In this Article
1. Eyelid Reconstruction focuses on the depth, size, & location of the defect.
2. Direct Closure is an option in low tension wounds
3. Skin is reconstructed by local flaps or full-thickness skin grafts
4. Tarsal plate is reconstructed by cartilage grafts or ADM
5. Conjunctiva is reconstructed by conjunctival flaps or mucosal grafts.
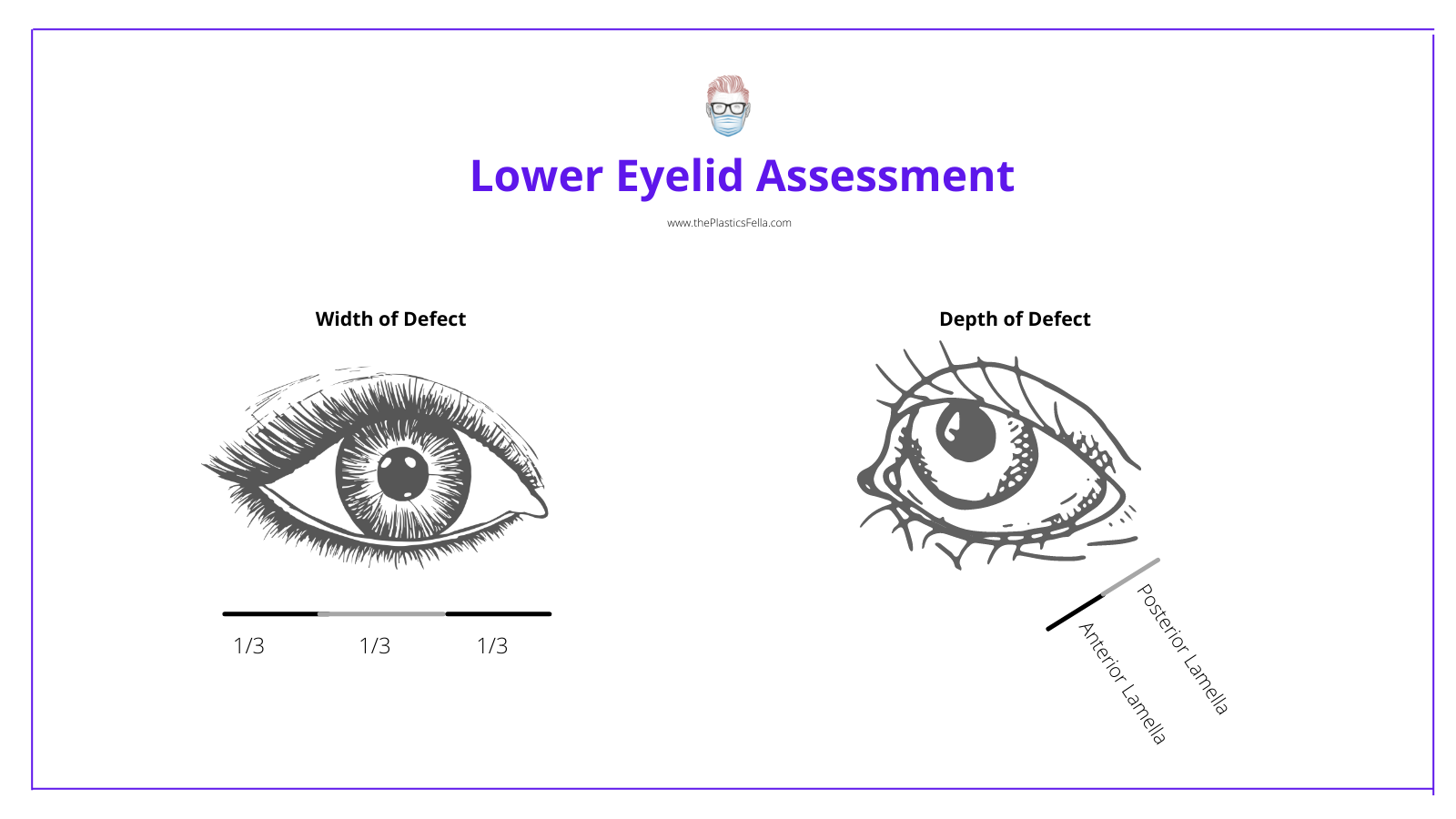
Lower Eyelid Defect Assessment
A lower eyelid defect should be assessed as a 3-Dimensional structure. The following should be noted:
- Location: medial, central or lateral ± canthus involvement.
