Summary Card
Overview
LASER technology enables precise, minimally invasive treatments through selective photothermolysis, with applications in resurfacing, scar revision, and lesion treatments.
Mechanism of Action
Lasers generate collimated, monochromatic, and coherent light, interacting with tissue through reflection, scattering, transmission, or absorption.
Clinical Applications
Lasers are classified based on their target chromophore, which determines their clinical applications.
Complications
Laser treatments pose risks including hyperpigmentation, hypopigmentation, scarring, infection, and ocular injury.
Primary Contributor: Benedetta Agnelli, Educational Fellow
Verified by thePlasticsFella ✅
Overview of Lasers
Laser technology in plastic surgery enables targeted, minimally invasive treatments by selectively converting light to heat.
LASER stands for "Light Amplification by Stimulated Emission of Radiation." It achieves targeted treatment of vascular lesions, pigmented disorders, tattoos, and scars by converting absorbed laser energy into heat through selective photothermolysis.
Key milestones in LASER history:
- 1960: Maiman develops the first ruby laser.
- 1964: CO₂ laser introduced for ablative treatments.
- 1984: First laser-assisted blepharoplasty by Dr. Baker.
- Mid-1990s: Er:YAG lasers introduced for skin resurfacing, alone or with CO₂ lasers
In 1917, Albert Einstein described stimulated emission—the key principle behind lasers.
