In this Journal Club
5-Point Summary
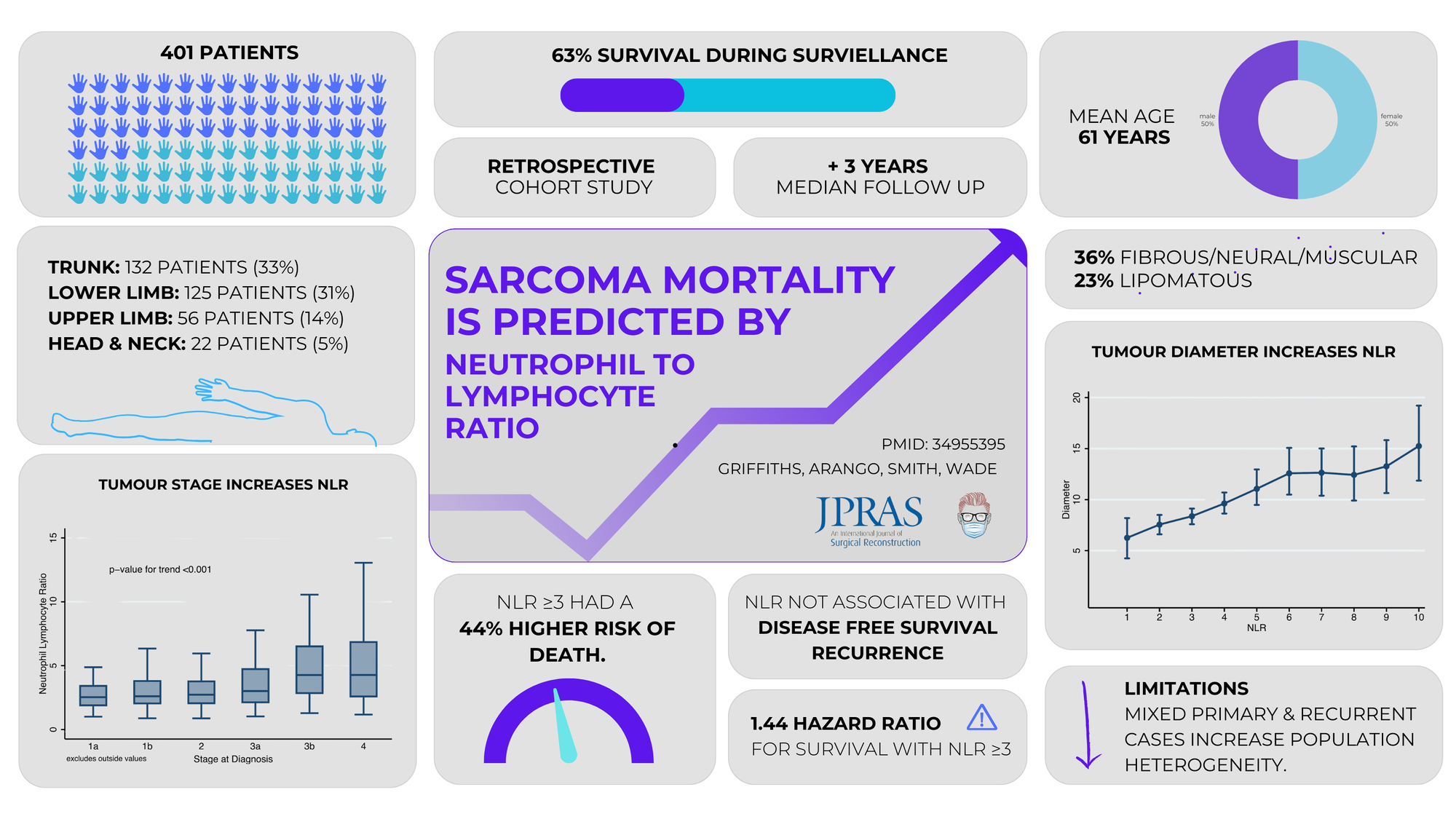
401 patients, NLR ≥3 predicts poorer survival, not recurrence, aids risk stratification & treatment planning.
4-Key Findings
Elevated NLR reduces survival, links to tumor size and stage, has no link with recurrence, and histological subtype impacts survival.
3-Critiques
Lack of adjustment for co-morbidities, cohort heterogeneity from recurrent tumuors, unclear link between NLR and recurrence
2-Practical Takeaways
Use NLR for identifying high-risk patients and guide closer monitoring for elevated NLR.