- Size: 1/3, >1/3.
- Depth: skin, orbicularis, tarsus, conjunctiva or full-thickness
- Patient: skin laxity and quality
- Additional: lacrimal drainage system, contralateral eyelid evaluation
After the assessment, you should know what is "missing" to allow you to replace "like with like".
Lower Eyelid Reconstruction Options
There are 5 ways to reconstruct a lower eyelid: direct closure, graft, flap, secondary intention, or a combination. The decision depends on the depth, location, defect size, and patient factors.
There are 5 ways to reconstruct a lower eyelid: direct closure, graft, flap, or a combination. Each of these options has a further subset of options.
- Direct Closure
- Graft: skin, mucosa (buccal, nasal, palatal), cartilage, acellular dermal matrix.
- Flap: local or regional flaps; cutaneous, myocutaneous or tarsoconjunctival
- Combination of grafts and flaps
- Secondary intention for partial thickness defects ("laissez-faire")
These lower eyelid reconstructive options are visualised in the illustration below.
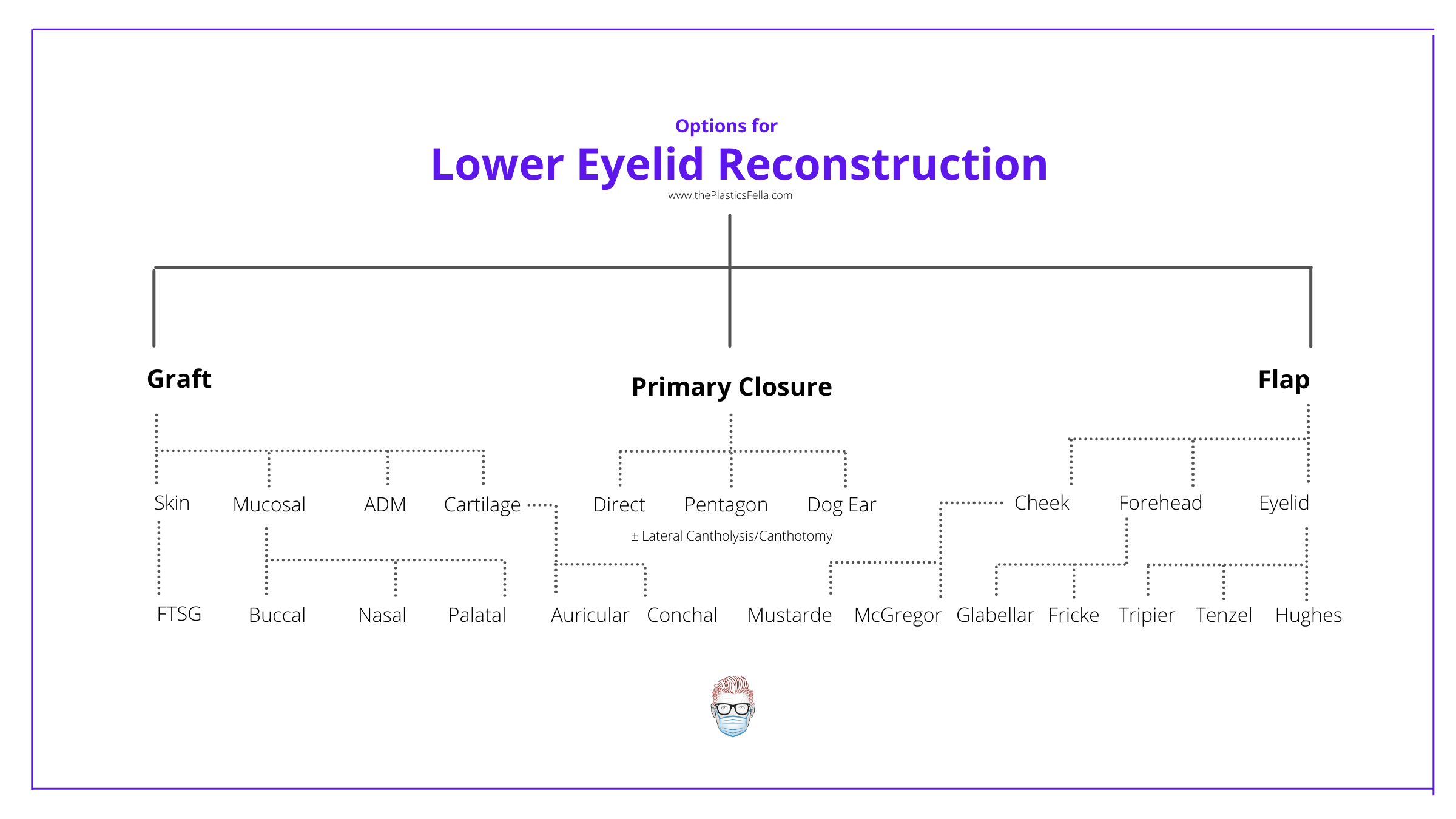
These options may be combined or used with other techniques, such as lateral canthotomy/cantholysis and canthal anchoring.
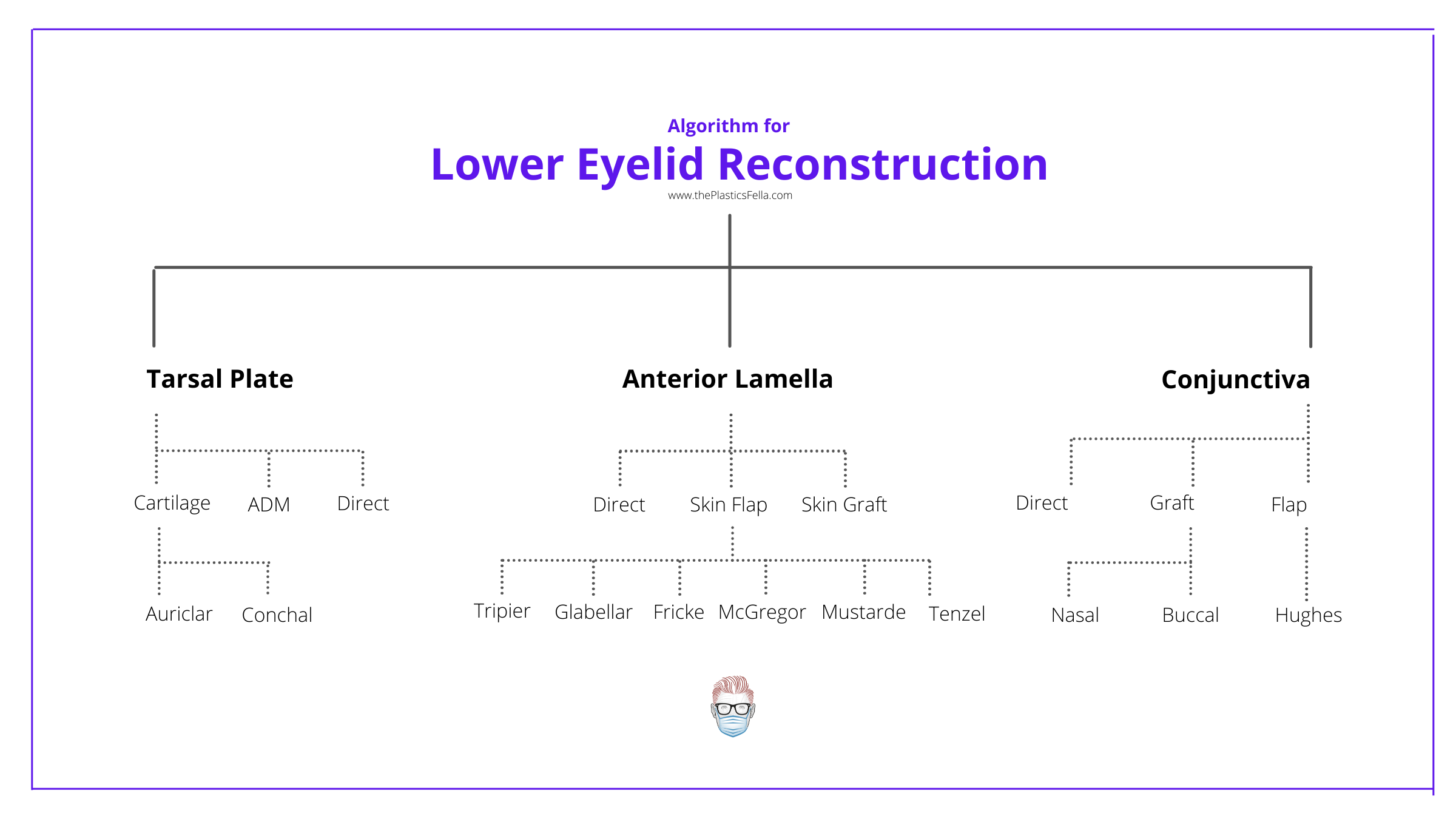
Lower Eyelid Reconstructive Algorithm
Once you are aware of the reconstructive options, it's important to have an understanding of when to use them. The key indicator is if the defect is partial or full thickness.
- Skin: primary tension-free closure, graft, flap, secondary intention
- Conjunctiva: direct closure, advancement flap (preferred), graft
- Tarsus: direct closure, graft, acellular dermal matrix.
- Full-thickness: direct closure, flap, a combination of flap + graft.
The lower eyelid reconstruction algorithm is visualized below in the flow chart.
It is worth noting that healing by secondary intention is an option. It is described as "Laissez faire" - healing by secondary intention/granulation formation. Fox and Beard were the first to describe it. It is feasible in:
