Summary Card
Definition
Lymphoedema is a chronic condition caused by impaired lymphatic drainage, resulting in progressive swelling, primarily affecting the limbs.
Overview of the Lymphatic System
Lymphoedema primarily affects the superficial, epifascial lymphatic system, while the subfascial system remains largely uninvolved.
Types of Lymphoedema
Primary lymphoedema results from congenital or genetic abnormalities, while secondary lymphoedema arises due to external factors such as surgery, radiation, infections, trauma, or malignancy.
Pathophysiology
Lymphoedema involves lymphatic obstruction, inflammation, fibrosis, adipose deposition, and impaired lymphangiogenesis, with non-specific histologic changes such as dermal edema and hyperkeratosis.
Grading
Lymphoedema grading is based on symptoms, reversibility, and the chronicity of the condition.
Clinical Features
Patients with lymphoedema typically present with swelling, heaviness, skin changes, and frequent infections. Diagnosis requires a thorough history and clinical examination.
Management
First-line treatment for lymphoedema is complete decongestive therapy (CDT), with surgery reserved for severe, debilitating cases or specific patient groups.
Primary Contributor: Dr Kurt Lee Chircop, Educational Fellow.
Reviewer: Dr Waruguru Wanjau, Educational Fellow.
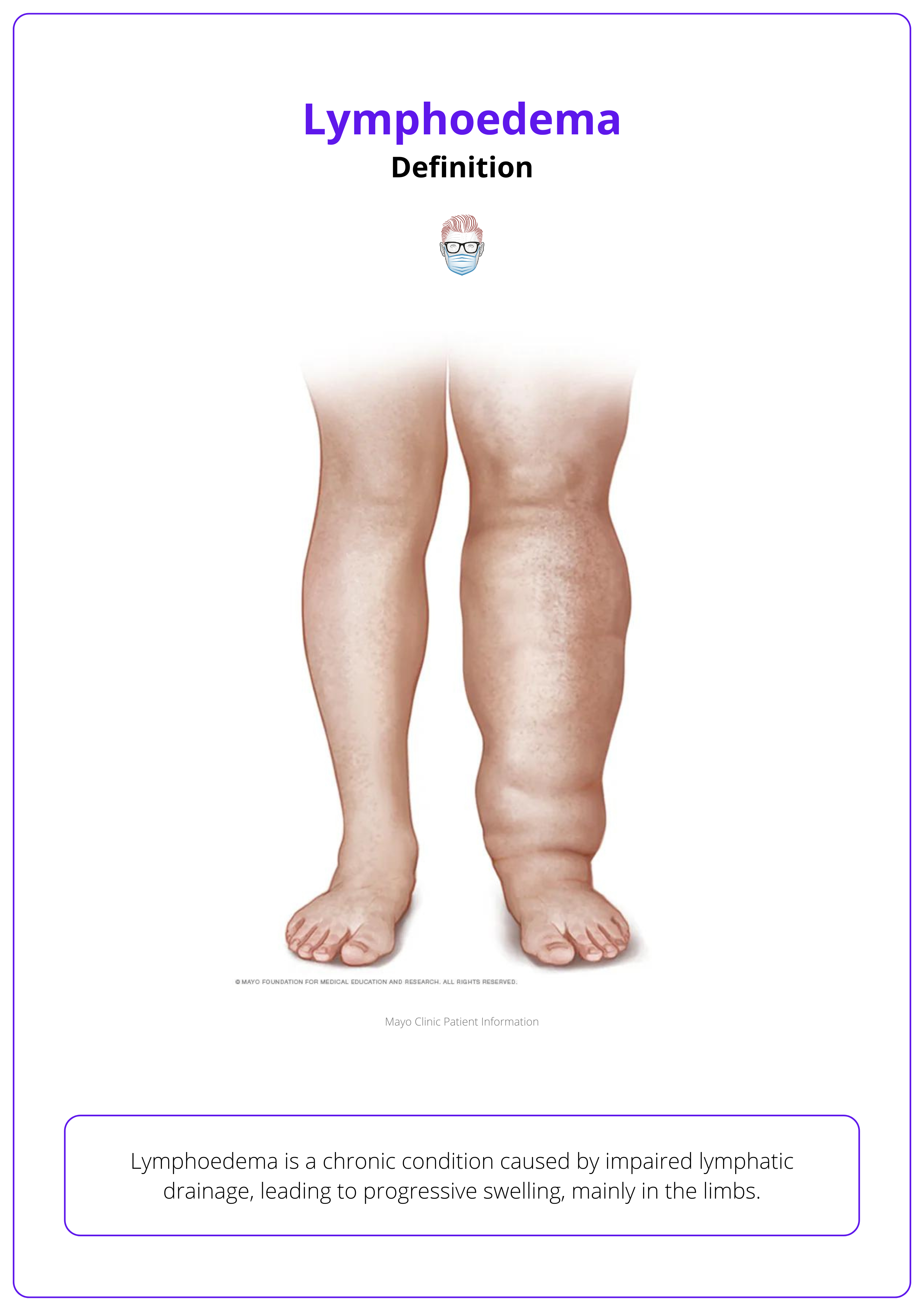
Definition of Lymphoedema
Lymphoedema is a chronic condition caused by impaired lymphatic drainage, resulting in progressive swelling, primarily affecting the limbs.
