In this week's edition
- ✍️ Letter from P'Fella
Surgery: A Numbers Game to Perfection - 🤓 The Sunday Quiz
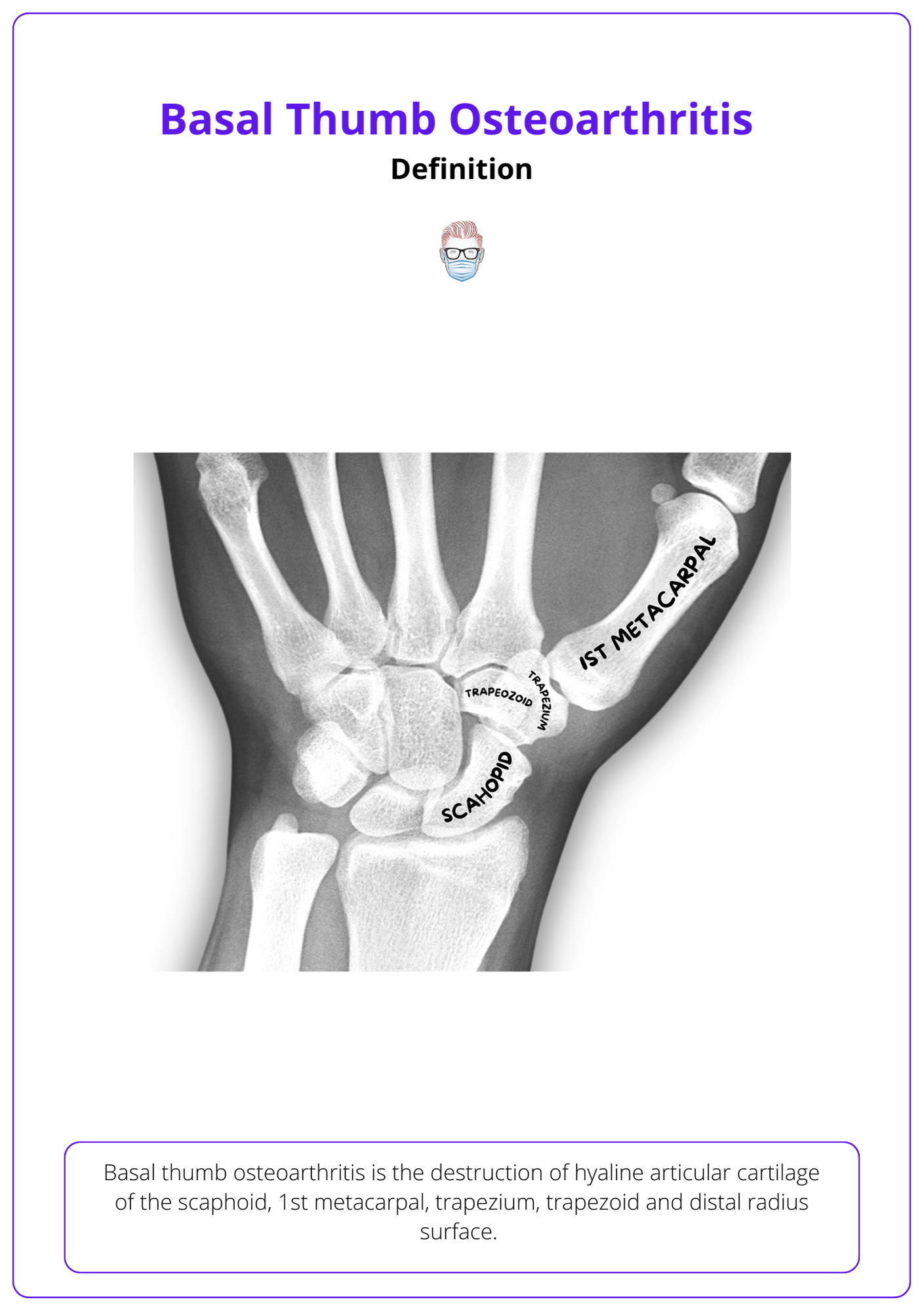
CMCJ arthritis classification (tips to remember) - 🎭 New & Upcoming
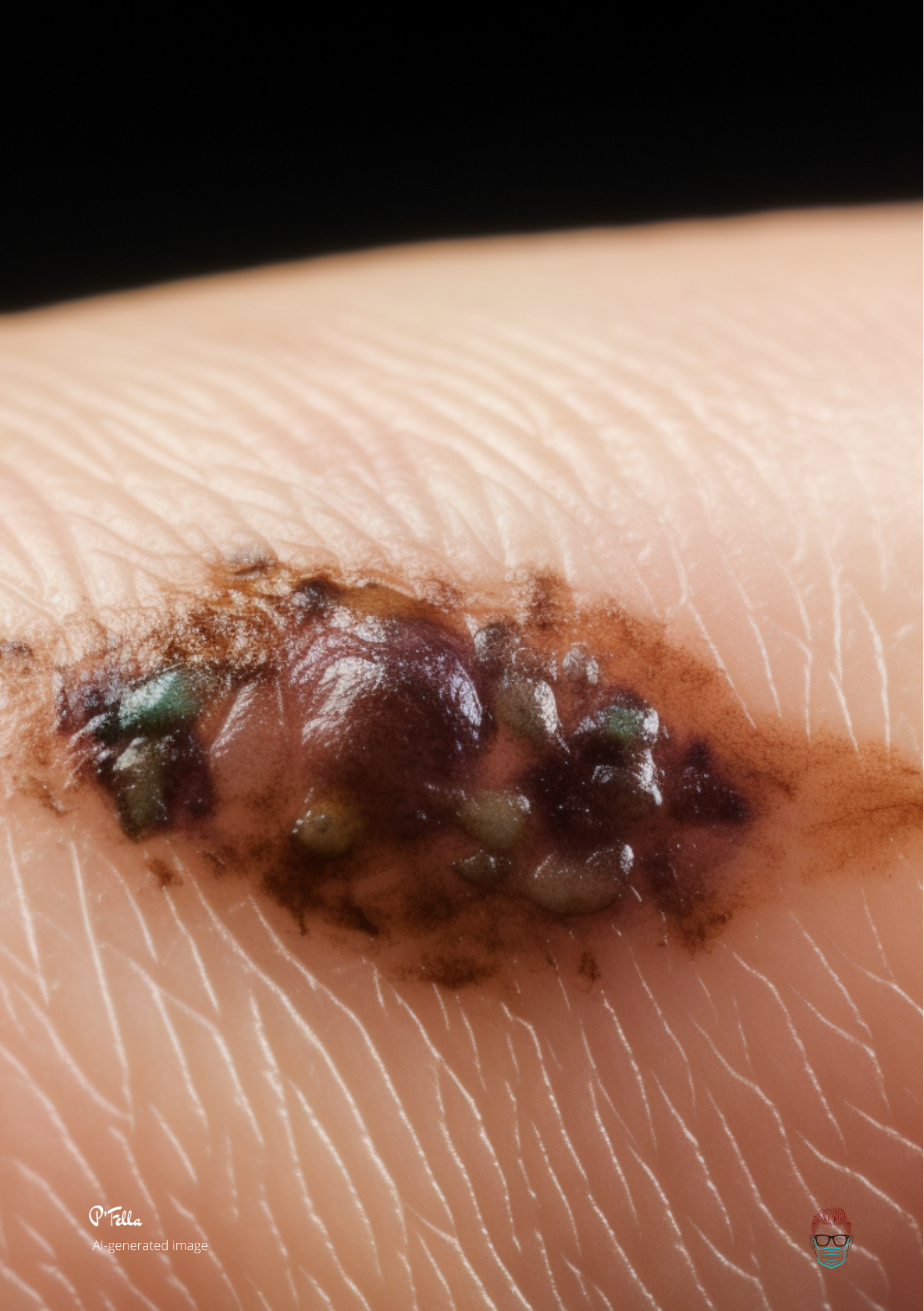
New Educational tools and upcoming events - 📸 Image of the Week
AI-generated nodular melanoma - 🐣 Tweets of the Week
P'Fella's 3 favourite tweets - 🤔 Ask P'Fella
Submit & I'll answer! - 📝 Articles of the Week
3 hot reads on UCLs, fractures and orthoplastics.
Deep dive: should we treat mallet fingers? - 💕 Feedback
Always looking to improve :)
BTW: Have your heard the deep-dive journal clubs are really good?
A Letter from P'Fella
Surgery: A Numbers Game to Perfection
Got a fresh spin on "practice makes perfect" for you. A study in The BMJ found that surgeons who perform more surgeries have better patient outcomes - the more we do, the better we get.