1-Recommended Reading
Szkandera J. et al. (Br J Cancer, 2013) found elevated preoperative NLR predicts poor prognosis in STS, reinforcing its prognostic role.
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur. Excepteur sint occaecat cupidatat non proident, sunt in culpa qui officia deserunt mollit anim id est laborum
5 Point Summary
Baseline NLR predicts overall survival in extremity STS, with higher NLR linked to worse survival. Useful for identifying high-risk patients.
1️⃣ Hypothesis
Baseline neutrophil-lymphocyte ratio predicts overall survival in extremity soft-tissue sarcoma (STS).
2️⃣ Method
17-year retrospective study of 401 adults. Preoperative NLR tests analysed with multivariable Cox regression.
3️⃣ Results
NLR ≥3 linked to poorer overall survival but not disease-free survival or recurrence.
4️⃣ Conclusion
NLR predicts survival in STS, aiding risk stratification & treatment planning
5️⃣ Implication
High NLR identifies patients needing aggressive therapy and monitoring.
4 Key Findings
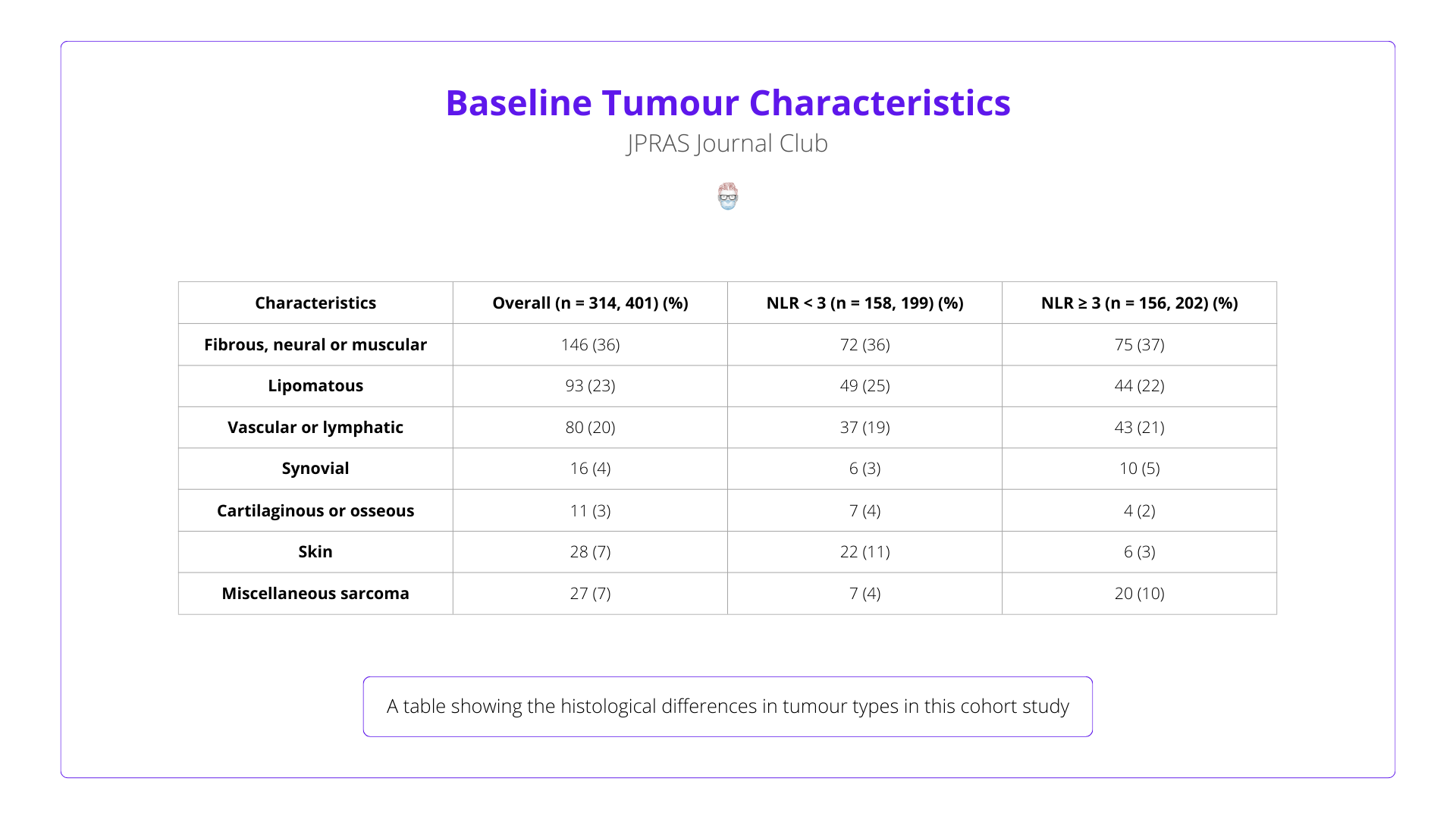
Elevated NLR reduces survival, links to tumor size and stage, has no link with recurrence, and histological subtype impacts survival.
