In this week's edition
- ✍️ Letter from P'Fella
Low-volume surgeons are hobbyists? - 🤓 The Sunday Quiz + Leaderboard
Start of a new season: Merkel cell carcinoma - 🎙️ Behind the 'Fella Episode 1
Listen to our first podcast episode! - 🎓 theFellow's Corner
What's new with the team? - 📖 What does the evidence say?
What does the evidence say about burying K-wires? - 🔥 Skin Cancer Articles of the Week
Merkel cell carcinoma, melanoma controversies, & basal cell carcinoma; with 1 sentence summaries. - 💕 Feedback
Suggest ideas & give feedback!
A Letter from P'Fella
Low-Volume Surgeons are Hobbyists?
I've come across the argument that low-volume surgeons are hobbyists, but I disagree, especially in the context of plastic surgery. Let's dive into the details.
👇
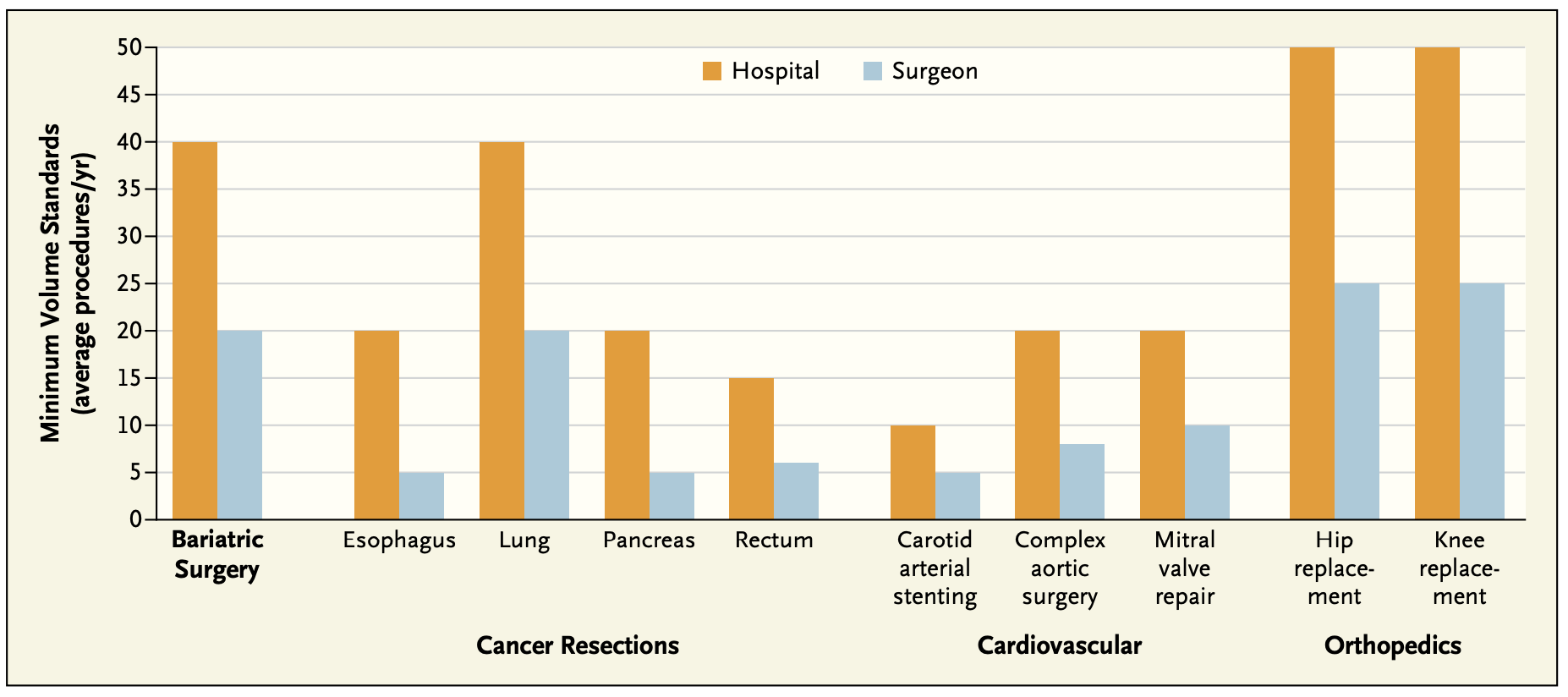
Defining "low volume" is tricky. The "Take the Volume Pledge" campaign sets minimum annual procedure thresholds, like 10 per hospital and 5 per surgeon for carotid stenting, and 50 per hospital and 25 per surgeon for hip and knee replacements. However, these numbers can be arbitrary and not always evidence-based.