Lymphoedema is characterized by protein-rich fluid accumulation in tissues, leading to swelling and tissue changes over time.
Lymphoedema arises from the abnormal buildup of protein-rich fluid in the interstitial space due to impaired lymphatic drainage. This blockage increases protein levels in the tissues, causing water retention and soft tissue swelling. The elevated protein content promotes fibroblast activity, which contributes to fluid organization and the development of non-pitting swelling in the affected areas. This chronic process leads to progressive limb enlargement, as seen in the image below.
Elephantiasis Nostra Verrucosa (ENV) is a rare skin condition from chronic lymphoedema, marked by thick, hardened, wart-like skin (Fredman, 2012).
Overview of the Lymphatic System
Lymphoedema primarily affects the superficial, epifascial lymphatic system, while the subfascial system remains largely uninvolved.
Normal Lymphatic System
Normal Anatomy
- Lymphatic Capillaries: Blind-ended capillaries begin in the dermal papillae's interstitial spaces. These unvalved capillaries drain into interconnected subdermal channels.
- Epifascial System: Running parallel to the superficial venous system, this system consists of valved trunks with smooth muscle cells located above the deep fascia. It drains lymph from the skin and subcutaneous tissues.
- Subfascial System: Parallels the deep venous system and drains lymph from deeper structures like muscles, joints, periosteum, and bones. Although it operates independently from the epifascial system, the two systems connect in regions such as the popliteal, inguinal, antecubital, and axillary areas (Null, 2023).
Normal Flow
Lymph flow is facilitated by variations in tissue pressure, driven by:
- Skeletal muscle contractions
- Pulsatile blood flow
- Smooth muscle contractions around larger lymphatic channels
Abnormal Lymphatic System
- Lymphoedema primarily affects the epifascial system.
- The subfascial system usually remains uninvolved.
- Reverse flow through perforators decompresses the epifascial system.
- Surgical interventions are focused on addressing the epifascial system.
Types of Lymphoedema
Primary lymphoedema results from congenital or genetic abnormalities, while secondary lymphoedema arises due to external factors such as surgery, radiation, infections, trauma, or malignancy.
Lymphoedema is classified as either primary or secondary, depending on the underlying cause.
Primary Lymphoedema
Primary lymphoedema is a chronic condition caused by congenital or genetic abnormalities that affect lymphatic system development. It can be divided into three main types:
- Congenital (Milroy Disease): Accounts for 10% of primary lymphoedema. It is present at birth and often associated with mutations in the FLT4 gene, affecting lymphatic development.
- Lymphoedema Praecox (Meige Disease): Typically develops between puberty and age 35, most commonly in women.
- Lymphoedema Tarda: Occurs after the age of 35. Its cause is often unknown, but it is linked to hormonal changes or obesity in many cases (Warren, 2007).
Primary lymphoedema is more common in females. Advances in molecular genetics have identified nine causal mutations, highlighting the need for a phenotype-based classification system in the future. An example of bilateral primary lymphoedema is shown in the image below.

