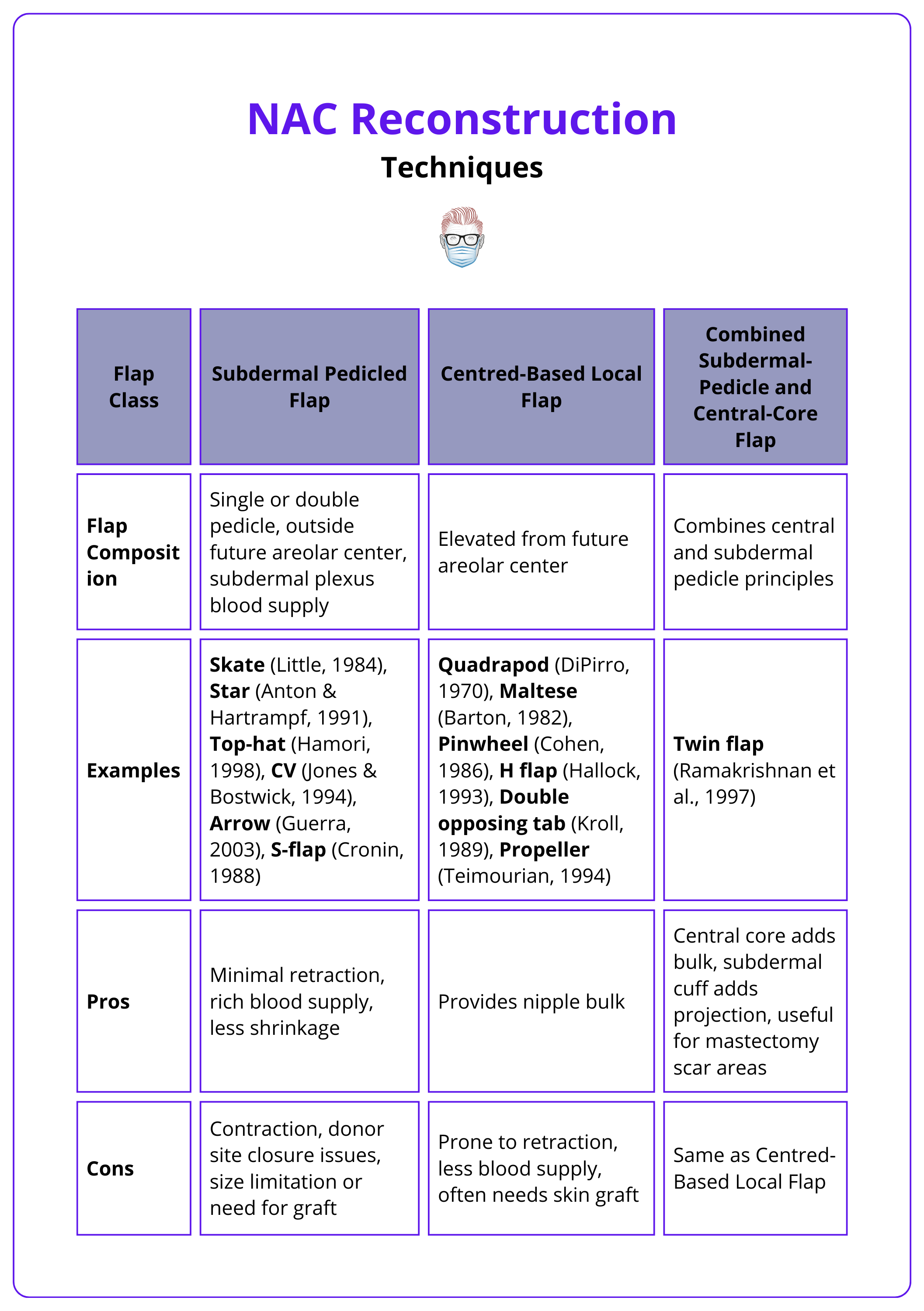
NAC Flap Reconstruction
These NAC flap reconstructions are explained in more detail below.
