Summary Card
Definition
Keloid is a dermo-fibroproliferative disorder thought to result from abnormal proliferation of fibroblasts.
Pathophysiology
Development involves genetic predisposition, inflammation, mechanical stress, and chronic inflammation of the reticular dermis, causing dysregulated fibroblast activity and excess ECM production.
Clinical Features
Keloids extend beyond the original wound boundary and may present with pain, itching, or burning.
Treatment
Keloid treatment includes non-pharmaceutical options like lasers and surgery and pharmaceutical options like corticosteroids and 5-FU.
Primary Contributor: Dr Waruguru Wanjau, Educational Fellow.
Definition of Keloids
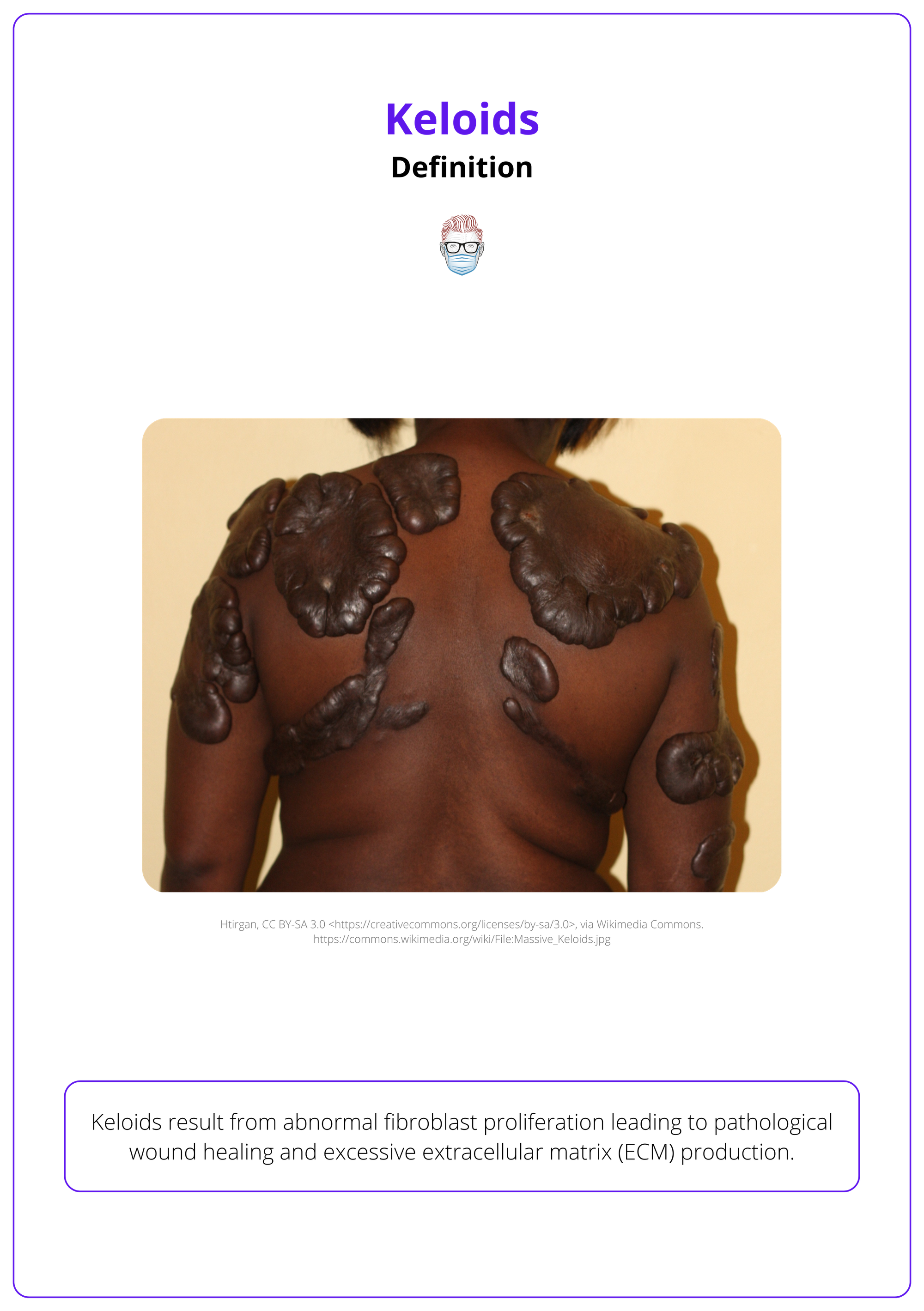
Keloid is a dermo-fibroproliferative disorder thought to result from abnormal proliferation of fibroblasts.