- small defects of the anterior lamella
- suited for the medial canthal region (nasal bones resist scar contracture)
- less suited for the middle region due to the risk of cicatricial ectropion.
- Simple absorbant dressing for 48 hours followed by eye drops for several weeks.
Direct Closure of Lower Eyelid
Direct closure of a lower eyelid defect is a suitable option if it can be achieved with minimal tension. It can be performed for both partial and full-thickness defects.
Traditionally, the following ratios have been suggested:
- < 1/3 horizontal width in a standard patient
- <2/3 horizontal width in patients with good skin laxity.
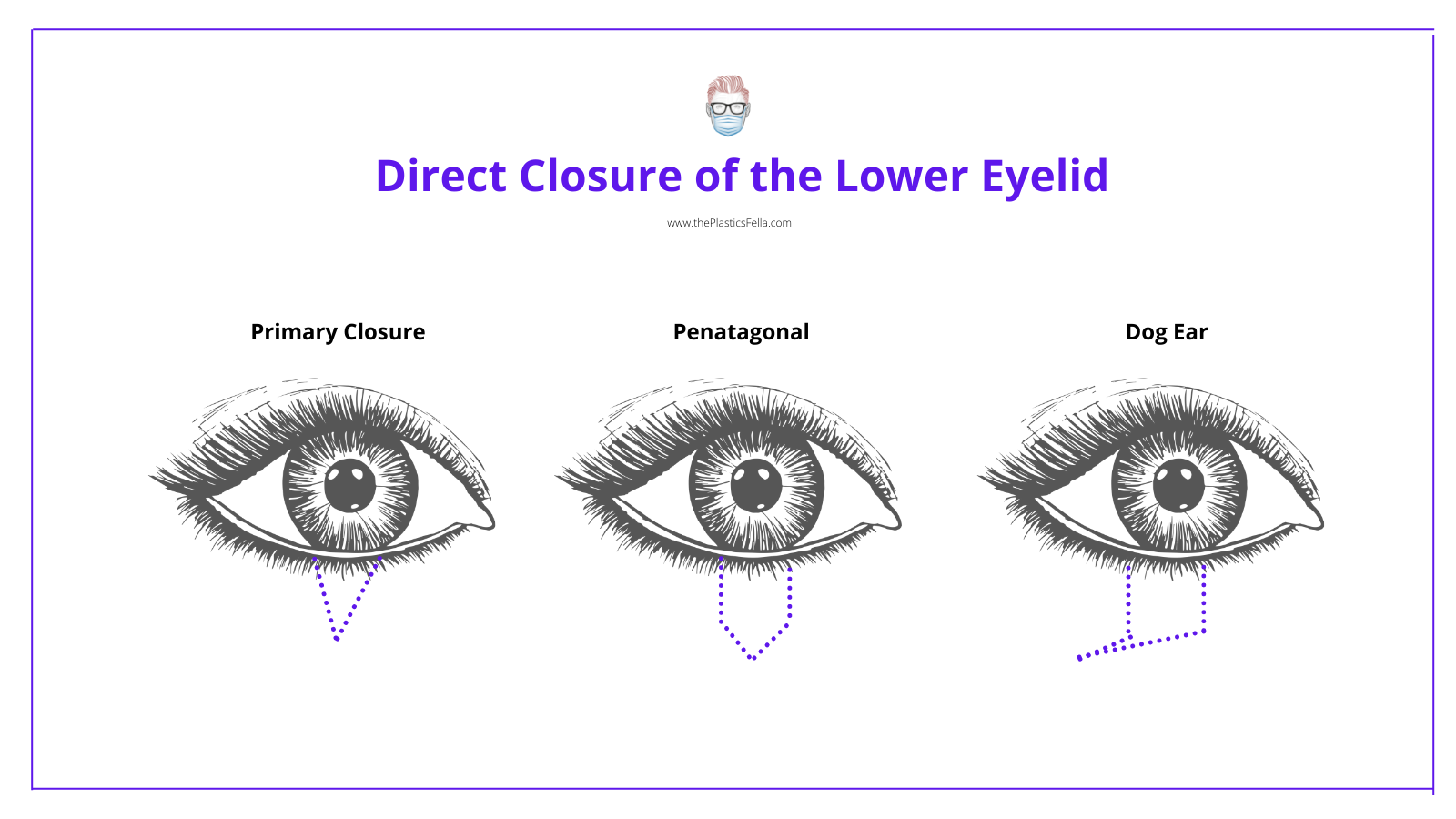
To assist the primary closure, the following can be considered:
- Lateral cantholysis and canthotomy can add ~5mm advancement.
- A pentagonal incision creates a square-edged tarsal defect.
- A lateral dog-ear incision reduces the risk of ectropion.
Bleeding may occur due to injury to the marginal artery, which often responds to compression.
There is a high risk of ectropion if the closure is too tight. Advantages of direct closure include:
- No donor site morbidity
- Lash continuity
Grafts for Lower Eyelid Reconstruction
The use of grafts in lower eyelid reconstruction is indicated for partial-thickness defects or as an adjunct to full-thickness defect reconstruction. There are 3 main types of grafts used.
Full Thickness Skin Graft
- A common option for partial-thickness defects of the anterior lamella.
- Donor sites can be the contralateral lid or post-auricular area.
- Contraindicated in conjunctival defects due to corneal irritation.
- Not suitable for full-thickness defects.
Mucosal Graft
- Can be used in conjunctival and tarsal plate reconstruction
- Graft contraction is an issue (less in nasal compared to buccal mucosa)
- Donor sites include hard palate or buccal mucosa (lots of tissue so it can be useful is large conjunctival defect)
Cartilage Graft
- It can be used to reconstruct tarsal plate
- Tarsal plate precision is key for structural lid support.