Mechanism of Action of Lasers
Lasers produce collimated, monochromatic, and coherent light that interacts with tissue, inducing biological effects—most notably, selective photothermolysis.
Laser systems produce coherent, monochromatic, and collimated light through stimulated emission. Their operation—comprising laser generation, wavelength-dependent tissue interactions, and biological effects (especially selective photothermolysis)—is detailed below.
Laser Generation
LASER is generated through three key components:
- Energy: Provides excitation energy (e.g., flashlamp or electrical discharge).
- Laser Medium: Determines the wavelength (e.g., solid Nd:YAG)
- Optical Resonator: Uses reflective mirrors to guide & amplify the beam.
This enables light to interact with tissue and generate heat.
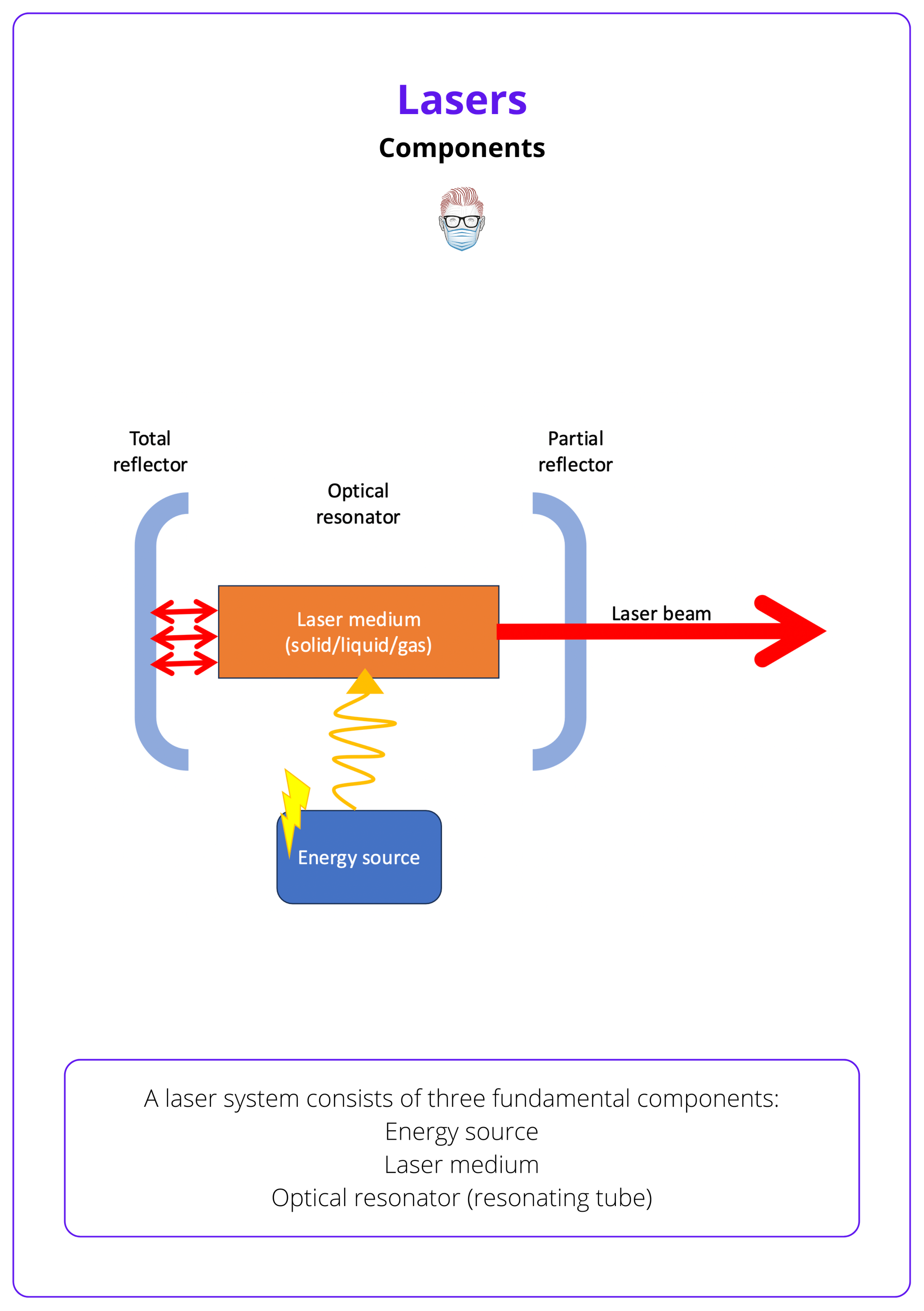
The laser medium often determines the laser’s name (e.g., CO₂ laser for carbon dioxide, Nd:YAG laser for neodymium-doped YAG).
Tissue Interactions
Light produced by the LASER interacts with tissue. Its behaviour is determined by its wavelength can result in:
- Reflection: The light bounces off the tissue surface with no effect.
- Scattering: The light disperses in multiple directions, reducing precision.
- Transmission: Unabsorbed light passes through the tissue without interaction
- Absorption: Specific chromophores absorb the light, converting it into heat (e.g., haemoglobin, melanin, tattoo pigment, water).