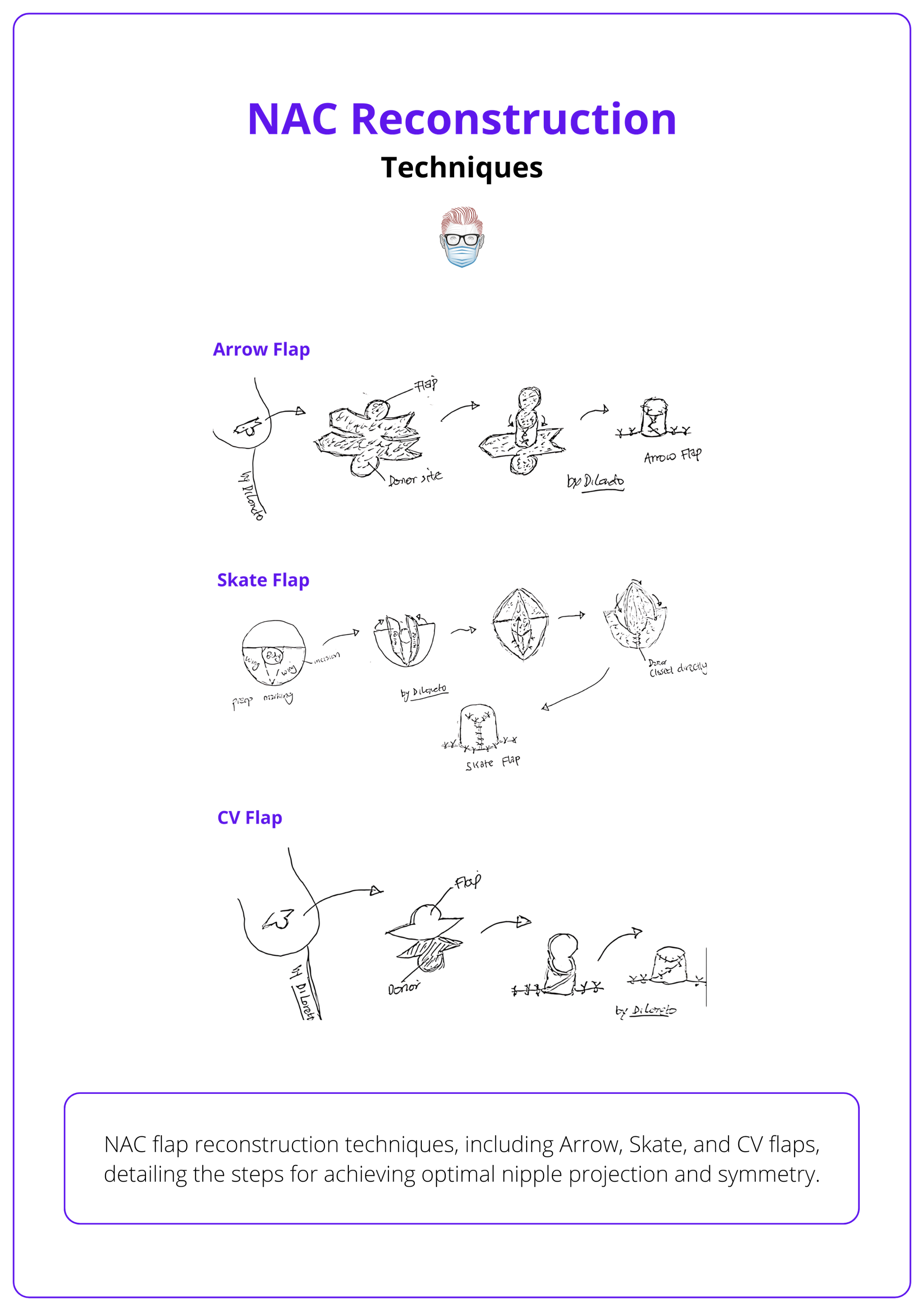
Arrow Flap
- Raising: Subdermal flap raised from lateral ends to base.
- Inset: Opposing ends wrapped together; C-flap forms roof.
- Closure: Primary closure at the donor site.
- Limitation: May lose projection.
Skate Flap
- Raising: Full-thickness wings raised.
- Inset: Adipose tissue column incorporated for projection. Wings wrap around the nipple's central body.
- Closure: Direct closure.
- Benefit: Optimal for providing projection
CV Flap
- Design: Two lateral V-shaped limbs connected by a C-shaped curve.