Secondary Lymphoedema
Secondary lymphoedema is a chronic condition that develops when the lymphatic system is damaged or obstructed by external factors.
The most common secondary cause is iatrogenic - in particular oncological lymph node surgery. More specifically:
- After breast cancer surgery, occurs in ~5% of cases after sentinel lymph node biopsy, ~20% after axillary lymphadenectomy, and up to 40% with combined axillary lymphadenectomy and radiation (Petronic-Rosic, 2022)
- After gynecological cancer surgery, occurs in 37% of cases likely due to lymph node dissection, chemotherapy, and radiotherapy (Hayes, 2017).
Other causes to consider include:
- Infections: Filariasis (caused by Wuchereria bancrofti) and tuberculosis
- Trauma: Damage to lymphatic vessels
- Malignancy: Obstruction of lymphatic drainage pathways
Globally, filariasis is the leading cause of lymphoedema, while in high-income countries, it’s mostly iatrogenic from oncological treatments and interventions.
Pathophysiology of Lymphoedema
Lymphoedema involves lymphatic obstruction, inflammation, fibrosis, adipose deposition, and impaired lymphangiogenesis, with non-specific histologic changes such as dermal edema and hyperkeratosis.
Lymphoedema results from a combination of mechanisms that lead to tissue changes over time:
- Lymphatic Obstruction: The initial blockage of lymphatic vessels leads to the accumulation of protein-rich interstitial fluid, causing swelling in the affected area (Brown, 2023).
- Inflammation and Fibrosis: Inflammatory cytokines, such as TNF-α and IL-6, accumulate, leading to chronic inflammation. Macrophages infiltrate the tissues, resulting in increased deposition of collagen and extracellular matrix, which ultimately leads to fibrosis.
- Adipose Tissue Deposition: Increased adipogenesis occurs in the affected limb, contributing to both limb enlargement and tissue stiffness.
- Impaired Lymphangiogenesis: The formation of new lymphatic vessels is disrupted, worsening lymphatic stasis. Over time, the lymphatic vessels themselves become sclerotic and lose functionality (Grada, 2017).