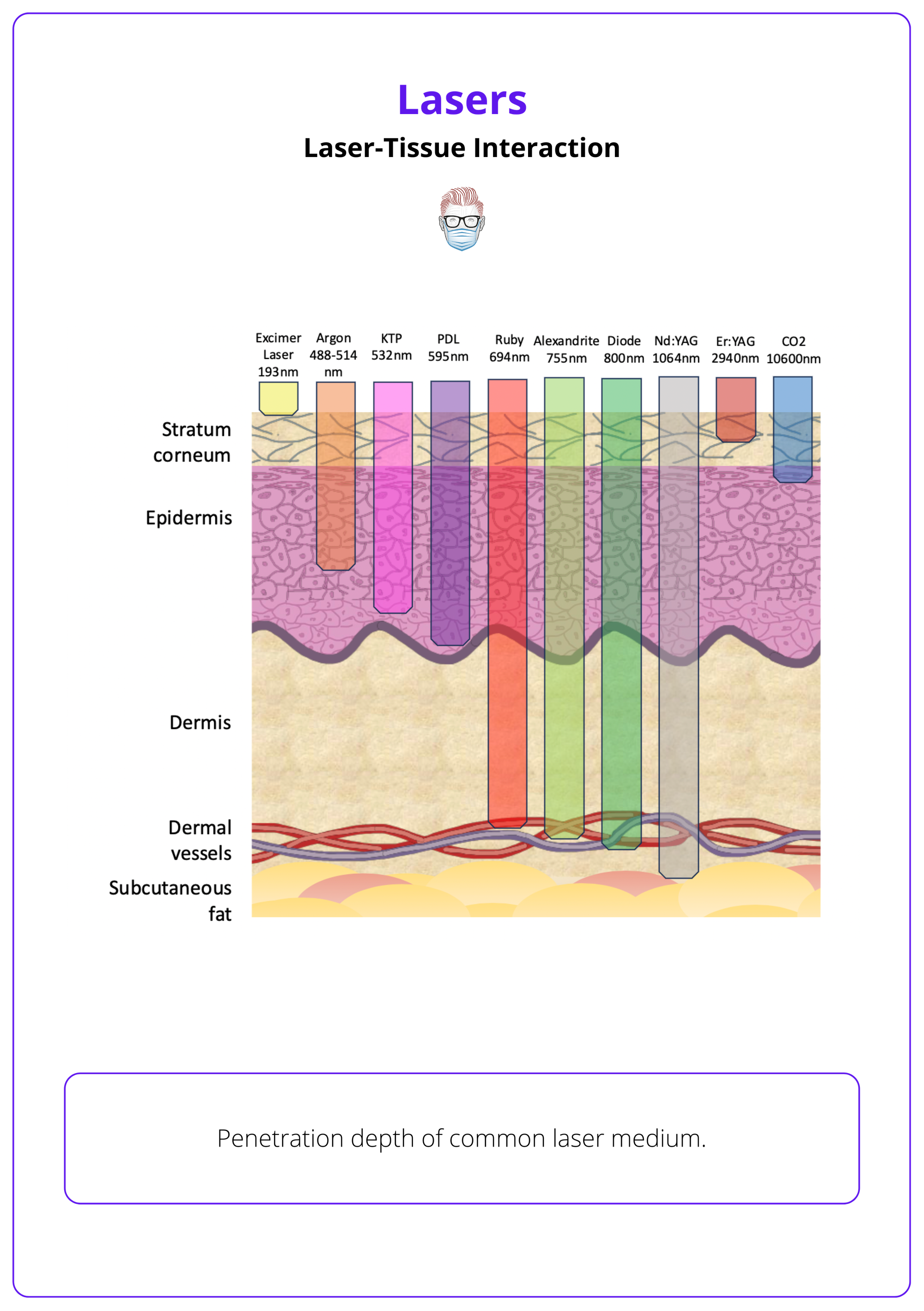
The specific wavelength of a laser determines its depth of penetration and interaction with biological tissues. Higher wavelengths correlate with deeper tissue penetration.
Biological Effects
This absorption of laser energy by specific chromophores converts the energy into heat and precisely targets tissue while sparing adjacent structures. This heat induces various biological effects:
- Photothermal: Heat causes vaporization, coagulation, or protein denaturation (e.g., CO₂ laser for resurfacing, Nd:YAG for coagulation).
- Photomechanical: High-energy pulses generate acoustic waves that fragment tissue (e.g., Q-switched lasers for tattoo removal).
- Photochemical: Light triggers chemical reactions without significant heat (e.g., photodynamic therapy).
- Photoelectrical: High-energy ionization occurs (rarely used in plastic surgery).
Selective photothermolysis uses precise wavelengths and pulses to produce a photothermal effect that destroys target chromophores while sparing adjacent tissue. It underpins vascular ablation (PDL), hair removal (Alexandrite/Diode), and pigment reduction (Q-switched). Not all laser-tissue interactions are photothermal.
Clinical Applications of Laser Types
Lasers are classified by their target chromophores, enabling specific wavelengths to treat vascular lesions, pigmentation, tattoos, and scars.
