In this week's edition
- ✍️ Letter from P'Fella
The shadow economy of plastic surgery is booming. - 🤓 The Sunday Quiz
How well do you know venous flaps? - 🖼️ Image of the Week
ALT musculocutaneous perforator flap in action. - 🚑 Technique Tip
How to do Allen’s patency test. - 📖 What Does the Evidence Say
Vasopressors in microsurgery: Challenging the dogma. - 🔥 Articles of the Week
CT Angio before DIEP, why flaps fail, & microsurgical principles: with 1 sentence summaries. - 💕 Feedback
Suggest ideas & give feedback!
A Letter from P'Fella
The Shadow Economy of Plastic Surgery is Booming
Let’s call this what it is: We’ve built a system that’s broken and hypocritical.
In an attempt to reduce stress and level the playing field, medical schools moved away from traditional grades and honors to a pass/fail setup. But instead of fixing the problem, we just shifted the battlefield.
Now, students are forced into a shadow economy of extracurricular effort to survive an arms race that does nothing to make them better doctors. They’re churning out abstracts, stacking volunteer experiences, and competing on a spreadsheet — not in the clinic, where it actually matters.
Eric Warm’s post on Twitter brought this to my attention.

And here’s the dirty truth: None of this insanity predicts who will excel in residency.
The Reality
In 2022, neurosurgery applicants averaged 30 publications per person. The top 10% submitted 58 or more. For perspective, that’s more than what many full-time academics publish in years. And this isn’t just isolated to the ultra-competitive specialties — plastic surgery is no different. Students are gaming the system because we’ve left them no choice.
We’ve replaced grades with meaningless metrics and called it progress. The result? Students are ditching clinical teaching, their hands-on skills are deteriorating, and burnout is now baked into the process before residency even begins.