But the Evidence is Clear?
Higher-volume surgeons do generally have better outcomes. A systematic review by Chowdhury et al. found that high-volume hospitals had significantly better outcomes in 74% of studies, though the benefit was less pronounced in prospective studies (40%). Similarly, high-volume surgeons had better outcomes in 74% of studies.
A Different Perspective
In plastic surgery, many conditions are inherently low volume, making certain surgeries rare. Procedures like thumb pollicization or Gustilo-Anderson 3C fractures are seldom encountered, even by subspecialists. As plastic surgeons, we handle a wide range of complex cases, similar to general surgeons but without the focus on visceral organs. The "Take the Volume Pledge" doesn't address managing low-volume procedures in these specialties, which are critical for patient care.
Potential Solutions
High standards must be maintained across all types of surgeries, whether common or rare.
- Subspecialize Further: Encourage focused subspecialization to develop deep expertise in specific areas.
- Travel to Other Departments: Gain exposure to rare procedures by collaborating with high-volume centers.
- Centralize Surgeries: Centralize low-volume surgeries in specialized centers to ensure patients receive care from experienced surgeons.
I'm eager to hear your thoughts. What methods should we explore to maintain our low-volume skills? Just reply to this email and share your insights!
P'Fella ❤️
tl;dr
👉 I disagree with the idea that low-volume surgeons are hobbyists, especially in plastic surgery.
👉 Defining low volume is complex and often arbitrary.
👉 Many conditions in plastic surgery are already low volume, making surgeries even rarer.
👉 Let's discuss how to adapt our training to ensure optimal patient care.
The Sunday Quiz
New Season is Starting!