- Donor sites include auricular and septal cartilage.
Tarsoconjunctiva Grafts
- Donor site is from the intact eyelid.
- Similar to a Hughes Flap, but it is detached.
Flap Reconstruction of Lower Eyelid
Flap reconstruction can be used for both partial and full-thickness defects of the lower eyelid. They can be used in conjunction with a graft. They can be skin-only (cutaneous), skin-muscle (myocutaneous), tarsoconjunctival, or have eponymous names, as described below.
Anterior Lamella Reconstruction
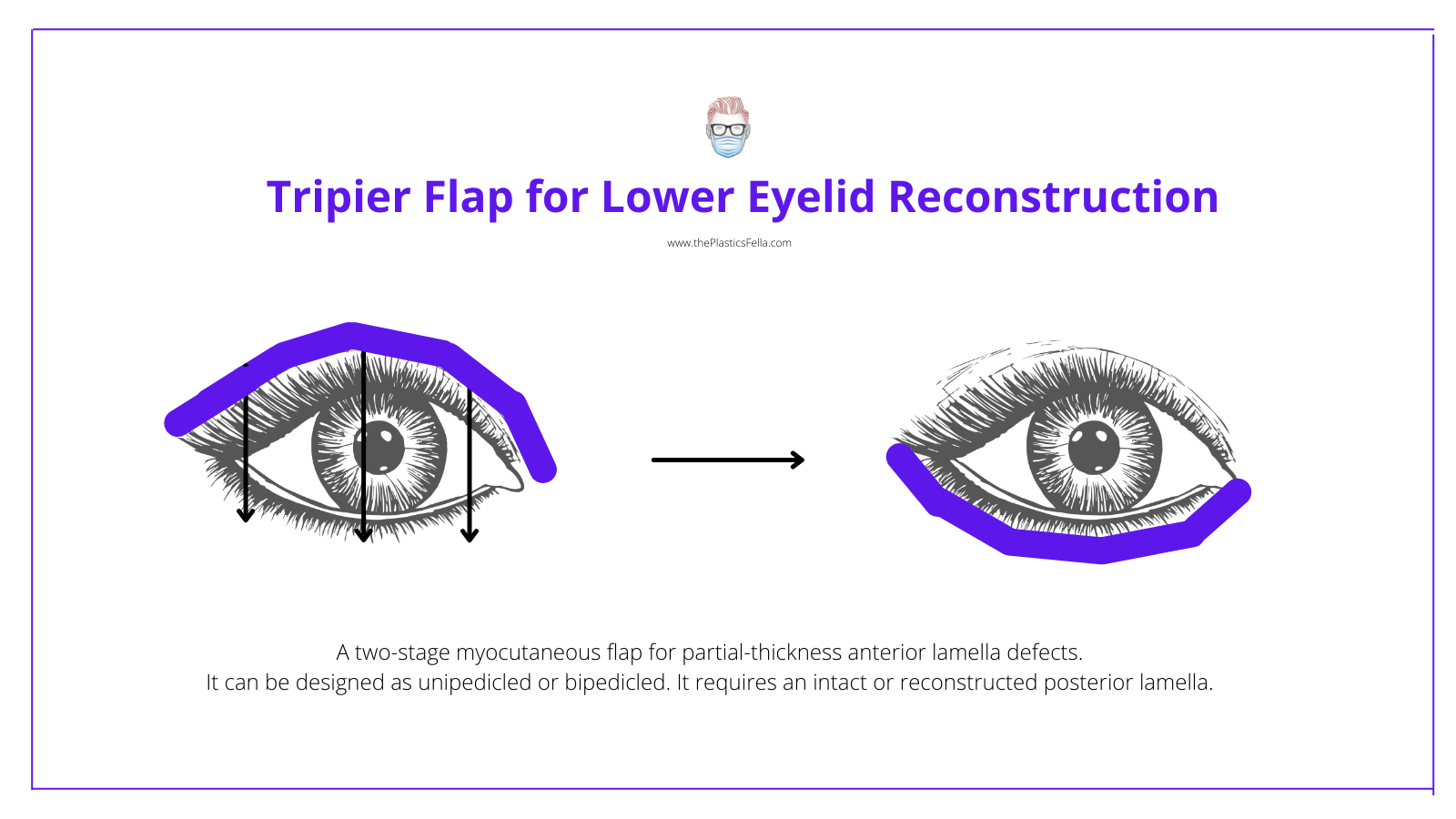
Tripier Flap
- 2-stage myocutaneous flap for partial-thickness anterior lamella defects.