Histologic Findings
Although there is no pathognomonic histologic feature of lymphoedema, the following non-specific changes are often observed:
- Dermal edema (more pronounced in earlier stages)
- Hyperkeratosis
- Epidermal papillomatosis and hyperplasia
- Telangiectasia with thickened-walled dermal vessels
- Thickened upper dermis with fibrillar collagen and increased fibroblast numbers (Sleigh, 2019)
Stewart-Treves syndrome is a rare complication of chronic lymphoedema, leading to lymphangiosarcoma. While often linked to post-mastectomy lymphoedema, it can arise from any chronic lymphoedema (Murgia, 2023).
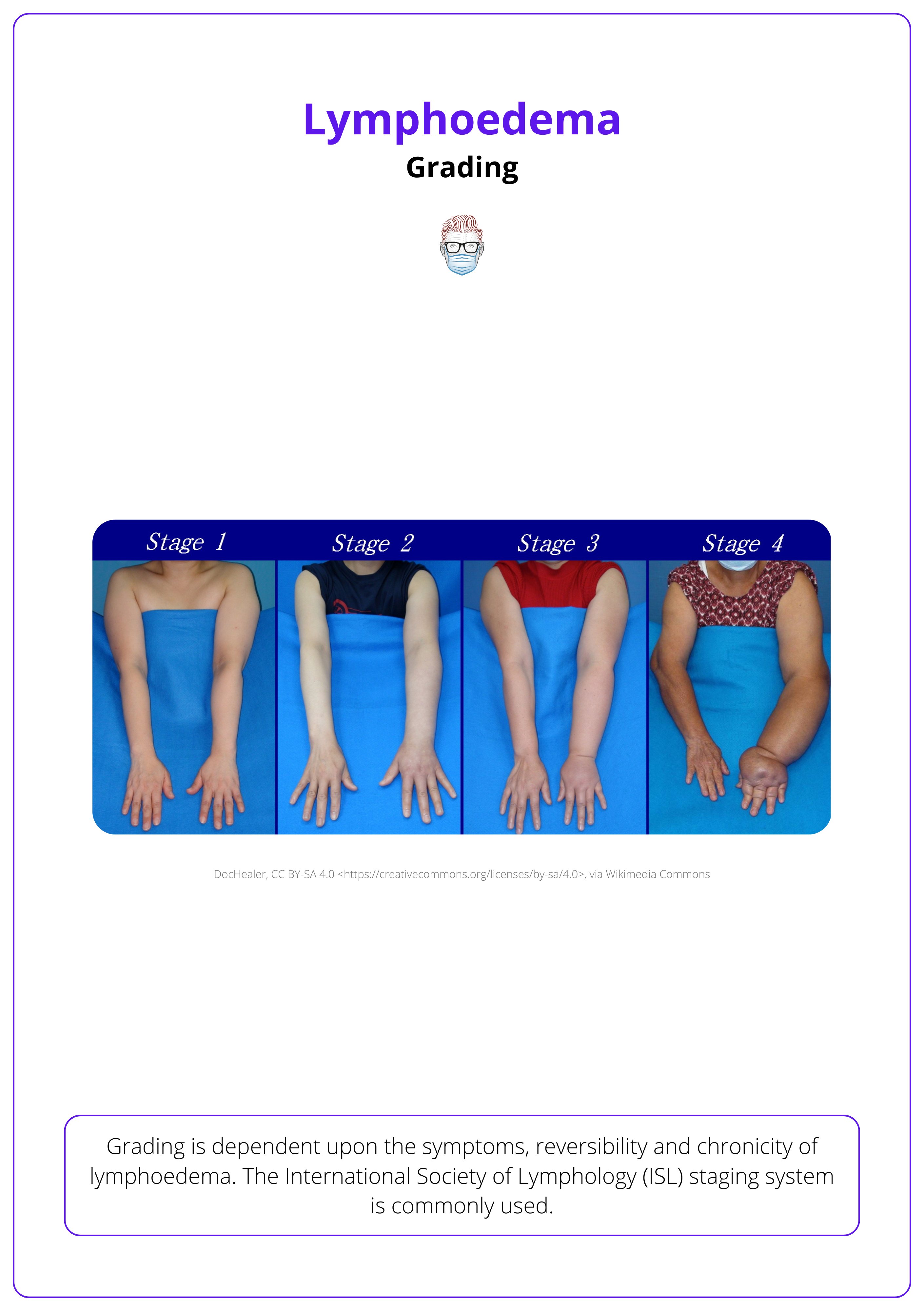
Grading of Lymphoedema
Lymphoedema grading is based on symptoms, reversibility, and the chronicity of the condition as per the International Society of Lymphology (ISL) staging system.
Lymphoedema is a progressive condition, and its severity is classified by the International Society of Lymphology (ISL) staging system (ISL, 2023):
- Stage 0 (Latency): Subclinical stage where lymphatic drainage is impaired, but limb size appears normal. Patients may experience a sensation of heaviness or tightness without visible swelling.
- Stage I (Pitting Edema): Characterized by reversible swelling that improves with limb elevation. The accumulated fluid is protein-rich, promoting inflammation and activation of fibroblasts, but the swelling remains soft and pitting.
- Stage II (Non-Pitting Edema): Swelling becomes permanent and non-pitting due to the development of fibrosis. The affected tissues harden as collagen is deposited and adipose tissue proliferates, making the condition irreversible without intervention.
- Stage III (Lymphostatic Elephantiasis): The most severe form of lymphoedema, characterized by significant swelling, fibrosis, hyperkeratosis, papillomatosis, and wart-like skin changes. Chronic inflammation leads to sclerosis of lymphatic vessels, causing severe functional impairment and deformity.
The stages represent a continuum of worsening severity, as illustrated in the image below.