Lasers are classified by the chromophore they target, which determines their clinical use. Specific wavelengths interact with chromophores—such as hemoglobin, melanin, tattoo pigments, or water—to treat vascular, pigmented, and textural abnormalities.
Vascular Lesions
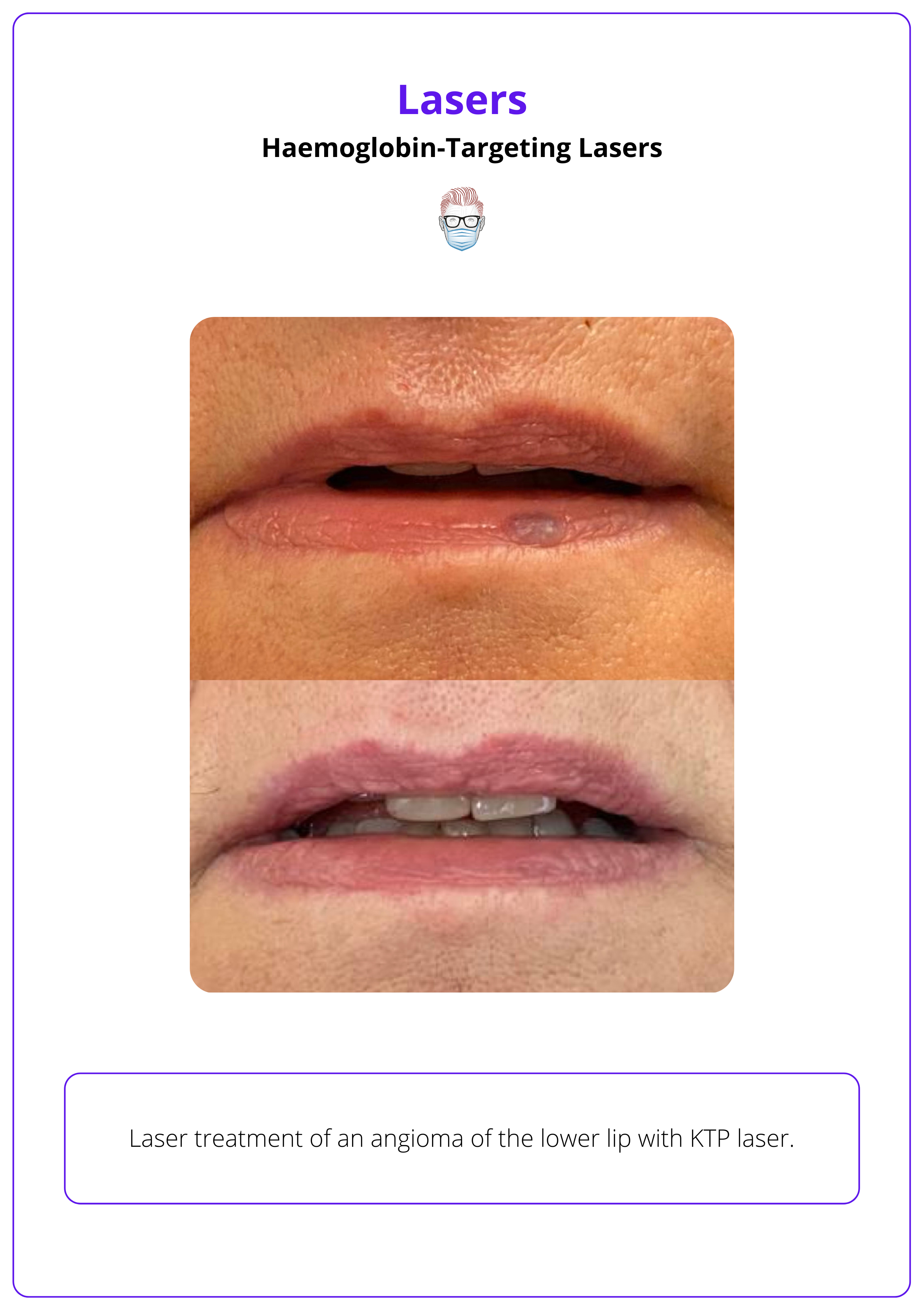
Haemoglobin-Targeting Lasers exploit the selective absorption of oxy- and deoxyhemoglobin to induce thermal coagulation and destroy abnormal vessels while sparing adjacent tissue.