Read more 👇
Got a fresh (and evidence-based) spin on an old saying for you: practice makes perfect. But it's not just about repetition, it's about the numbers game in surgery. Intrigued? Let's get into it.
A study just out in The BMJ has found a fascinating link between the number of surgeries a surgeon performs and the outcomes for patients who undergo elective shoulder replacement surgery. Now, I hear you: "I'm a plastic and reconstructive surgeon, what's this got to do with me?" Stick with me here.
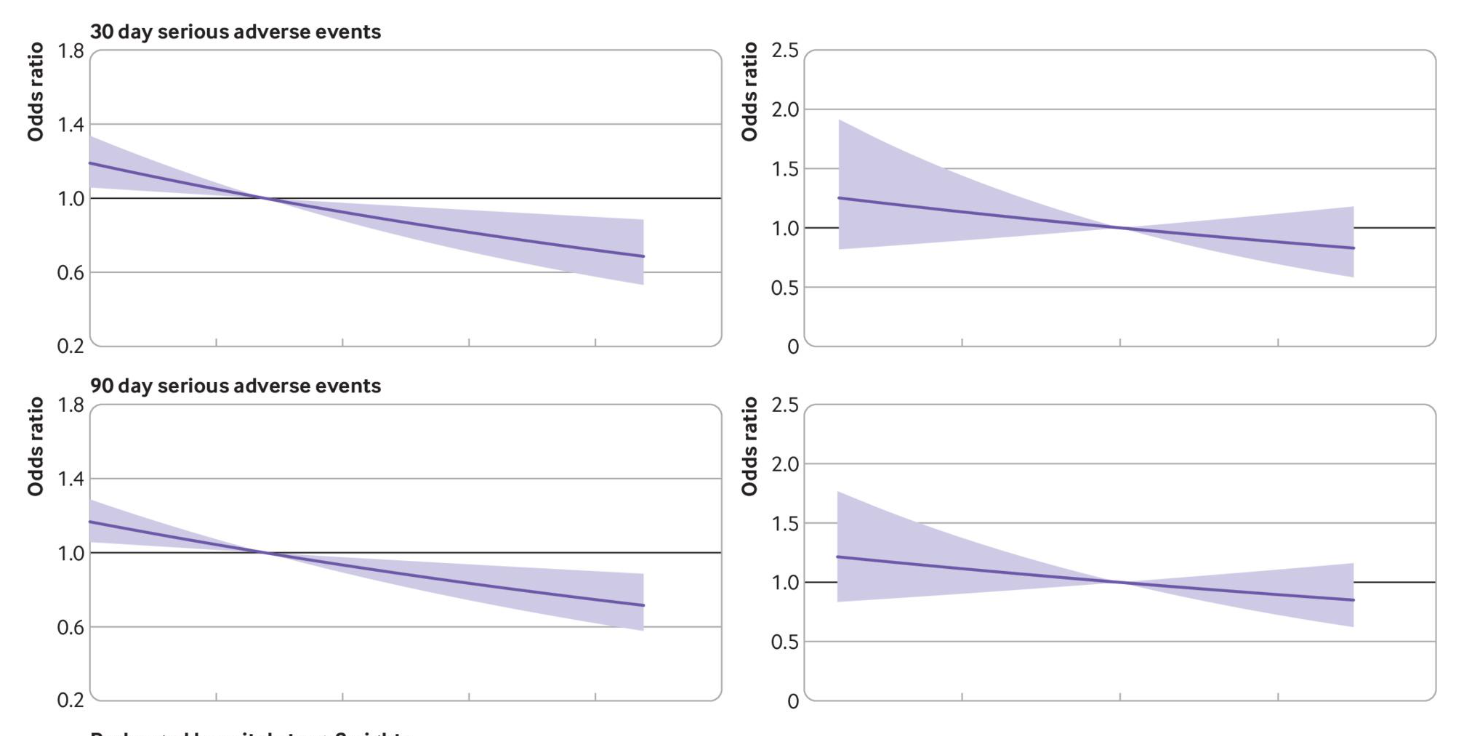
The study found that surgeons who clocked in more than 10.4 shoulder replacements per year had better patient outcomes. We're talking lower rates of revision surgery and reoperation, fewer serious adverse events, and shorter hospital stays. The takeaway? The more surgeries a surgeon performed, the better the outcomes for their patients.