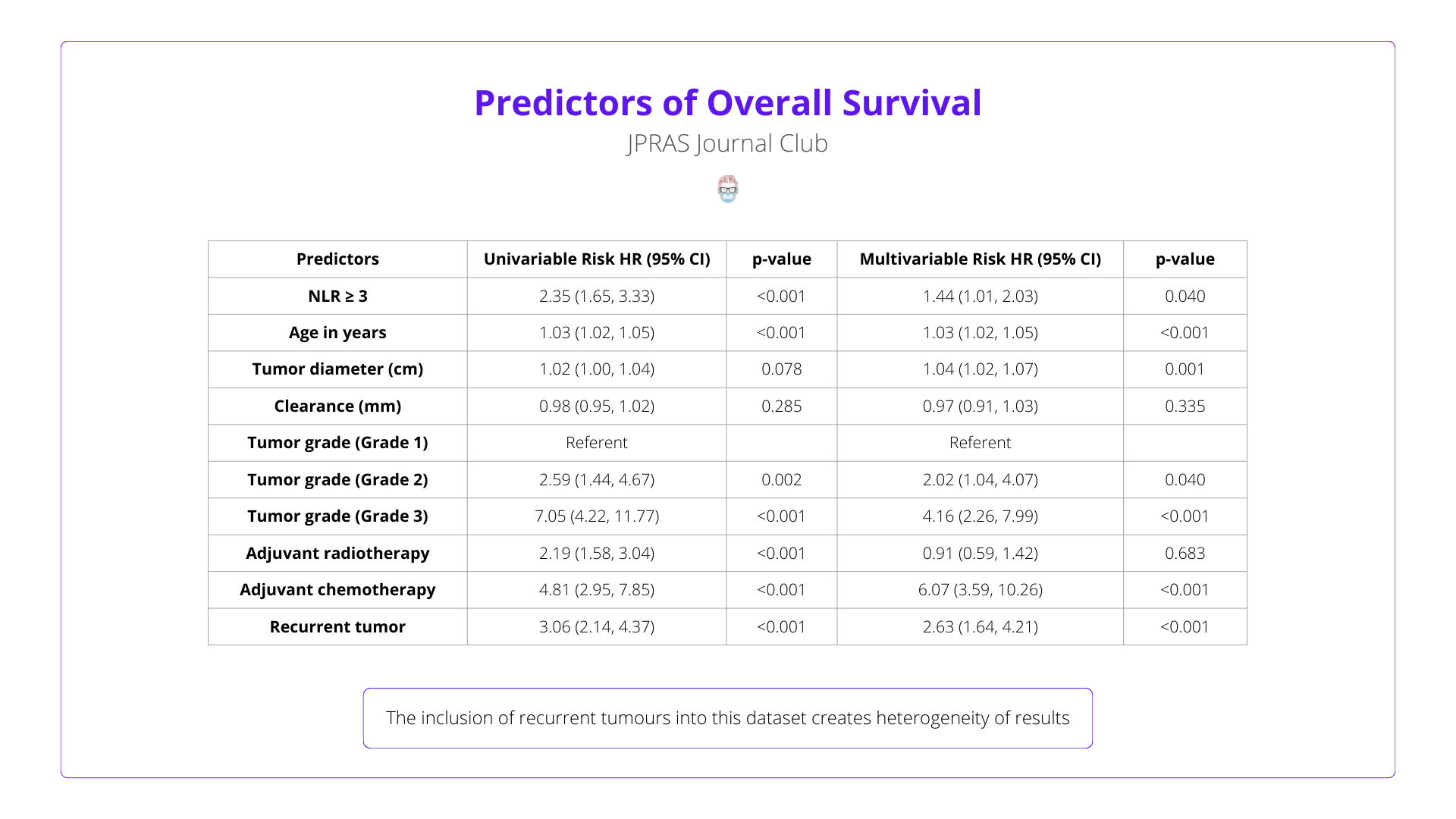
Elevated NLR (≥3) independently predicts reduced survival (HR 1.44; 95% CI 1.01–2.03), even after adjusting for age, tumor size, and grade.