Keloid scars are an abnormal response to dermal injury, characterized by persistent fibroblast hyperactivity and excessive extracellular matrix (ECM) deposition. Unlike typical scars, keloids extend beyond the boundaries of the original wound and fail to regress over time (Wanjala, 2022).
At a cellular level, keloid scars have the following features (Lee, 2023):
- Collagen Composition: Keloids are marked by excessive Type I and III collagen, with an altered matrix composition compared to normal scar tissue.
- Persistent Inflammation: Chronic activation of inflammatory pathways sustains fibroblast proliferation and ECM accumulation.
- Prolonged Remodeling Phase: Unlike normal wound healing, where remodeling resolves fibrosis, keloids remain in an active state of tissue remodeling and expansion.
Large keloid scars on the back are illustrated below.
Pathophysiology of Keloids
Keloid formation results from a combination of genetic predisposition, environmental triggers, and chronic inflammation that disrupts normal wound healing. The primary pathology involves dysregulated fibroblast activity and excessive extracellular matrix (ECM) deposition.
Keloids arise from chronic inflammation in the reticular dermis (Ogawa, 2021). It usually has a triggering event which is then influenced by genetic predisposition, inflammatory processes, and mechanical stress.
- Triggering Event: Skin injuries (e.g., surgery, burns, acne) commonly trigger keloids.
- Fibroblast Dysregulation: Overactive fibroblasts synthesize excessive collagen and resist apoptosis, leading to persistent scarring (McGinty, 2023).
- Cytokine Imbalance: Elevated TGF-β levels drive fibroblast recruitment and chronic inflammation (Lee, 2023).
- Hormonal Influences: Estrogen-induced vasodilation, especially during pregnancy, aggravates keloid formation (Ogawa, 2021).
- Metabolic and Environmental Factors: Hypoxia, mechanical stress, and conditions like vitamin D deficiency or hypertension exacerbate keloid progression.
Clinical Features of Keloids
Keloids extend beyond the original wound boundary and are often associated with symptoms such as pain, itching, or burning.