Devices
- Superficial: KTP (532 nm), IPL (560 nm), PDL (585–595 nm), Alexandrite (755 nm)
- Deeper: Diode (810 nm) and Nd:YAG (1064 nm)
Conditions
- Congenital Vascular Lesions: Capillary vascular malformations, infantile hemangiomas, and angiomas.
- Acquired Vascular Lesions: Telangiectasias, spider veins, reticular veins, postprocedural purpura, and erythematous scars.
The image below showcases the pre-treatment and post-treatment results of a lower lip angioma successfully treated with laser therapy.
1. For higher Fitzpatrick skin types, use longer wavelengths to reduce melanin absorption.
2. Adjust pulse width to specifically target the vessel.
3. Apply epidermal cooling to protect the skin.
Pigmented Lesions
Melanin is the primary chromophore responsible for cutaneous pigmentation. Absorption by melanin enables targeted destruction of pigmented lesions or hair follicles through Melanin-Targeting Lasers. Optimal wavelength selection is crucial based on whether the melanin is located in the epidermis, dermis, or both.
Devices:
- Superficial: KTP (532 nm), IPL (560 nm)
- Broad-Spectrum: Q-Switched Nd:YAG (532 nm & 1,064 nm), Alexandrite (755 nm), Diode (800–810 nm)
Conditions:
- Epidermal Pigmentation: Lentigines, ephelides, seborrheic keratoses, café-au-lait macules, Becker nevi
- Dermal Pigmentation: Nevus of Ota, nevus of Ito, Mongolian spots, drug-induced hyperpigmentation
- Mixed Lesions: Post-inflammatory hyperpigmentation (PIH), melasma
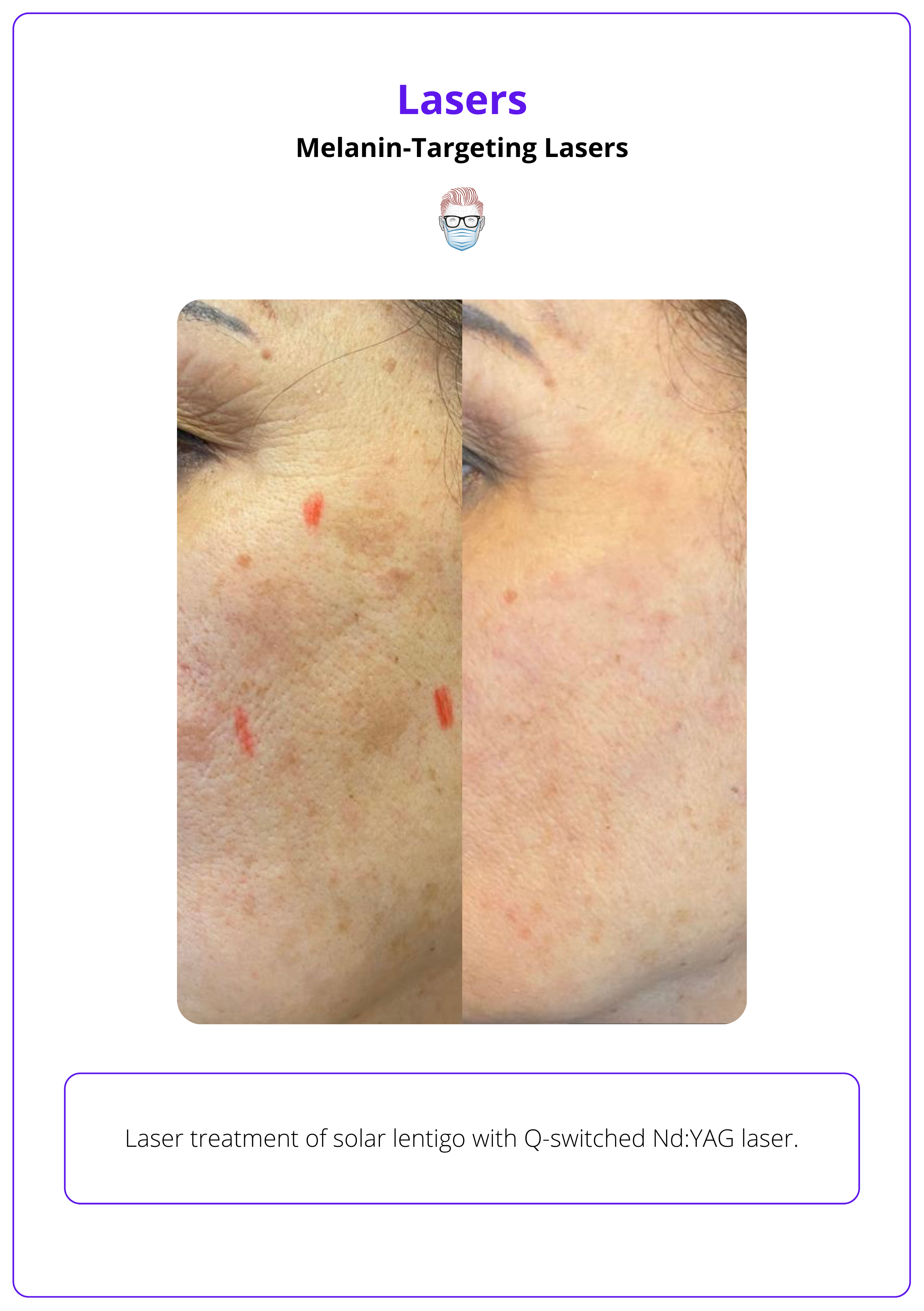
Before laser treatment, evaluate pigmented lesions, and any suspicion of malignancy requires a biopsy.
Hair Removal
Laser hair removal works by targeting the melanin in hair follicles, converting laser energy into heat that selectively damages the follicle and prevents regrowth.
- Primary Wavelengths: Alexandrite (755 nm) and Diode (800–810 nm)
- For Deeper Follicles: Nd:YAG (1064 nm)
Melanin within the hair shaft can also be targeted in order to perform laser hair reduction (LHR).
Tattoo Pigment-Targeting Lasers
Tattoo pigment-targeting lasers remove tattoos by using wavelengths absorbed by the ink. This triggers photothermal and photomechanical effects that fragment the pigment into smaller particles, which are then cleared via the lymphatic system or rendered visually imperceptible.
The colour and wavelength required for tattoos includes Nd:YAG, Alexandrite, Ruby, KTP and Titanium Sapphire. This is detailed in the table below.