- Skin & orbicularis from the upper eyelid is transferred to the lower eyelid.
- Designed as unipedicled or bipedicled (reduces the risk of distal necrosis).
- Useful if the defect is the majority of the lower eyelid.
- Requires an intact or reconstructed posterior lamella.
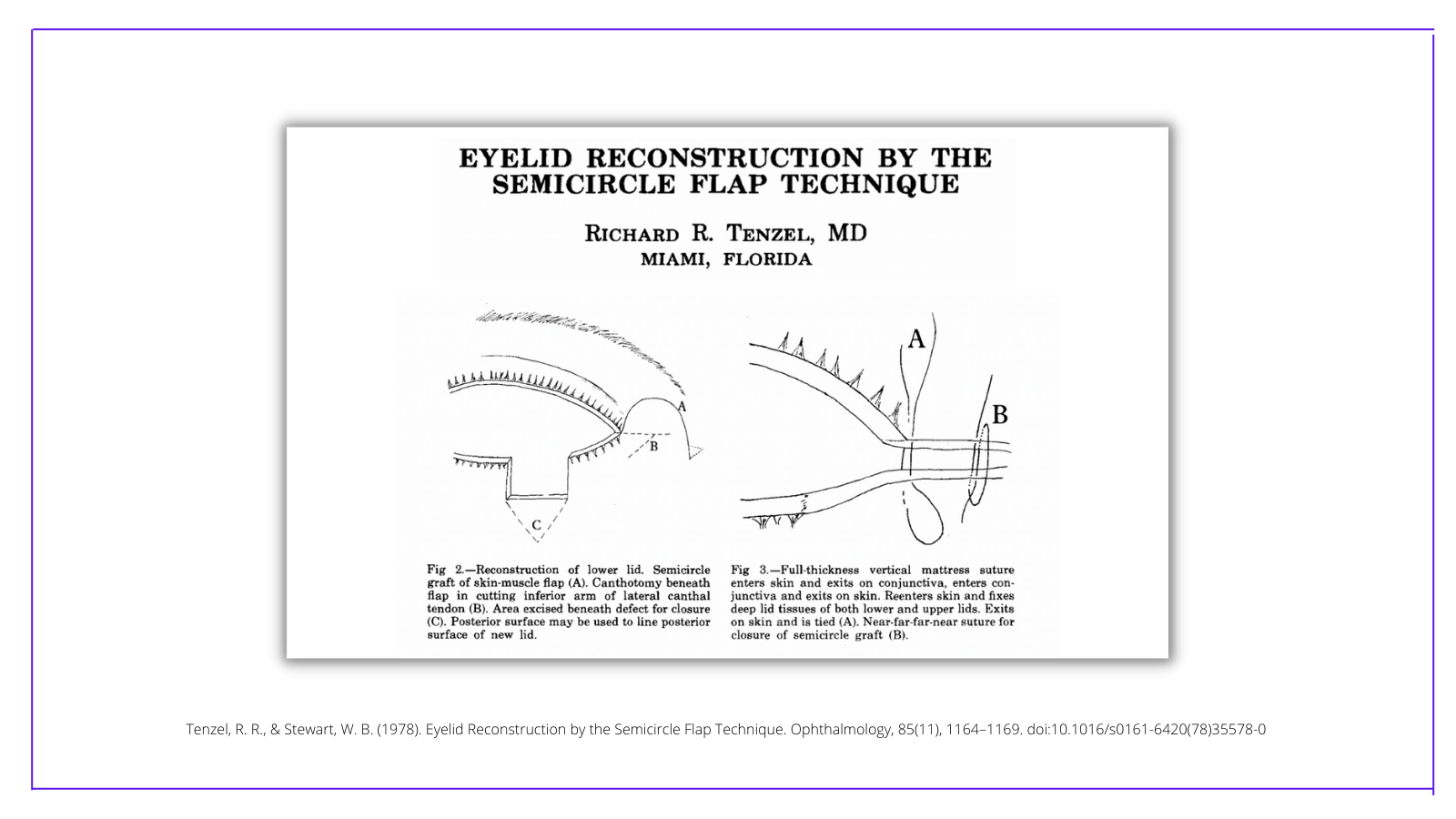
Tenzel semi-circular rotation flap
This is a laterally-based myocutaneous flap that is useful if the defect is <2/3 majority of the lower eyelid. The technique allows a step-wise process to an eyelid closure:
- A lateral canthotomy followed by a cantholysis (provides ~5mm)
- If a further 5mm is required, convert to a Tenzel flap.