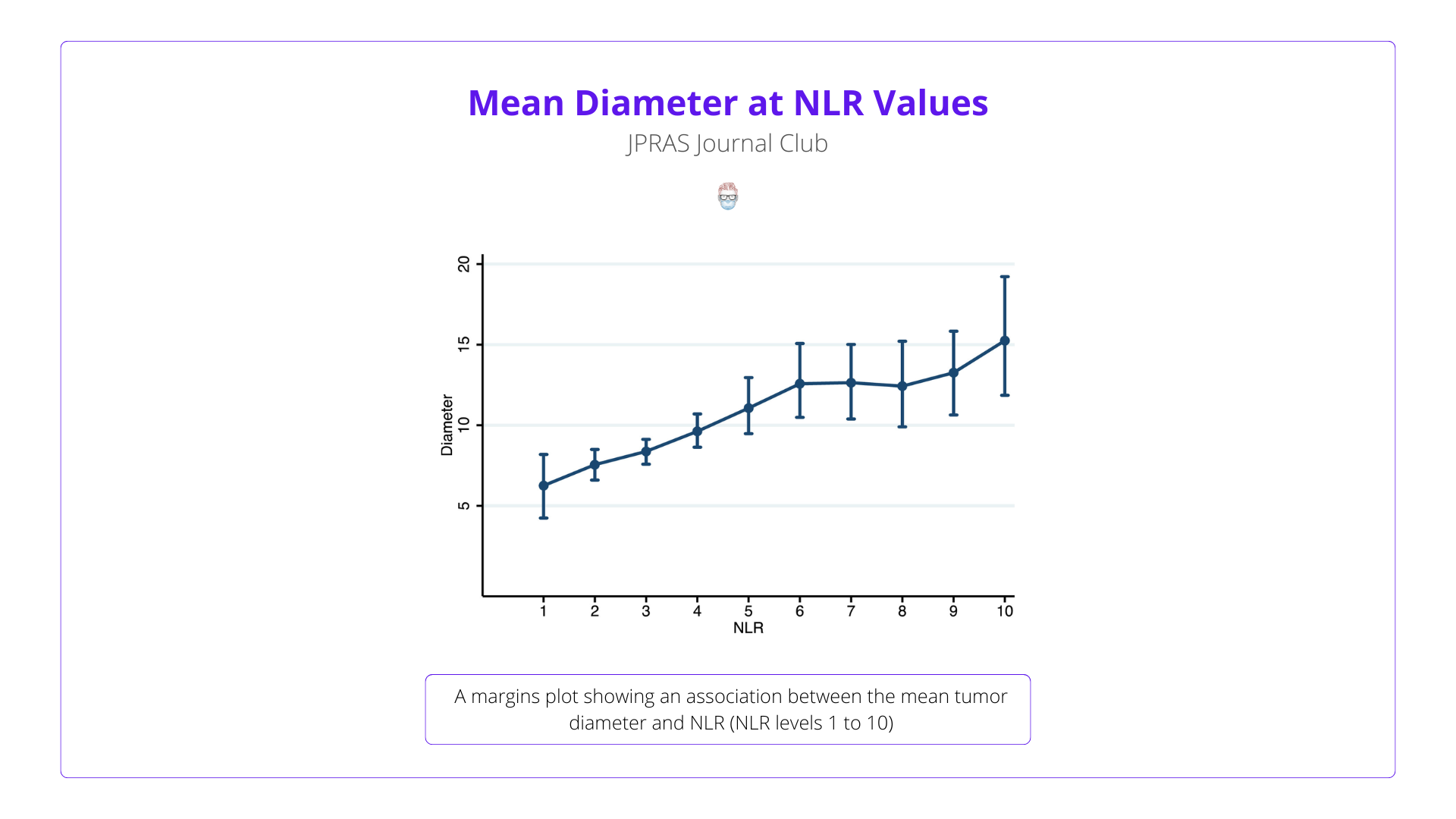
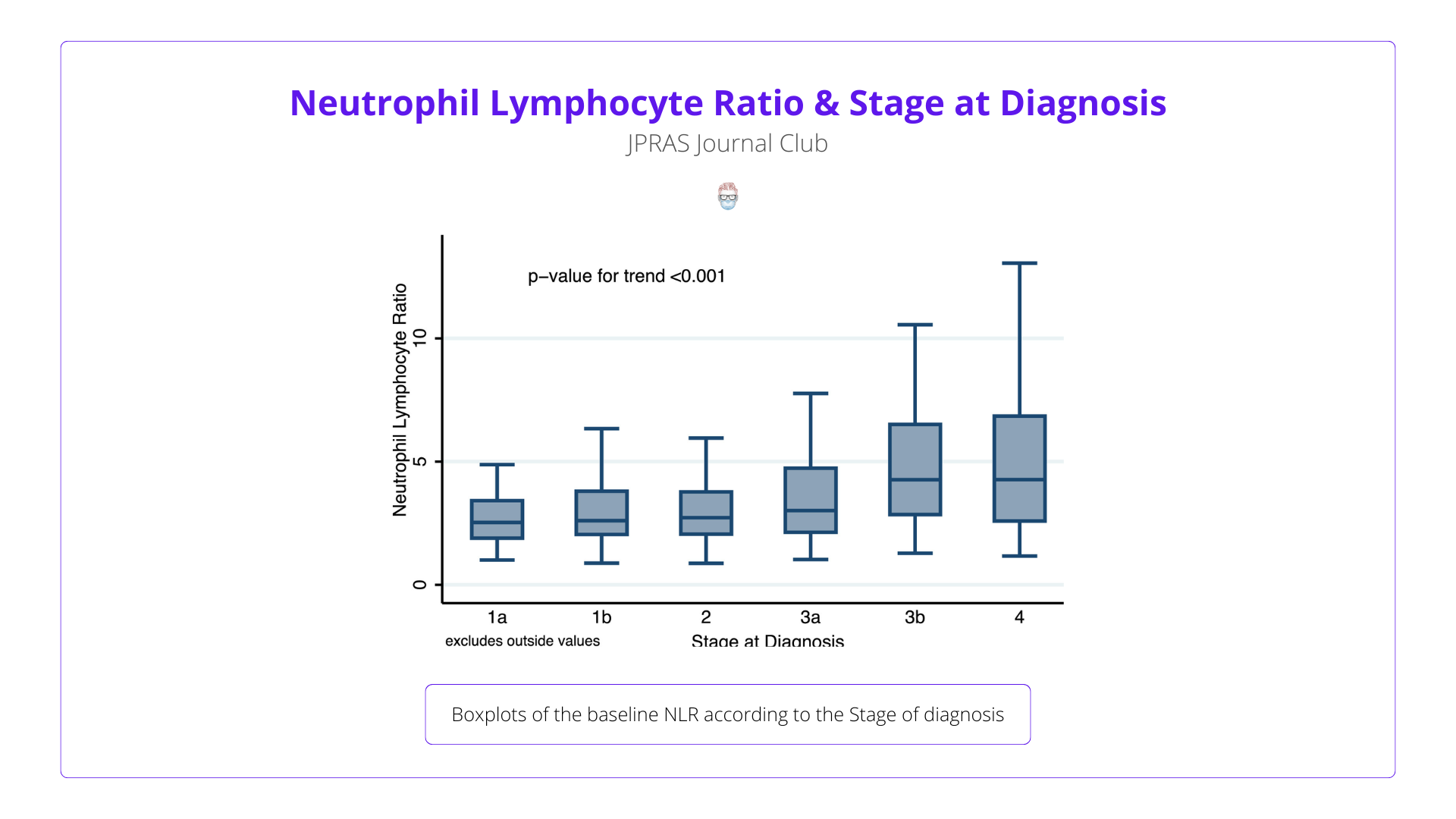
Higher NLR correlates with larger tumors and advanced stages, reflecting systemic inflammation and tumor aggressiveness.