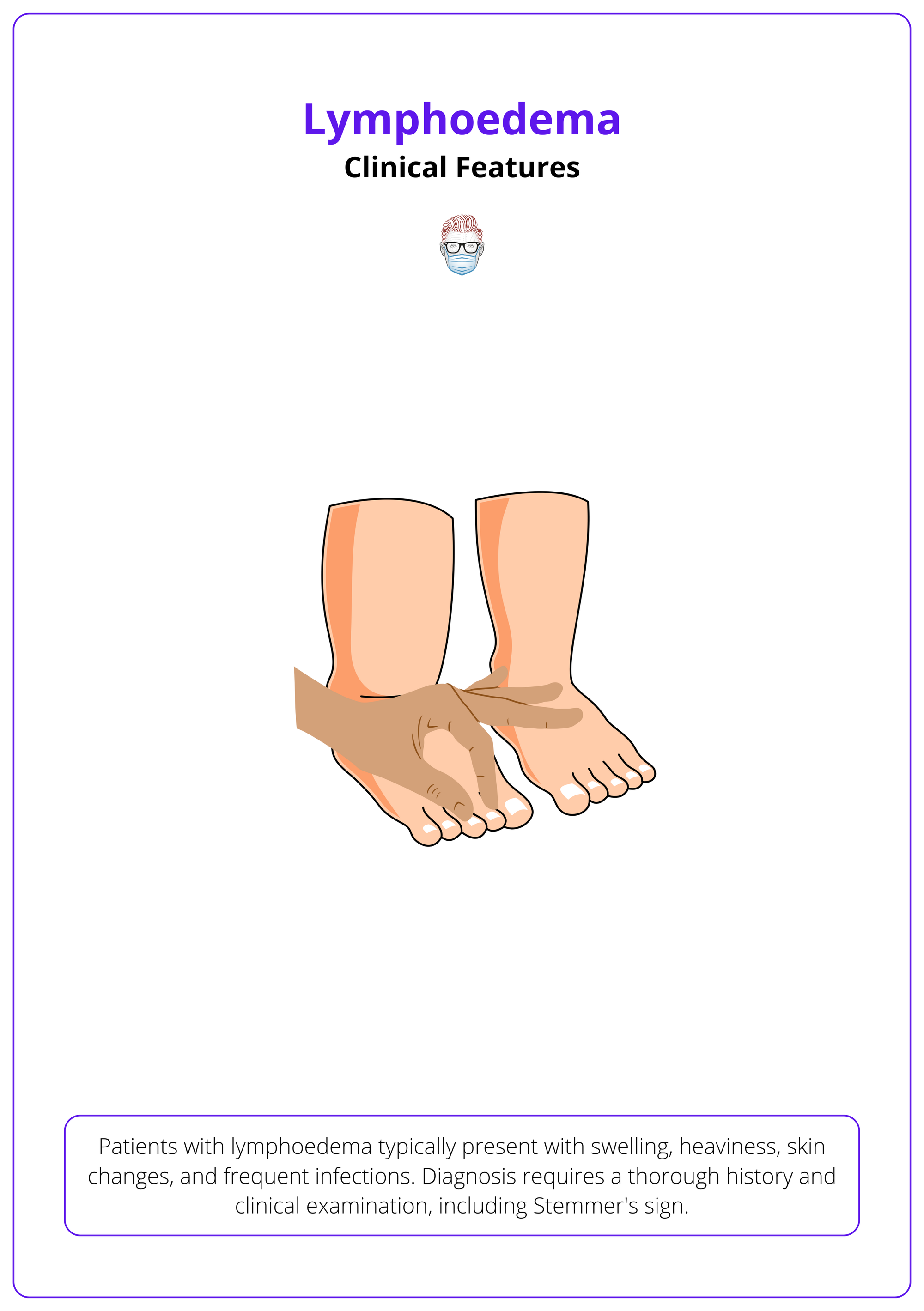
Clinical Features of Lymphoedema
Patients with lymphoedema typically present with swelling, heaviness, skin changes, and frequent infections. Diagnosis requires a thorough history and clinical examination, including circumferential limb measurements.
History
A detailed history is crucial. For suspected primary lymphoedema, family history is key. Other potential causes, such as cancer, surgery, injuries, and severe burns, should also be ruled out.
A typical presentation of lymphoedema is:
- Swelling: Gradual onset, often unilateral but can be bilateral, especially in congenital lymphoedema.
- Heaviness and Aching: Affected limbs often feel heavy and achy.