- Raising: Lateral limbs towards the midline in the subcutaneous plane. Subcutaneous fat may be included to enhance vascularity and volume.
- Inset: Lateral limbs wrapped towards each other, C-flap forms the roof.
- Closure: Direct closure
These flap designs are illustrated in the image below.
Post-operatively, dressing choices vary, often including topical antibiotics or petroleum jelly. Key points include:
- Protective Dressing: Applied with a hole for the neo-nipple, sometimes using a nipple guard, breastfeeding shield, or 10ml syringe base.
- Bra and Compression: Use a non-compressing bra; avoid direct compression for 6-8 weeks, or up to 3 months for significant projection.
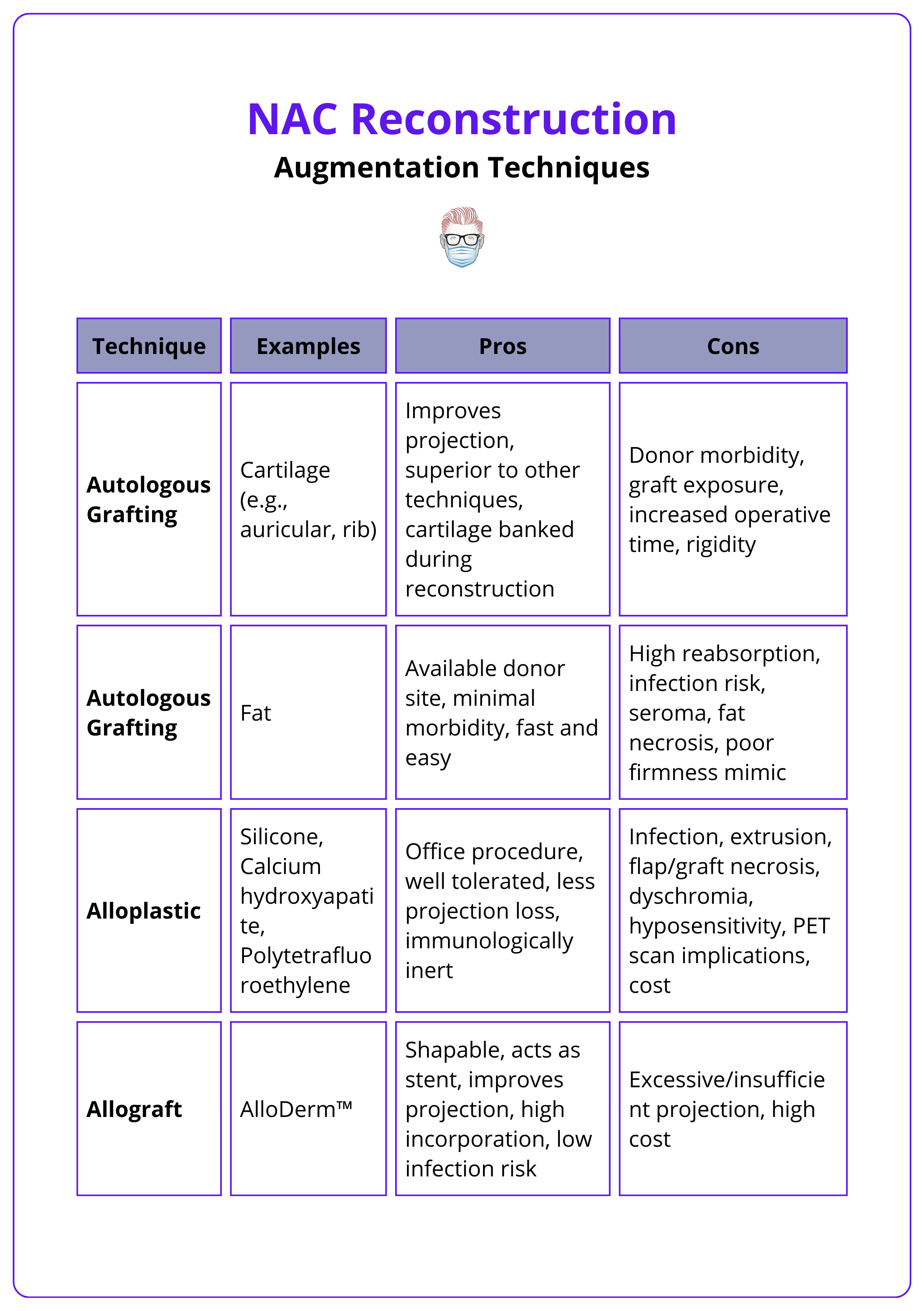
Nipple Augmentation Techniques
Nipple augmentation techniques include autologous grafting, alloplastic methods, and allografts, each with specific advantages and disadvantages. These are detailed in the table below.