Welcome to the first round of The Weekly Quiz.
Each edition of thePlasticsPaper includes a quiz question designed to challenge and engage our readers. Keep your wits about you and join in every week—the winner at the end of six rounds will earn you a $100 voucher.
PS: Our top scorers from the last season are joining us for a playoff, live on our upcoming podcast episode!
Behind the ‘Fella
Episode One is Now Live!
Have you checked out the first episode of our podcast yet? "Behind the Fella," is now live on Spotify or Apple.
Join us for exclusive insights from our team meetings and engaging discussions on plastic surgery with our fellows. Get a unique, behind-the-scenes look at our practice!
The first episode is out! 🌟
Have a listen to our discussion on:
- Meet the team!
- Seymour fractures
- K-wire tips and tricks
- Surgical video brainstorming debut on the platform
the Fellows' Corner
What have the fellows been up to?
Our team has been hard at work creating fantastic new content for our community, including fresh articles, clinical cases, and surgical techniques focused on tumors. Don't miss our article on Merkel cell carcinomas.
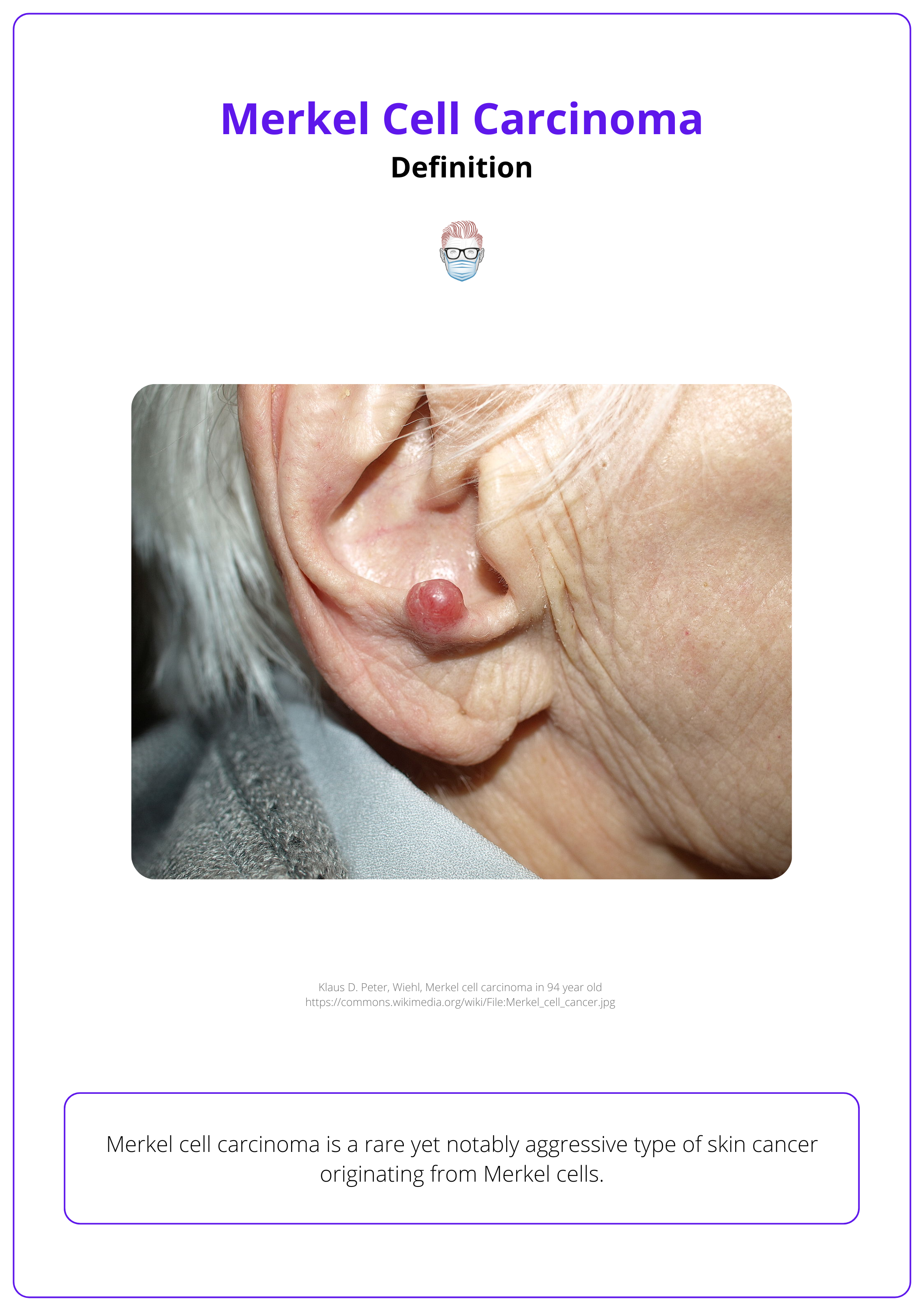
Merkel Cell Carcinoma
Definition
Merkel cell carcinoma is a malignant skin lesion arising from neuroendocrine cells.
Risk Factors
Include sun exposure, older age, immunosuppression, being Caucasian, and being male.
Pathogenesis
Merkel cell polyomavirus (MCPyV) is a recently discovered polyomavirus in MCC tumour tissue.
Clinical Features
A fast-growing, painless, firm, non-tender cutaneous nodule. It is reddish-purple with a shiny surface, most commonly in the head and neck region.
Diagnosis
Definitive diagnosis of MCC consists of histopathology with an immunohistochemistry panel. An SNLB should be performed on all patients who are diagnosed with MCC.
