In this week's edition
- ✍️ Letter from P'Fella
FBI stops simultaneous surgery. - 🤓 The Sunday Quiz + Leaderboard
How well do you know melanomas? - 🎙️ Behind the 'Fella
Sneak peek from episode 03: All things research. - 🎓 theFellow's Corner
Fresh drop: Gynaecomastia pathophysiology, diagnosis, & treatment. - 📖 What Does the Evidence Say?
Adjuvant therapies in melanoma. - 🔥 Recommended Articles of the Week
Lymph node dissection, excision margins for thick cutaneous melanoma, & margins for primary cutaneous melanoma; with 1 sentence summaries. - 💕 Feedback
Suggest ideas & give feedback!
A Letter from P'Fella
FBI Stops Simultaneous Surgery
Big news: the FBI investigated a Medical Center, accusing three heart surgeons of running two ORs at once and letting residents handle complex surgeries. Let's break it down:
👇
Experienced surgeons often differentiate between aspects of surgical procedures that require their expertise and those that can be managed by senior residents or fellows. The practice of running multiple operating rooms simultaneously is usually designed to treat more patients efficiently.
These "surgical trainees" are often not novices; they are often fully trained fellows who require real surgical experience to refine their skills. However, the absence of hands-on practice could compromise future patient care. There is a significant debate surrounding this practice. Critics argue that entrusting complex parts of surgeries to residents could be risky, especially as modern medicine increasingly prioritizes safety and quality, which makes this practice controversial.
Patients typically provide informed consent, acknowledging the involvement of trainees in their surgeries. However, questions remain about the actual qualifications of these residents and whether patients fully understand the extent of trainee involvement.
The involvement of the FBI raises further questions. Typically, state medical boards are responsible for overseeing medical qualifications and practices, so why is a federal agency involved? This situation underscores the delicate balance between ensuring patient safety and providing necessary training to future surgeons—a balance that is crucial for the advancement and security of the medical field.
Let’s keep the conversation going!
❤️,
P'Fella
The Sunday Quiz
How Well Do You Know Melanomas?
Welcome to the next round of The Weekly Quiz.
Each edition of thePlasticsPaper includes a quiz question designed to challenge and engage our readers. Keep your wits about you and join in every week — the winner at the end of six rounds will earn you a $100 voucher.

We're planning to discuss melanomas in an upcoming podcast episode. Subscribe on Spotify or Apple to listen once it's out!
Behind the ‘Fella
Sneak Peek from Episode 03
If there's any specific discussion you're interested in, let us know below.
the Fellows' Corner
This Week's Focus: Gynaecomastia