- Frequent Infections: The compromised immune response in the affected area makes infections more likely.
Several syndromes are associated with lymphoedema, including:
- Turner Syndrome: Features short stature, webbed neck, and lymphoedema.
- Noonan Syndrome: Involves short stature, congenital heart defects, and lymphoedema.
- Klippel-Trenaunay Syndrome: port-wine stain, varicose veins, lymphoedema.
- Yellow Nail Syndrome: Involves lymphoedema, yellow, thickened nails, and respiratory abnormalities.
Clinical Examination
On clinical examination, the following should be noted:
- Inspection: dry, thickened skin, hyperkeratosis, lymphangiomas (lymph fluid-filled blisters), and papillomatosis, which can cause a cobblestone-like appearance, darkened skin, lymphorrhea.
- Palpation: increased warmth, a positive Stemmer's sign.
Circumferential limb measurements using fixed anatomical landmarks:
- ≥2 cm increase or 10% increase in diagnoses of lymphoedema (Houwen, 2022).
- Mild to Moderate: Less than a 20% difference in the affected limb.
- Severe: More than a 20% difference.

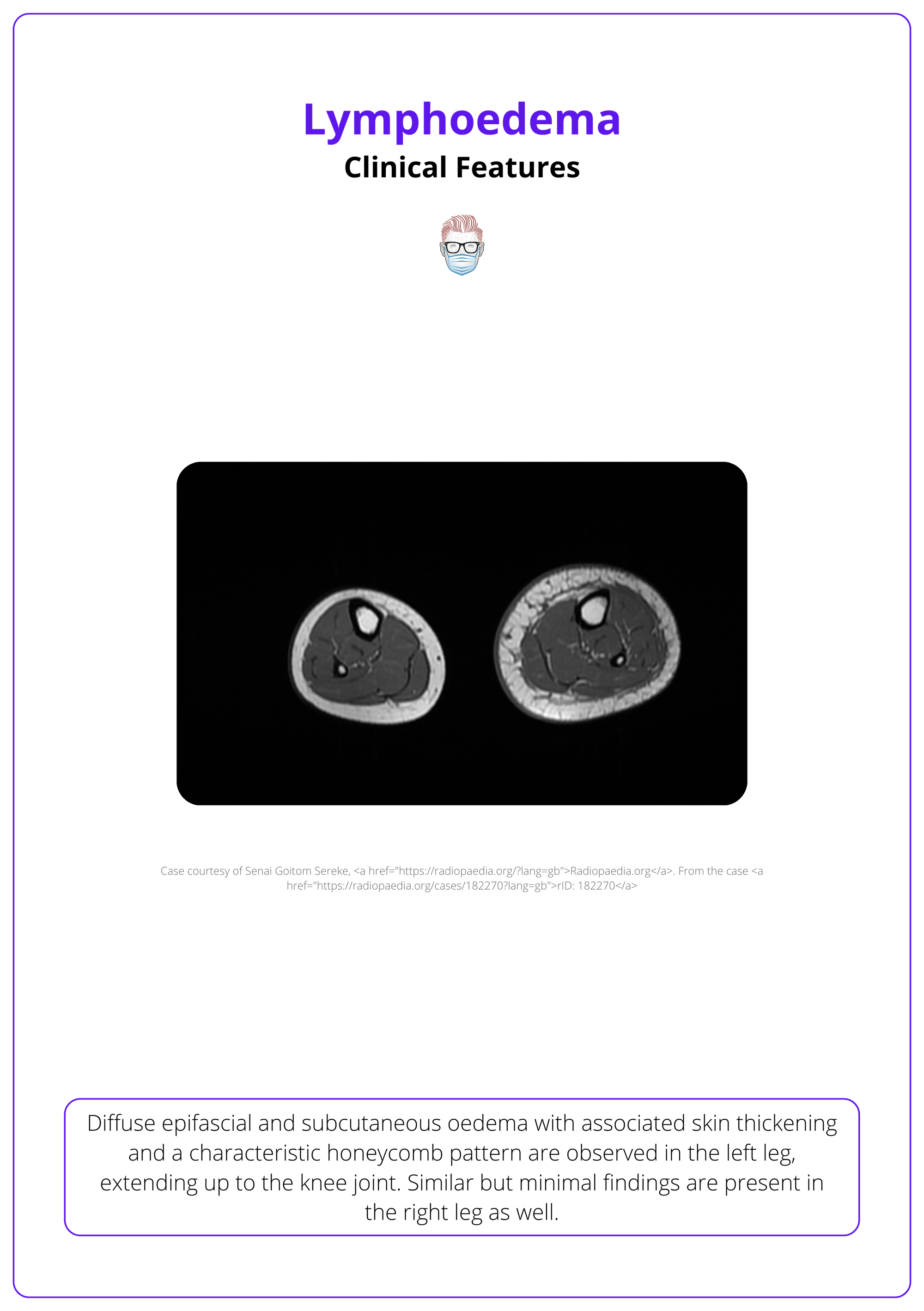
Investigations
- Lymphoscintigraphy: The gold standard for assessing the lymphatic system. It measures radiolabeled Technetium-99m colloid uptake, helping define lymphatic anatomy and evaluate flow dynamics without causing tissue damage.