Keloid scars are pathological scars that extend beyond the boundaries of the original wound & persist indefinitely, often causing physical discomfort & psychological distress. Diagnosis is primarily clinical, confirmed by histologic findings such as keloidal collagen and fibroblast density.
Clinical Features
Their key clinical features include,
- Locations: Deltoid, pre-sternal chest, upper back, and ear regions.
- Color: erythematous in early stages to hyperpigmented over time.
- Onset: 1–3 months after trauma but can develop up to a year later.
- Symptoms: Pruritus, pain, and burning are reported. (McGinty, 2023).
Risk Factors for keloid scar formation include,
- Family history increases keloid risk.
- Gender: Female predominance is linked to estrogen's role in vasodilation and scar inflammation.
- Ethnicity: Black 2.4%, Asian 1.1%, Caucasian 0.4% (Ung, 2023).
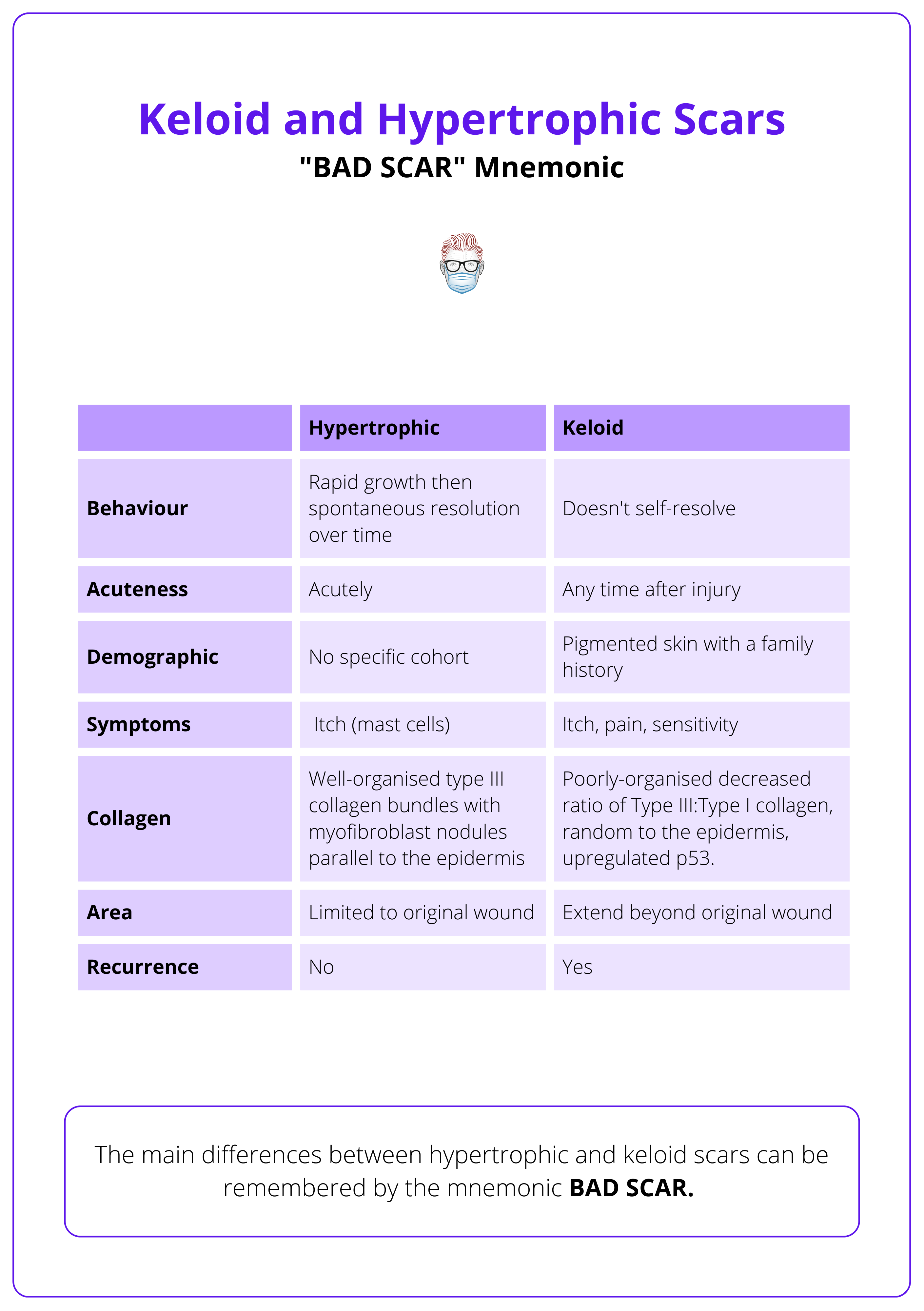
The table below categorizes keloids and hypertrophic scars along with their differences.
Malignant tumors, such as dermatofibrosarcoma protuberans, may mimic keloids clinically and require biopsy for confirmation (Ogawa, 2021).
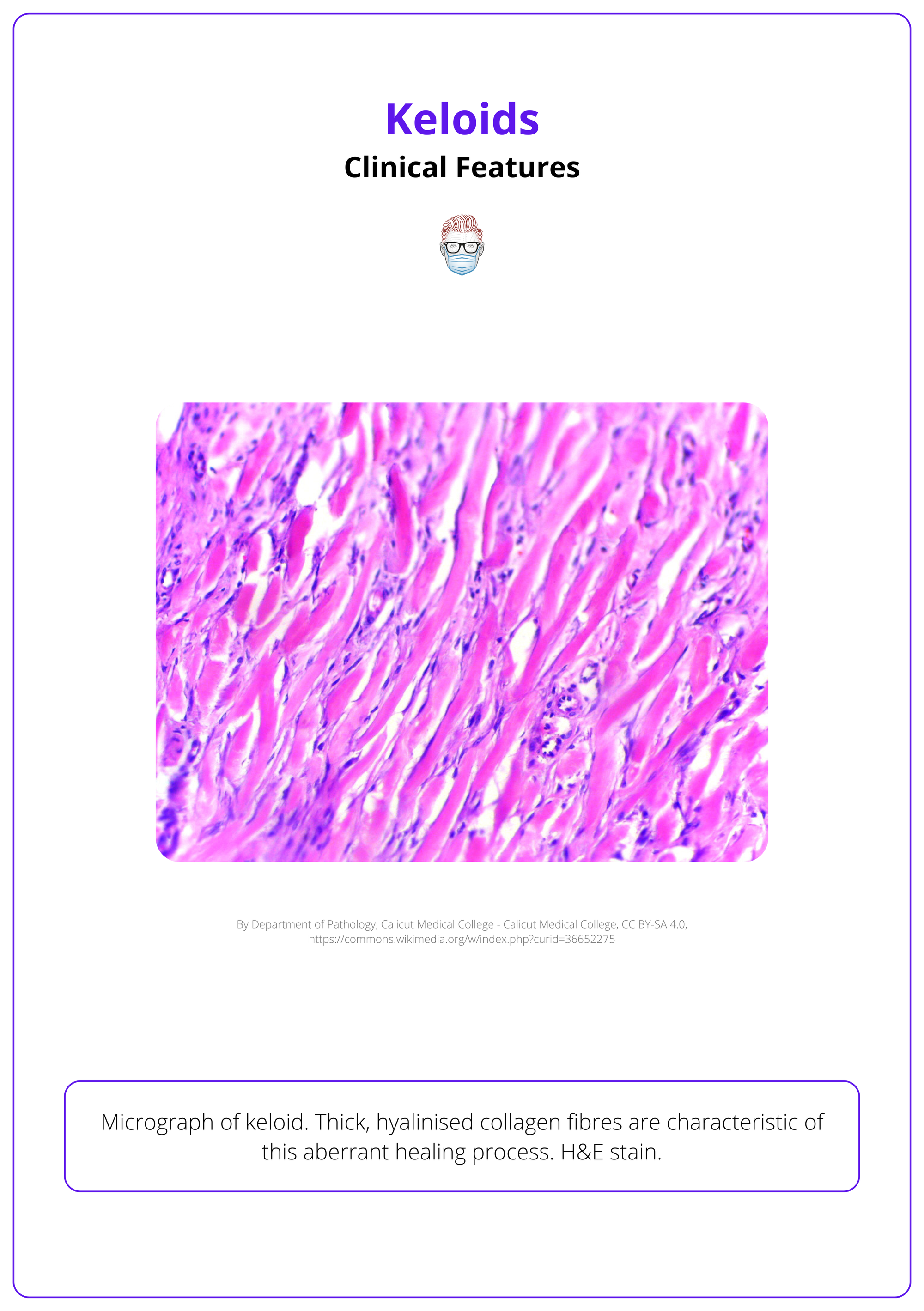
Histologic Features
Histologically, keloids are characterized by large, irregular, hyalinized collagen bundles, known as keloidal collagen, and an abundance of fibroblasts, which are central to their pathological structure (McGinty, 2023). Even in the absence of keloidal collagen, keloids can be identified by the following diagnostic features:
- Standard Epidermis and Papillary Dermis: The epidermis appears normal, with no significant abnormalities in the papillary dermis.
- "Tongue-Like" Advancing Edge: A projection of fibrous tissue extending below the papillary dermis is a hallmark of keloid expansion.
- Horizontal Fibrous Band: A dense, horizontal band of fibrous tissue in the upper reticular dermis is typically observed.
- Prominent Fascia-Like Band: A thick, fascia-like structure in the deep dermis contributes to the rigidity and persistence of keloids.
A micrograph of a keloid is illustrated below.