Areolar Reconstruction Techniques
Areolar reconstruction uses skin grafting for natural texture or dermal tattooing for a less invasive option, with the purse string suture technique enhancing definition.
Areolar reconstruction can be performed either simultaneously with nipple reconstruction or as a delayed procedure. The two primary methods are skin grafting and dermal tattooing.
Skin Grafting
Skin grafting involves harvesting skin from donor sites such as the contralateral areola, medial thighs, abdominal-inguino-perineal region, or areas with excess skin. This method offers a textured and wrinkled appearance similar to a natural areola and allows for pigment variations. Techniques like pie-crusting can mimic the Montgomery tubercles, enhancing the natural look.
- Advantages of skin grafting include its ability to closely resemble natural areolar texture.
- Disadvantages include the risk of graft failure, contracture, loss of sensation, and donor site morbidity. Long-term color can be unpredictable.
Dermal Tattooing
Dermal tattooing, introduced in the 1970s (Bunchman et al., 1975), is a less invasive option that can be used alone or in conjunction with nipple reconstruction. This technique involves applying pigment to the skin to replicate the appearance of an areola.
- Advantages: quick and straightforward, no hospitalization or general anesthesia, no donor site morbidity, good initial color match
- Disadvantages: lacks texture and projection of natural tissue. The success of this technique heavily depends on the skill of the tattooist.
Purse String Suture Technique
Caterson et al. (2015) used this technique during nipple reconstruction with a C-V flap. Key steps to the procedure are:
- Once the neo-areolar is marked, small incisions (~2mm) are made, 8mm apart and 5mm from the areolar diameter.
- The areolar is then cinched with a purse string suture. This elevates the areolar and reduces radial pull at the base of the nipple.
To avoid areolar tightness and deformity, it is advisable to harvest skin grafts with a diameter slightly larger than the areolar diameter.
Conclusion
1. Basics of NAC Reconstruction: Gained a comprehensive understanding of the various aspects and challenges of NAC reconstruction, including the latest techniques and methodologies.
2. Techniques of NAC Reconstruction: Explored the technical aspects of NAC reconstruction, such as the different flap techniques and the importance of preoperative planning.
3. Clinical Considerations: Explored the clinical considerations of NAC reconstruction, including patient-specific factors and potential contraindications.
4. Complications and Management: Learned about the potential complications associated with NAC reconstruction and the strategies for managing them.
Further Reading
- Farhadi J, Maksvytyte GK, Schaefer DJ, Pierer G, Scheufler O. Reconstruction of the nipple–areola complex: an update. J Plast Reconstr Aesthet Surg. 2006;59:40-5.
- Braza ME, Sisti A. Nipple-Areolar Complex Reconstruction.StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
- Zucca-Matthes G, Urban C, Vallejo A. Anatomy of the nipple and breast ducts. Gland Surg. 2016 Feb;5(1):32-6. doi: 10.3978/j.issn.2227-684X.2015.05.10. PMID: 26855906; PMCID: PMC4716863.
- Mayer AP, Goodreau AM, Blanchet NP. Accurate Nipple Areolar Positioning in Nipple-sparing Mastectomy Reconstruction. Plast Reconstr Surg Glob Open. 2019 Jan 14;7(1):e2064. doi: 10.1097/GOX.0000000000002064. PMID: 30859033; PMCID: PMC6382234.
- Paolini, G., Firmani, G., Briganti, F. et al. Guiding Nipple-Areola Complex Reconstruction: Literature Review and Proposal of a New Decision-Making Algorithm. Aesth Plast Surg 45, 933–945 (2021). https://doi.org/10.1007/s00266-020-02047-9
- Zenn MR, Garofalo JA. Unilateral nipple reconstruction with nipple sharing: time for a second look. Plast Reconstr Surg. 2009 Jun;123(6):1648-53. https://doi.org/10.1097/PRS.0b013e3181a3f2f.