So, what's the scoop for us? It's a nudge about the power of experience and the value of sharpening our skills through repetition. Whether we're talking rhinoplasty or breast reconstruction, the principle holds: the more we do, the better we get.
But it's not just about us leveling up. It's about our patients leveling up, too. Shorter hospital stays and fewer adverse events mean a smoother recovery process and a better overall experience for our patients. And that's the real win, isn't it?

I'm curious to hear your thoughts on this. Are you seeing a similar trend in your practice? Is there a 'magic number' of surgeries that we, as plastic and reconstructive surgeons, should be aiming for each year? Hit reply and let P'Fella in on your thoughts.
Until next time, keep practicing, keep perfecting, and keep making a difference.
Lots of love, P'Fella ❤️
The Sunday Quiz
Classifying Osteoarthritis
New and Upcoming
Educational Tools, Events & Courses
4 Upcoming Events
- World Reconstructive Microsurgery - 18th August
- ASSH Annual Meeting - Toronto, 5th October
- Plastic Surgery - The Meeting: Texas, 26th Oct
- BAPRAS Congress - 29th Nov
Image of the Week
AI-generated clinical images
Tweets of the Week
Don't forget to follow P'Fella!
Blood gas when coming down from the summit of Everest. 😳 #TC2023 @Anaes_Trainees pic.twitter.com/yVbVMUOBMw
— Emily (@dr_doddle) July 7, 2023
I hope people’s takeaway message from recent medtwitter stories about mistakes, shortening medical school, and overall expertise is that medicine is quite difficult, actually. And we all should be campaigning for maximising training, not seeking the minimal viable product model.
— Medlife Crisis (Rohin) (@MedCrisis) July 8, 2023
🧵regarding 'the crimp' and other technical pointers having to do with securing surgical drains with suture.
— Ron Barbosa MD FACS (@rbarbosa91) July 6, 2023
We'll go over my preferred method, other methods like the Roman sandal, some errors people make, and other factoids.
(1/ ) pic.twitter.com/2nTB41hOuC
Ask P'Fella
You ask, I'll answer
How long your observe a keratoacanthoma ?
Keratoacanthomas, they can be a bit of a headache. You gotta make sure the diagnosis is spot on. Mistaking them for something else might lead you to misdiagnose a high-risk skin cancer called SCC. So, these Keratoacanthomas grow pretty fast, like a few weeks fast, mainly on sun-exposed skin. You can spot them by their central crater filled with a "keratin plug".
Now, if you've got a patient with a classic Keratoacanthoma, I'd schedule a follow-up in about 6 weeks. If the spot hasn't started to shrink by then, it's time to dig deeper with a biopsy for a clearer diagnosis.
You might wonder, "Why not just remove it at first sight?" Well, it's not that simple. Under the microscope, Keratoacanthomas and SCCs look pretty much the same, making them hard to tell apart. So, if you remove a Keratoacanthoma thinking it's an SCC, the patient may end up with unnecessary lifelong check-ups per SCC guidelines.
If you want to dive deeper into the nitty-gritty of these things, like the challenges in identifying them under the microscope, how they behave over time, and when they appear, there's plenty of reading material out there.
3 questions submitted in the last 24 hours...
Articles of the Week
3 must-read articles, 1 deep-dive! 📚
3 Must-reads
- When is "metal" risky in finger fractures?
Grisdela et al. Factors Associated With Implant Removal Following Plate-and-Screw Fixation of Isolated Metacarpal Fractures. J Hand Surg Am. 2023 - When can I go back to sport? UCL injuries
Allahabadi et al. Return to Play After Thumb Ulnar Collateral Ligament Injuries Managed Surgically in Athletes-A Systematic Review. J Hand Surg Glob Online. 2023 - Orthoplastic protocols actually work.
Ylitalo et al. Implementing an orthoplastic treatment protocol for open tibia fractures reduces complication rates in tertiary trauma unit. Injury. 2023
How should we treat Mallet Fingers?
Uncover the intriguing journey from Mallet Finger Fractures to osteoarthritis in this riveting study! Despite a surprising twist of high OA incidence and diminished mobility post non-surgical treatment, the patient-reported outcomes surprisingly remain minimally affected - an unexpected plot twist that keeps you on the edge of your seat!