Differences in clinical presentation and histology between keloids and hypertrophic scars arise from variations in the intensity and duration of reticular dermis inflammation (Ogawa, 2021).
Treatment of Keloids
Keloid management integrates non-pharmaceutical approaches like lasers, silicone sheeting, cryotherapy, and surgery with pharmaceutical treatments such as corticosteroids, 5-Fluorouracil (5-FU).
Keloid treatment requires a tailored approach based on the lesion's characteristics, including size, number, and patient-specific risk factors. Both conservative and surgical strategies are often combined with adjuvant therapies to enhance outcomes and minimize recurrence.
Conservative Options
These methods target the physical and biological properties of keloids, improving outcomes in smaller or isolated lesions.
- Scar Massage: Increases blood flow, releases tissue adhesions, and induces mechanotransduction to aid scar remodeling.
- Pressure Therapy via Taping: Realigns collagen fibers, reduces collagen nodules, diminishes fibrotic activity, and reduces edema.
- Silicone Sheeting or Gel: Enhances scar pliability and color, reduces collagen production through occlusion, and hydrates the stratum corneum.
- Laser Therapy: Pulsed-dye laser (PDL), non-ablative fractional lasers, and carbon dioxide lasers. Laser-assisted topical steroid application for improved aesthetics.
Procedural Options
- Intralesional Corticosteroid injections at ~6-week intervals. Enhanced efficacy when paired with 5-FU or laser therapy but may cause pigmentation changes or tissue atrophy.
- Corticosteroid Tape is a painless alternative to corticosteroid injections. These include (Ogawa, 2021) Fludroxycortide tape or Deprodone propionate plaster (strong steroid).
- Cryotherapy Reduces collagen synthesis by inducing tissue necrosis. This can be applied through direct contact, sprays, or intralesional probes. Limitation include post-treatment pigmentation changes.
- Surgical Excision: Small keloids may be radically excised; large lesions require partial or core excision. Surgery alone has high recurrence rates (45–100%) and must be paired with adjuvant therapy such as radiation or steroids.