- Millard DR Jr. Nipple and areola reconstruction by split-skin graft from the normal side. Plast Reconstr Surg. 1972 Oct;50(4):350-3. doi: 10.1097/00006534-197210000-00006. PMID: 4561575.
- Little JW. Nipple-areolar reconstruction. In: Spear SL, editor. Surgery of the Breast: Principles and Art. Philadelphia: Lippincott-Raven Publisher; 1998.
- Little III JW. Nipple-areola reconstruction. Clin Plast Surg. 1984;11:351-64.
- Ramakrishnan VV, Mohan D, Villafane O, Krishna A. Twin flap technique for nipple reconstruction. Ann Plast Surg 1997;39: 241–4.
- Sisti A, Grimaldi L, Tassinari J, et al. Nipple-areola complex reconstruction techniques: A literature review. Eur J Surg Oncol. 2016;42:441–465.
- Antón, M.A., Eskenazi, L.B., & Hartrampf, C.R. (1991). Nipple Reconstruction With Local Flaps: Star and Wrap Flaps. Seminars in Plastic Surgery, 5, 67 - 78.
- Hamori, C.A., & Larossa, D. (1998). The Top Hat Flap: For One Stage Reconstruction of a Prominent Nipple (Top Hat Flap). Aesthetic Plastic Surgery, 22, 142-144.
- Jones G, Bostwick 3rd J. Nipple-areolar reconstruction. Operative Tech Plastic Reconstr Surg.1994; 1:35-8.
- Guerra, A. B., Khoobehi, K., Metzinger, S. E., & Allen, R. J. (2003). New technique for nipple areola reconstruction: arrow flap and rib cartilage graft for long-lasting nipple projection. Annals of plastic surgery, 50(1), 31–37. https://doi.org/10.1097/00000637-200301000-00006.
- Cronin, E. D., Humphreys, D. H., & Ruiz-Razura, A. (1988). Nipple reconstruction: the S flap. Plastic and reconstructive surgery, 81(5), 783–787. https://doi.org/10.1097/00006534-198805000-00026.
- DiPirro ME. Reconstruction of the nipple and areolar after burn. Case report. Plast Reconstr Surg 1970;46:299-300.
- Barton Jr FE. Latissimus dermal-epidermal nipple reconstruction. Plast Reconstr Surg 1982;70:234–7.
- Cohen, I. K., Ward, J. A., & Chandrasekhar, B. (1986). The pinwheel flap nipple and barrier areola graft reconstruction. Plastic and reconstructive surgery, 77(6), 995–999. https://doi.org/10.1097/00006534-198606000-00025.
- Hallock, G. G., & Altobelli, J. A. (1993). Cylindrical nipple reconstruction using an H flap. Annals of plastic surgery, 30(1), 23–26. https://doi.org/10.1097/00000637-199301000-00003.
- Kroll SS, Hamilton S. Nipple reconstruction with the double-opposing-tab flap. Plast Reconstr Surg. 1989;84(3):520-5.
- Teimourian, B., & Duda, G. (1994). The propeller flap: a one-stage procedure for nipple-areola reconstruction. Aesthetic plastic surgery, 18(1), 81–84. https://doi.org/10.1007/BF00444253.
- Rees TD. Reconstruction of the breast areola by intradermal tattooing and transfer. Case report. Plast Reconstr Surg1975;55:620-1.
- Spear SL, Convit R, Little JW., 3rd Intradermal tattoo as an adjunct to nipple-areola reconstruction. Plast Reconstr Surg1989;83:907-11.
- Bunchman HH, Larson DL, Huang TT, Lewis SR. Nipple and areola reconstruction in the burned breast. The ‘double bubble’ technique. Plast Reconstr Surg 1974;54:5.
- Caterson, Stephanie A. MD; Singh, Mansher MD; Talbot, Simon G. MD; Eriksson, Elof MD, PhD. Reconstruction of Areolar Projection Using a Purse-String Suture Technique. Plastic and Reconstructive Surgery Global Open 3(7):p e453, July 2015. | DOI: 10.1097/GOX.0000000000000431