- ICG Lymphangiography: Offers real-time visualization of lymphatic flow patterns. It is invasive and mainly used intraoperatively due to its potential to worsen the disease.
MRI can be used in certain circumstances as illustrated below.
Other diagnostic tools include bioimpedance spectroscopy, perometry, & skin tonometry.
A positive Stemmer's sign refers to the inability to pinch a fold of skin at the base of the second toe or middle finger — a hallmark of lymphoedema (Goss, 2019).
Management of Lymphoedema
First-line treatment for lymphoedema is complete decongestive therapy (CDT), with surgery reserved for severe, debilitating cases or specific patient groups.
Non-Surgical Management
Non-surgical treatment is the cornerstone of lymphoedema management, aiming to prevent disease progression and alleviate symptoms.
Complete Decongestive Therapy (CDT):
- Phase I (Reduction): Intensive treatment with a lymphoedema specialist, including manual lymphatic drainage, compression therapy, skin care, and physiotherapy.
- Phase II (Maintenance): Focuses on patient self-care, including skin care, use of compression garments, self-lymph drainage, and physical exercise.
- Effectiveness: Although time-consuming and requiring patient commitment, CDT remains the most effective management strategy for lymphoedema (Lasinski, 2013).
Pharmacological Agents:
Some agents, such as benzopyrones and retinoids, may be used alongside conservative treatments, but they come with potential complications due to toxicity.
Surgical Treatment
Surgical interventions are considered for late-stage lymphoedema or when conservative measures fail to control the condition.
Direct Excision (e.g., Charles Procedure):
Involves excising excess adipose tissue and requires lifelong post-operative compression therapy. It carries risks, such as infection and poor cosmetic outcomes, and is reserved for severe cases.
Liposuction:
Targets excess adipose tissue and reduces limb volume.
Vascularized Lymph Node Transfer (VLNT):
Involves transferring lymph nodes from one area (e.g., groin, submental region) to the affected region to restore lymphatic function. Minimally invasive super microsurgical techniques have shown symptom improvement and limb volume reduction in many cases.
Lymphovenous Anastomosis (LVA):
A microsurgical technique that creates a bypass between lymphatic vessels and venules, restoring lymph flow. It is most effective in early-stage cases with functional lymphatic channels.
Outcomes
Both LVA and VLNT have shown promising results in reducing limb volume and improving symptoms, though further research is needed to standardize protocols (Carl, 2017).
Patient-reported tools assess the impact of lymphoedema on quality of life. The most widely used are:
- LYMQOL: A 21-question tool for upper and lower limb lymphoedema.
- ULL-27: A validated tool for breast cancer-related lymphoedema.
Conclusion
1. Definition: Lymphoedema is a chronic condition characterized by the accumulation of protein-rich fluid due to impaired lymphatic drainage, leading to swelling, primarily in the limbs.
2. Lymphatic Anatomy: It primarily affects the superficial epifascial lymphatic system, which consists of networks running parallel to the superficial venous system.