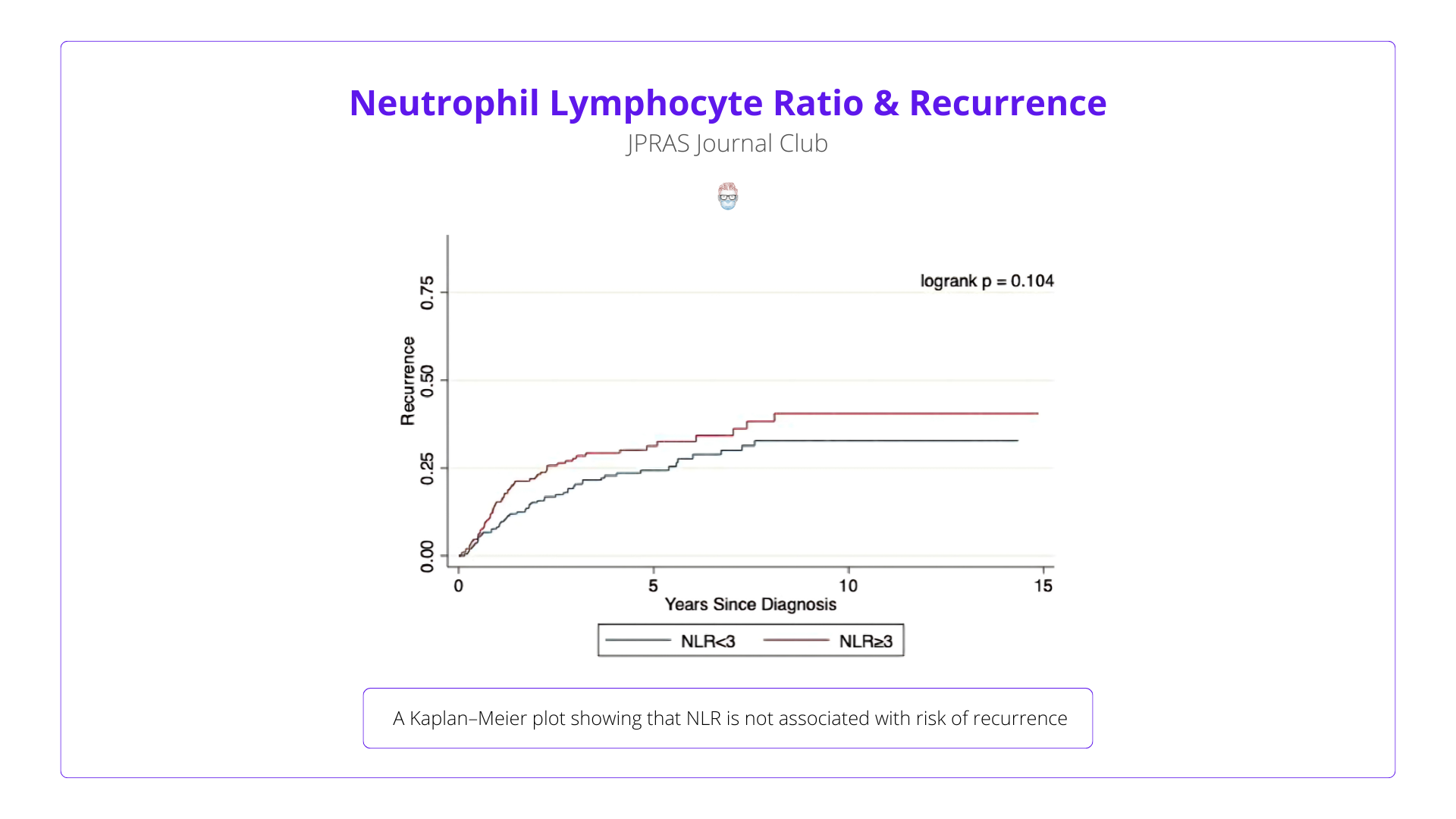
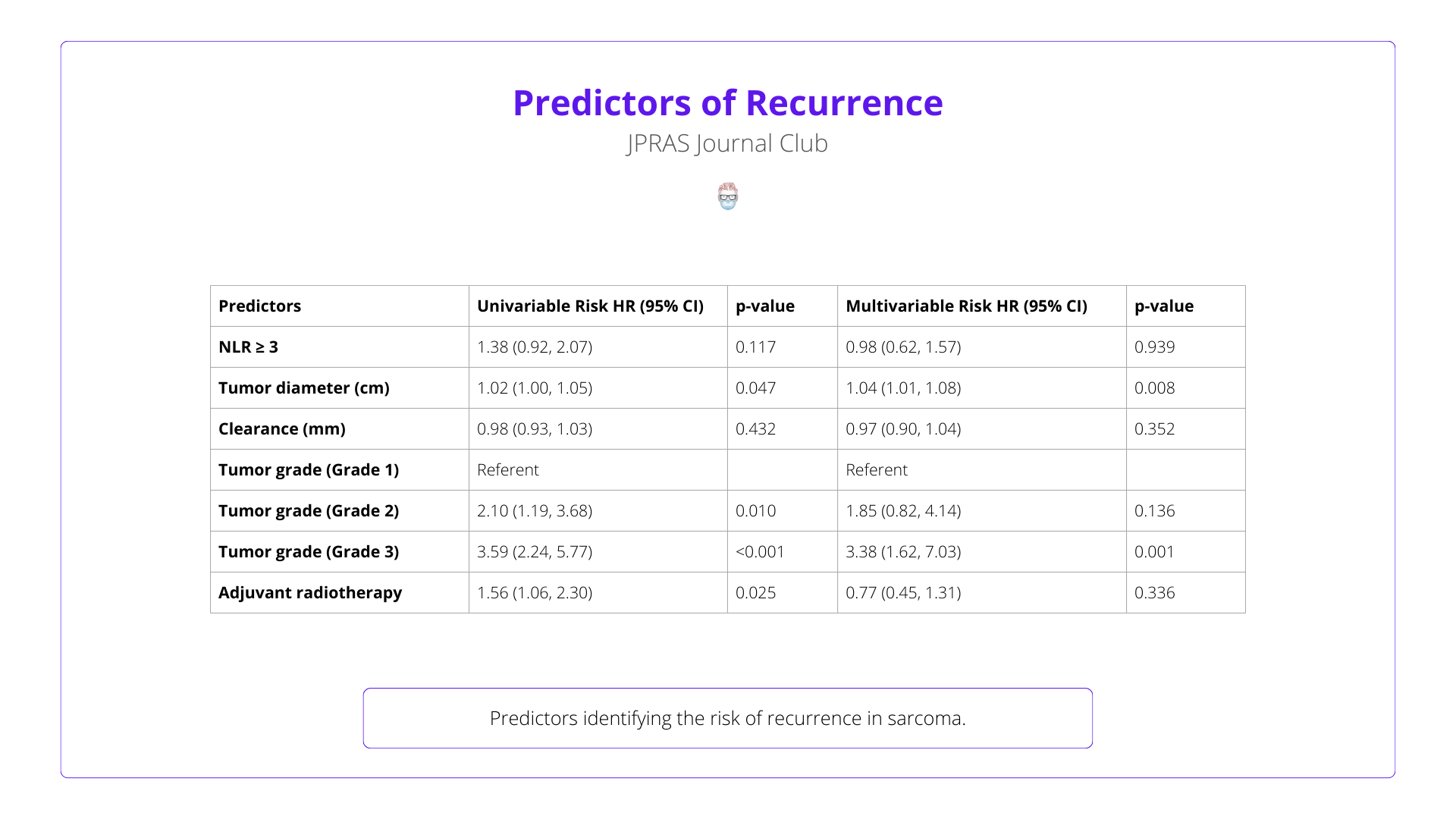
NLR did not significantly predict recurrence or disease-free survival after adjustment, limiting its utility to mortality prediction.
Patients with lipomatous sarcomas had better survival regardless of NLR, emphasising the role of tumour biology.
3 Critiques
Lack of adjustment for comorbidities, cohort heterogeneity from recurrent tumors, unclear link between NLR and recurrence
Key factors like diabetes and performance status were not adjusted for, potentially influencing both NLR and survival. Future studies should address these to confirm NLR's independent role.
Including primary and recurrent STS cases may have diluted outcome associations. Separate analyses could yield clearer insights.
While NLR predicts overall survival, its lack of association with recurrence raises questions about its relevance to STS progression, warranting further study.
2 Practical Takeaways
Use NLR for identifying high-risk patients and guide closer monitoring for elevated NLR.
High NLR can guide closer post-treatment monitoring to detect disease progression early.
Elevated NLR identifies high-risk STS patients who may benefit from tailored neoadjuvant or adjuvant therapies to improve survival.
1 Recommended Reading
Szkandera J. et al. (Br J Cancer, 2013) found elevated preoperative NLR predicts poor prognosis in STS, reinforcing its prognostic role.
Read the Article