- Radiation Therapy inhibits fibroblast activity and angiogenesis, making it effective in preventing keloid recurrence. It should Administered within 24–28 hours post-surgical excision via electron beam radiation or brachytherapy (McGinty, 2023).
Monitor surgical sites prone to hypertrophic scars or keloids for 3–12 months. Start steroid tape or plaster at the first sign of induration, switching to steroid injections if it persists (Ogawa, 2021).
Other, currently less commonly used agents include,
- 5-Fluorouracil (5-FU): Effective when combined with steroids, reducing erythema and elevation.
- Bleomycin: Promotes apoptosis in fibroblasts.
- Retinoids: Enhances new scar remodeling by suppressing sebum and excessive fibroblast activity.
There are anecdotal reports of tissue-engineered allografts (Jones, 2016) and platelet-rich plasma for the treatment of keloids (Oswald, 2003).
Conclusion
1. Definition: Keloids are a dermo-fibroproliferative disorder caused by abnormal fibroblast activity and excessive ECM production, resulting in scars that extend beyond the wound boundary.
2. Pathophysiology: Keloids arise from genetic predisposition, mechanical stress, chronic reticular dermis inflammation, and dysregulated fibroblast activity.
3. Clinical Features and Diagnosis: Keloids commonly appear on the chest, back, shoulders, and ears, presenting as firm, raised scars with pain or itching. Diagnosis is clinical, supported by histologic findings.
4. Treatment: Management involves non-pharmaceutical methods (lasers, silicone sheeting, cryotherapy, surgery, radiation) and pharmaceuticals (corticosteroids, 5-FU, bleomycin).
5. Prevention: Preventative strategies include tension-free wound closure, silicone gel application, scar massage, and avoiding elective procedures like tattoos or piercings in predisposed individuals.
Further Reading
- McGinty S, Siddiqui WJ. Keloid. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
- Lee CC, Tsai CH, Chen CH, Yeh YC, Chung WH, Chen CB. An updated review of the immunological mechanisms of keloid scars. Front Immunol. 2023 Mar 22;14:1117630. doi: 10.3389/fimmu.2023.1117630. PMID: 37033989; PMCID: PMC10075205.
- Ung CY, Warwick A, Onoufriadis A, Barker JN, Parsons M, McGrath JA, Shaw TJ, Dand N. Comorbidities of Keloid and Hypertrophic Scars Among Participants in UK Biobank. JAMA Dermatol. 2023 Feb 1;159(2):172-181. doi: 10.1001/jamadermatol.2022.5607. PMID: 36598763; PMCID: PMC9857738.
- Ogawa R. The Most Current Algorithms for the Treatment and Prevention of Hypertrophic Scars and Keloids: A 2020 Update of the Algorithms Published 10 Years Ago. Plast Reconstr Surg. 2022 Jan 1;149(1):79e-94e. doi: 10.1097/PRS.0000000000008667. PMID: 34813576; PMCID: PMC8687618.
- Jones ME, Hardy C, Ridgway J. Keloid Management: A Retrospective Case Review on a New Approach Using Surgical Excision, Platelet-Rich Plasma, and In-office Superficial Photon X-ray Radiation Therapy. Adv Skin Wound Care. 2016 Jul;29(7):303-7. doi: 10.1097/01.ASW.0000482993.64811.74. PMID: 27300360; PMCID: PMC4915758.
- Osswald SS, Elston DM, Vogel PS. Giant right plantar keloid treated with excision and tissue-engineered allograft. J Am Acad Dermatol. 2003 Jan;48(1):131-4. doi: 10.1067/mjd.2003.48. PMID: 12522384.
- Katta R, Kramer MJ. Skin and Diet: An Update on the Role of Dietary Change as a Treatment Strategy for Skin Disease. Skin Therapy Lett. 2018 Jan;23(1):1-5. PMID: 29357214.
- Wanjala NF, Joseph G, Anthony M, Primus O, Ogeng'o JJ, Anzala O, Dohil I, Agak GW. Keloids: Does patients' sex influence the presentation and recurrence post-excision? J Plast Reconstr Aesthet Surg. 2022 Jan;75(1):366-368. doi: 10.1016/j.bjps.2021.08.030. Epub 2021 Sep 20. PMID: 34642061.
- Liu EK, Cohen RF, Chiu ES. Radiation therapy modalities for keloid management: A critical review. J Plast Reconstr Aesthet Surg. 2022 Aug;75(8):2455-2465. doi: 10.1016/j.bjps.2022.04.099. Epub 2022 May 6. PMID: 35817711.
- Theplasticsfella. Wound healing April 2022. Accessed on 24th November 2024.