3. Types of Lymphoedema: There are two main types. Primary lymphoedema is caused by congenital or genetic abnormalities. Secondary Lymphoedema results from external damage to the lymphatic system.
4. Pathology: The condition involves lymphatic obstruction and inflammation, leading to fibrosis and adipose deposition, which impair lymphangiogenesis and exacerbate fluid accumulation.
5. Clinical Features and Diagnosis: Symptoms include limb swelling, heaviness, and skin changes like thickening and hyperpigmentation. Diagnosis is primarily clinical, supported by imaging.
6. Management: The primary treatment is complete decongestive therapy, which includes manual lymphatic drainage, compression therapy, and exercise. Severe cases may require surgical interventions.
Further Reading
- Null, Manda, and Manuj Agarwal. "Anatomy, lymphatic system." (2018).
- Keeley, Vaughan, et al. "A quality of life measure for limb lymphoedema (LYMQOL)." Journal of Lymphoedema 5.1 (2010): 26-37.
- Warren AG, Brorson H, Borud LJ, Slavin SA. Lymphedema: a comprehensive review. Ann Plast Surg. 2007 Oct;59(4):464-72. doi: 10.1097/01.sap.0000257149.42922.7e. PMID: 17901744.
- Petronic-Rosic V. Treatment of Skin Disease: Comprehensive Therapeutic Strategies. Skinmed. 2022 Oct 31;20(5):400. PMID: 36314715.
- Hayes, S. C., Janda, M., Ward, L. C., Reul-Hirche, H., Steele, M. L., Carter, J., Quinn, M., Cornish, B., & Obermair, A. (2017). Lymphedema following gynecological cancer: Results from a prospective, longitudinal cohort study on prevalence, incidence and risk factors. Gynecologic oncology, 146(3), 623–629. https://doi.org/10.1016/j.ygyno.2017.06.004
- Brown S, Campbell AC, Kuonqui K, Sarker A, Park HJ, Shin J, Kataru RP, Coriddi M, Dayan JH, Mehrara BJ. The Future of Lymphedema: Potential Therapeutic Targets for Treatment. Curr Breast Cancer Rep. 2023 Jun 1:1-9. doi: 10.1007/s12609-023-00491-5. Epub ahead of print. PMID: 37359311; PMCID: PMC10233555.
- Grada AA, Phillips TJ. Lymphedema: Pathophysiology and clinical manifestations. J Am Acad Dermatol. 2017 Dec;77(6):1009-1020. doi: 10.1016/j.jaad.2017.03.022. PMID: 29132848.
- Sleigh, Bryan C., and Biagio Manna. "Lymphedema." (2019).
- Murgia RD, Gross GP. Stewart-Treves Syndrome. 2023 Aug 14. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 29939610.
- Executive Committee of the International Society of Lymphology. The Diagnosis and Treatment of Peripheral Lymphedema: 2023 Consensus Document of The International Society of Lymphology. Lymphology. 2023;56(4):133-151. PMID: 39207406.
- Houwen, Frans, et al. "Estimates for assessment of lymphedema: Reliability and validity of extremity measurements." Lymphatic Research and Biology 20.1 (2022): 48-52.
- Goss JA, Greene AK. Sensitivity and Specificity of the Stemmer Sign for Lymphedema: A Clinical Lymphoscintigraphic Study. Plast Reconstr Surg Glob Open. 2019 Jun 25;7(6):e2295. doi: 10.1097/GOX.0000000000002295. PMID: 31624689; PMCID: PMC6635205.
- Fredman R, Tenenhaus M. Elephantiasis nostras verrucosa. Eplasty. 2012;12:ic14. Epub 2012 Oct 12. PMID: 23150746; PMCID: PMC3479949.
- Lasinski, Bonnie B. "Complete decongestive therapy for treatment of lymphedema." Seminars in oncology nursing. Vol. 29. No. 1. WB Saunders, 2013.
- Carl, H. M., Walia, G., Bello, R., Clarke-Pearson, E., Hassanein, A. H., Cho, B., ... & Sacks, J. M. (2017). Systematic review of the surgical treatment of extremity lymphedema. Journal of reconstructive microsurgery, 33(06), 412-425.