In case you've missed out, here's a reminder to check out our fresh articles, clinical cases, and surgical techniques.
Read below for an overview of our article on Gynaecomastia.
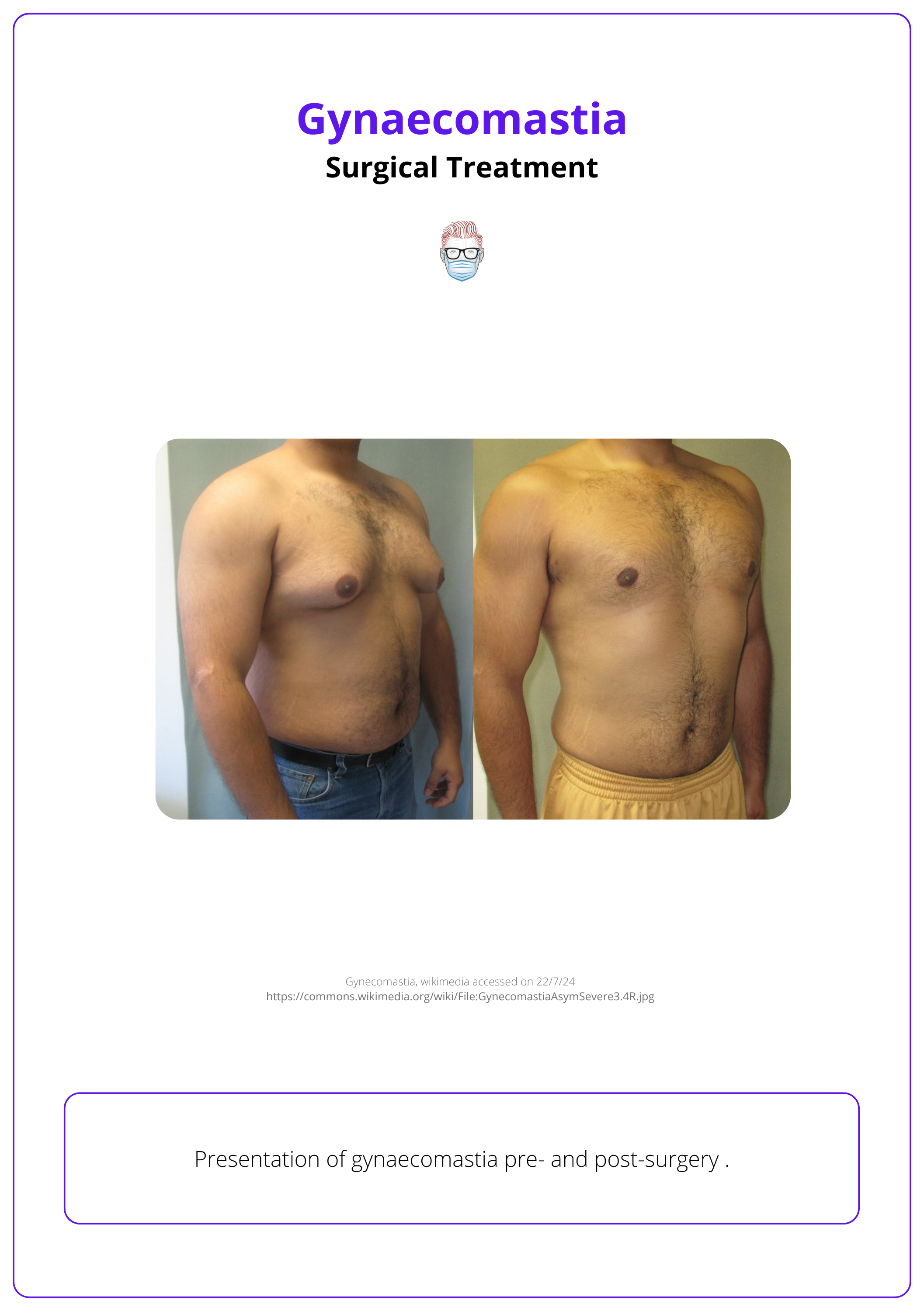
Gynaecomastia
Definition
Gynaecomastia (GM) is characterized by enlargement of the male breast, caused by glandular proliferation and fat deposition.
Pathophysiology
Gynaecomastia is caused by an imbalance of androgenic and oestrogenic effects on the breast.
Clinical Features
Gynaecomastia presents as bilateral, firm, concentric, and painless enlargement of the male breast.
Classification
Simon's classification is based on the degree of tissue and skin excess and Cordova is based on structural components of the breast. Gynaecomastia is staged using the Rohrich et al staging system.
Investigations
Evaluation of gynaecomastia must include a detailed medical history, clinical examination, specific blood tests, imaging, and tissue sampling.
Treatment
Treatment options include weight loss, reassurance, pharmacotherapy, and surgical resection or liposuction.
Complications
Complications of surgical excision include NAC loss, deformity, over/under resection, scarring, and recurrence.
What Does the Evidence Say?
Adjuvant Therapies in Melanoma
Major adjuvant trials have shown significant survival benefits for patients with resected Stage III melanoma.
- EORTC 18,201 demonstrated that ipilimumab significantly improved 5-year recurrence-free (40.8% vs. 30.3%) and overall survival (65.4% vs. 54.4%) compared to placebo.
- CheckMate 238 found nivolumab more effective than ipilimumab, with a 24-month relapse-free survival rate of 70.5% versus 63.7%.
- Combi-AD revealed that dabrafenib plus trametinib greatly reduced metastasis risk, achieving a 3-year relapse-free survival of 59% compared to 39% for placebo.
- EORTC 1325/KeyNote 054 showed pembrolizumab increased recurrence-free survival to 75.4% versus 61% for placebo.
- BRIM-8 indicated a modest effect of vemurafenib on disease-free survival in Stage IIC-III melanoma.
These studies confirm the efficacy of adjuvant therapies in improving outcomes for this patient group.
Articles of the Week
3 Interesting Articles with 1 Sentence Summaries
Immediate completion lymph node dissection in melanoma patients with sentinel-node metastases did not enhance melanoma-specific survival compared to nodal observation, but improved regional disease control and offered valuable prognostic insights, albeit with a higher risk of lymphedema.
A long-term study comparing 2-cm and 4-cm surgical excision margins for thick cutaneous melanoma found that both margins provide similar overall and melanoma-specific survival rates, suggesting that the narrower 2-cm margin is sufficient for effective treatment.
A pilot study (MelMarT) compared 1-cm and 2-cm surgical excision margins for primary cutaneous melanoma thicker than 1 mm, finding that both margins were feasible, with no significant differences in patient quality of life.