The benefits of this flap include the following:
- Versatile, relatively simple
- It can be applied to the upper and lower eyelid.
Some literature suggests it requires an intact or reconstructed posterior lamella (which can be done with a periosteal flap from the lateral orbit). Anecdotally, the conjunctiva does not always need to be reconstructed because it will epithelialise.
Mustarde Flap (Cheek)
- Cheek advancement flap for large defects
- Useful if the defect is the majority of the lower eyelid.
- Aim for tension-free inset with lateral canthal fixation.
- Requires intact or reconstructed posterior lamella.
Fricke Flap (Temporal)
- Two-stage reconstruction useful soft-tissue overlying temporal area
- Useful in anterior lamella defects
- Risk of damaging the temporal branch of the facial nerve
- Limited by the fact it is introducing thick skin into the lower eyelid.
- Requires intact or reconstructed posterior lamella.
McGregor Flap
- Lateral advancement flap
- Straddles subunits and requires dissection in 2 separate planes
Posterior Lamella Reconstruction
Hughes tarsoconjunctival flap (Upper Eyelid)
- Two-stage transfer of upper eyelid conjunctiva and tarsus
- Flap of tarsus and its attachment to Müller muscle is preserved to improve flap blood supply and reduce the risk of tethering that results in upper eyelid contraction.
- Useful if the defect is the majority of the lower eyelid.
- Requires an intact or reconstructed anterior lamella by flap or FTSG.
- 3-4 mm of tarsal height in the upper eyelid donor site is preserved to prevent upper-lid margin distortion and entropion.
- Division of the flap occurs within 3 weeks.
- Limitations include: monocular for 3-4/52, corneal irritation, lid retraction and entropian.
Modified-Hughes Advancement Flap (Upper eyelid)
- A composite advancement of the tarsus and conjunctiva
- Useful for posterior lamella defects
- Two-stage procedure
- Requires intact or reconstructed anterior lamella.
Hewes Tarsal Transposition Flap
- Laterally-based tarsoconjunctival flap
- Donor site closed directly
- For defects extending into or involving the lateral canthus
- Caution: similar sound but different spelling to Hughes Flap
Supportive Techniques
Anchoring Sutures
Flap reconstruction is supported through anchoring techniques. These include:
- Lateral Canthus: direct fixation into the periosteum
- Medial Canthus: direct fixation to connective tissue behind the lacrimal sac or nasal into periosteum.
Lateral Cantholysis
A lateral cantholysis mobilises the lower lid to reduce the tension on primary closures. One method for this to be performed is:
- Lateral canthotomy to get access to the lateral canthal tendon
- Division of the lower limb of the lateral canthal tendon ("a tight band")
- A medial advancement after release (~5mm of advancement)
Flashcards
They are continually updated for thePlasticsPro users.
This is for thePlasticsPro
Join the Club to enjoy unlimited access to all of thePlasticsFella.
Join the Club