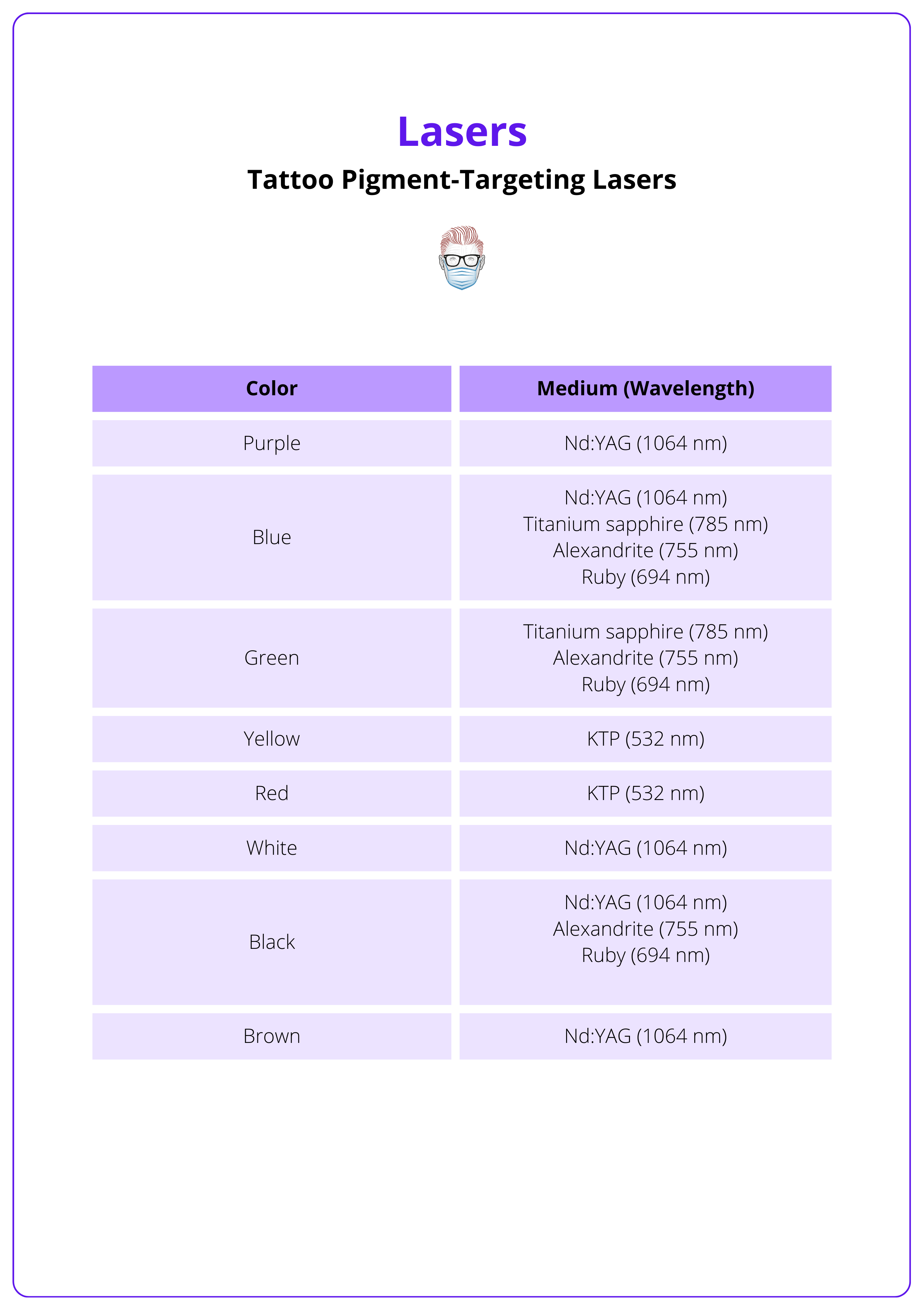
It is estimated that 17% of patients with tattoos have considered elective removal (Bencini, 2012).
Water-Targeting Lasers
Water, as a ubiquitous chromophore in skin, lacks structural selectivity due to its high absorption efficiency. Modern laser systems overcome this by employing central pattern generators and scanners to deliver controlled microinjury with precise penetration depths.
The tissue response depends on the wavelength of light.
- Ablative Lasers: CO₂ (10,600 nm) and Er:YAG (2,940 nm) lasers induce rapid tissue vaporization, making them ideal for skin resurfacing, scar revision, and lesion excision.
- Non-Ablative Lasers: Er:YAG and Nd:YAG lasers (1,550 nm, 1,927 nm) generate controlled thermal effects within the dermis without removing the epidermis. Stimulates collagen remodeling for wrinkle reduction, skin tightening, and acne scar treatment.