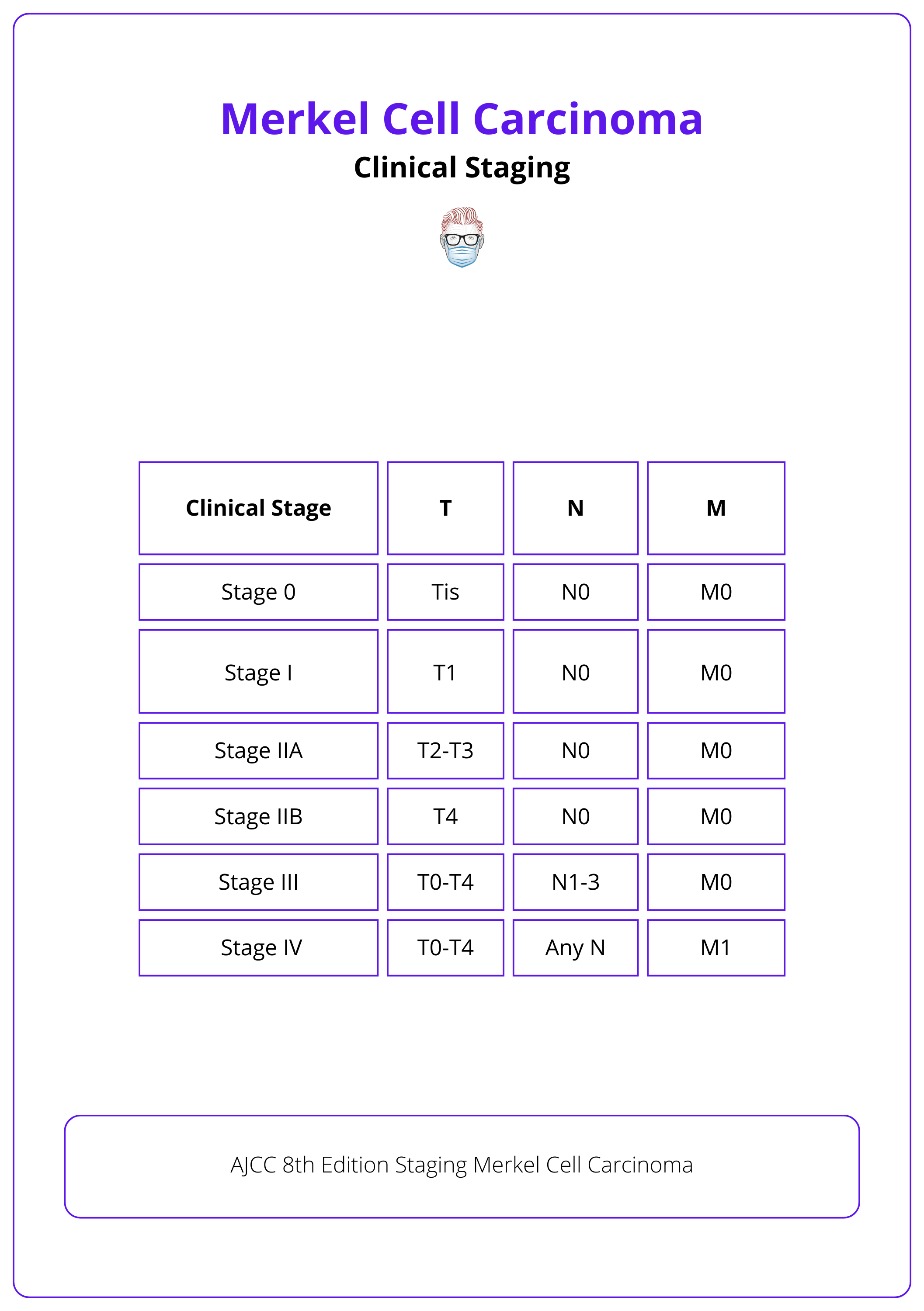
Clinical Staging
MCC is classified and staged from the AJCC 8th edition of 2017.
Treatment
Treatment of MCC involves wide local excision +/- radiotherapy as MCC is very radiosensitive. Chemotherapy is rarely used, except occasionally for palliative care.
On top of that, we've also curated a clinical case of Merkel cell carcinoma – you can read it here.
What does the Evidence say?
A new section!
Buried vs Non-Buried K-Wires in Hand Surgery
"The decision to bury or leave Kirschner wires (K-wires) exposed in hand surgery is influenced by various factors, including ease of removal, perceived risk of infection, and patient preferences (Gardiner 2018). While some studies have found no significant difference in infection rates between buried and non-buried K-wires (Koç 2012), others have reported a lower risk of pin site infection with buried K-wires (Hidajat 2023). However, non-buried K-wires have been associated with a lower risk of adverse events and may be more cost-effective (Wormald 2017). Similarly, percutaneous K-wires have been found to have a significantly greater infection rate than buried wires in treating hand fractures (Rafique 2006)".
Articles of the Week
3 interesting articles with 1 sentence summaries.
The NCCN Guidelines for Merkel Cell Carcinoma highlight the importance of early detection through comprehensive skin exams and biopsy, with immunohistochemistry staining confirming the diagnosis.
Controversies in melanoma treatment: Optimal margins for in situ and invasive disease, reconstructive options like the keystone flap for excision defects, and advancements in managing sentinel node biopsies.
Explore the latest NCCN guidelines on Basal Cell Skin Cancer, detailing diagnostic, treatment, and follow-up practices for this prevalent skin cancer.