- Fractional ablative systems (eg CO₂ fractional, Er:YAG fractional) create microthermal zones that promote faster healing by sparing surrounding tissue, while conventional non-fractional ablative lasers provide uniform ablation but require longer recovery times.
These lasers are widely used for treating rhytides, atrophic scars, dyschromias, and photodamage, offering tailored approaches based on patient needs and skin types.
Complications of Laser Treatment
Laser treatments carry risks including pigmentary changes, scarring, infection, and ocular injury, with darker skin types (Fitzpatrick IV–VI) at increased risk for post-inflammatory hyperpigmentation.
While lasers offer precision, improper settings or techniques can lead to complications. Key issues include:
- Erythema & Edema: Temporary redness and swelling that typically resolve without intervention.
- Pigmentary Changes: Fitzpatrick I–III: Higher risk of hypopigmentation after aggressive treatments. Fitzpatrick IV–VI: Increased risk of post-inflammatory hyperpigmentation.
- Scarring: More likely with excessive fluence or improper technique.
- Infection: Particularly with ablative lasers; prophylactic antivirals or antibiotics are recommended for high-risk patients.
- Ocular Injury: Direct or reflected laser beams can damage the retina; use of protective eyewear is mandatory.
Always perform a test spot to assess skin response and adjust parameters, especially in darker or sensitive skin.
Conclusion
1. Overview: Lasers enables precise, minimally invasive treatments through selective photothermolysis, with applications in resurfacing, scar revision, and lesion treatments.
2. Mechanism of Action: Lasers emit collimated, monochromatic, and coherent light, interacting with tissue via absorption, reflection, scattering, or transmission.
3. Types & Clinical Applications: Lasers are categorized based on their target chromophore.
4. Risks & Complications: Hyperpigmentation, hypopigmentation, scarring, infection, and ocular injury are key risks. Test spots and cooling help reduce complications.
Further Reading
- Hersant B, SidAhmed-Mezi M, Bosc R, Meningaud JP. Current indications of low-level laser therapy in plastic surgery: a review. Photomed Laser Surg. 2015 May;33(5):283-97. doi: 10.1089/pho.2014.3822. PMID: 25954831.
- Zhang DD, Zhao WY, Fang QQ, Wang ZC, Wang XF, Zhang MX, Hu YY, Zheng B, Tan WQ. The efficacy of fractional CO2 laser in acne scar treatment: A meta-analysis. Dermatol Ther. 2021 Jan;34(1):e14539. doi: 10.1111/dth.14539. Epub 2020 Nov 23. PMID: 33190373.
- Azadgoli B, Baker RY. Laser applications in surgery. Ann Transl Med. 2016 Dec;4(23):452. doi: 10.21037/atm.2016.11.51. PMID: 28090508; PMCID: PMC5220034.
- Hernandez L, Mohsin N, Frech FS, Dreyfuss I, Vander Does A, Nouri K. Laser tattoo removal: laser principles and an updated guide for clinicians. Lasers Med Sci. 2022 Aug;37(6):2581-2587. doi: 10.1007/s10103-022-03576-2. Epub 2022 May 23. PMID: 35604505.
- Goldman A, Wollina U. Komplikationen nach Laserbehandlung vaskulärer Veränderungen des Gesichts [Complications after laser treatment of facial vascular lesions]. Hautarzt. 2021 May;72(5):421-425. German. doi: 10.1007/s00105-021-04796-3. Epub 2021 Mar 19. PMID: 33740081.
- Kauvar AN, Wang RS. Laser treatment of cutaneous vascular anomalies. Lymphat Res Biol. 2004;2(1):38-50. doi: 10.1089/1539685041690391. PMID: 15609926.
- Grabb, W. C., Smith, J. W., & Thorne, C. H. (2013). Grabb and Smith's Plastic Surgery (7th ed.). Philadelphia: Wolters Kluwer.