What We’re Really Doing
This pass/fail era creates triple harm.
- Clinical Excellence is Devalued: Students are rewarded for looking good on paper, not for being great in practice.
- Burnout is Accelerating: The bar is impossibly high. Even the strongest students are crumbling under the pressure.
- Superficial Academia is Thriving: “Achievements” like mass-producing abstracts aren’t about quality or learning — they’re strategic resume padding.
A System That Eats Its Young
Sure, some students feel liberated to pursue meaningful work under pass/fail — but let’s not kid ourselves. Most are just trying to survive. This is not the meritocracy we claim it to be; it’s a system that eats its young and wonders why they’re burnt out by Day 1 of residency.
P'Fella ❤️
The Sunday Quiz
How Well Do You Know Venous Flaps?
Welcome to the last round of The Weekly Quiz.
Each edition of thePlasticsPaper includes a quiz question designed to challenge and engage our readers. Keep your wits about you and join in every week — the winner at the end of six rounds will earn you a one-year subscription to thePlasticsPro.
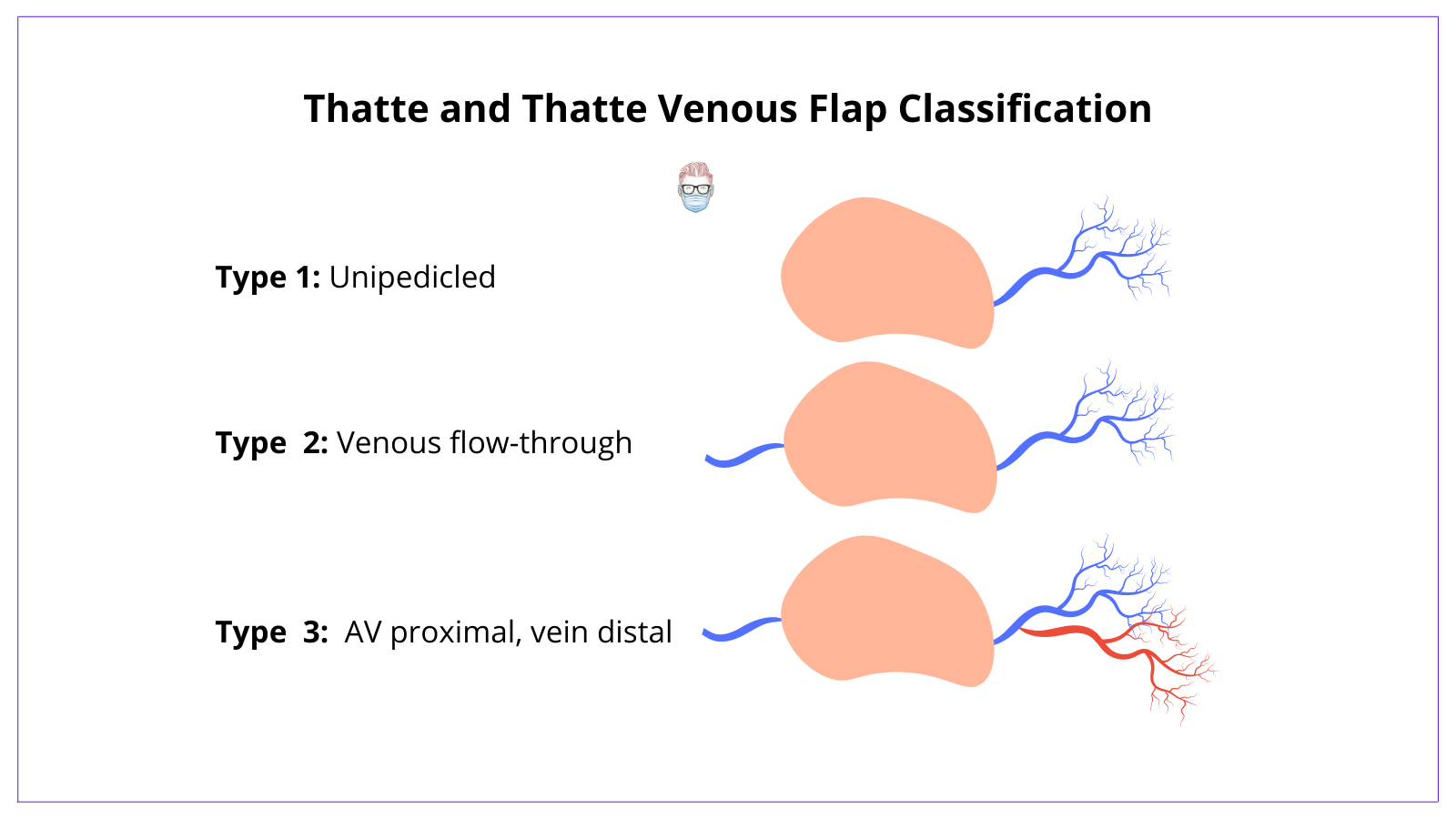
Image of the Week
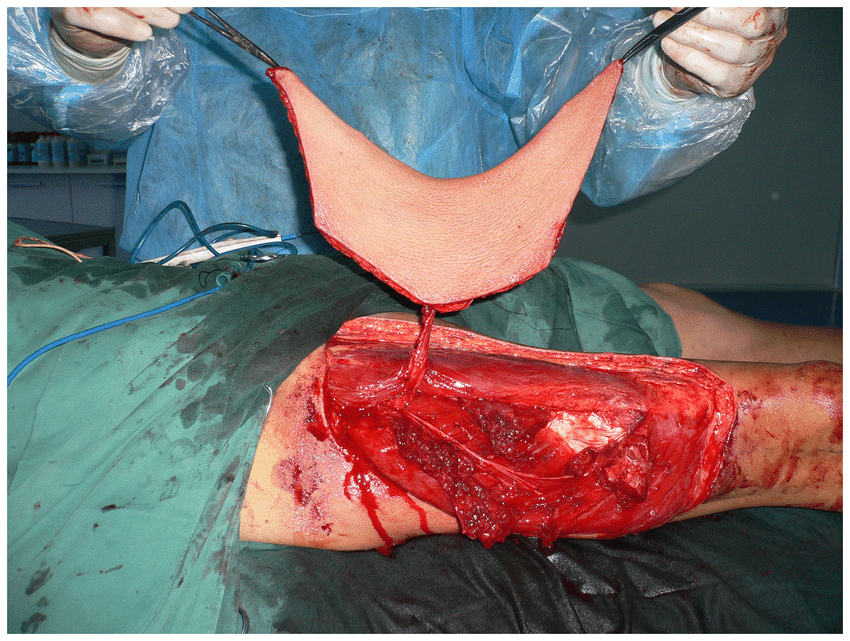
ALT Musculocutaneous Perforator Flap in Action
In this section, we feature an anatomical illustration. This week, we’re looking at an intraoperative image of an elevated ALT musculocutaneous perforator flap with the deep fascia.
Read more about the anterolateral thigh flap here.
Technique Tip
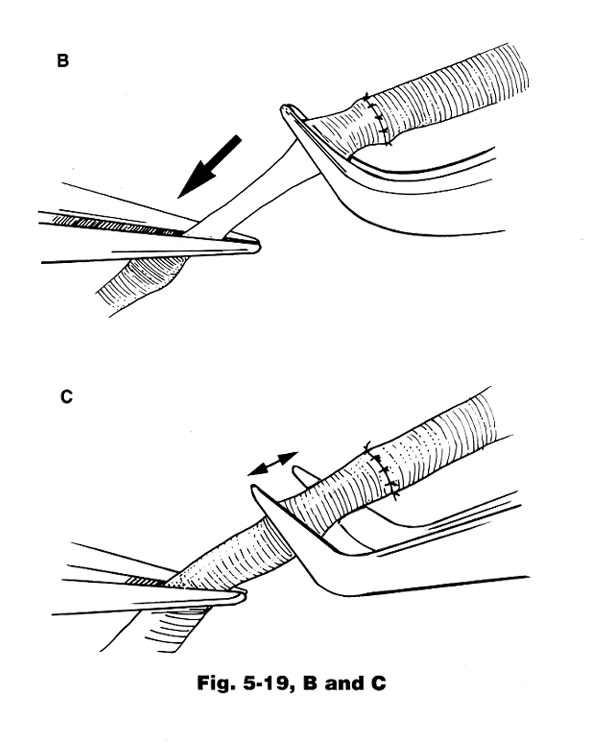
How to Do A Patency Test
This week’s technique focuses on Patency Test, a useful but minimally traumatic method to assess vessel patency. Use it judiciously to avoid unnecessary vessel trauma.
Steps:
1. Occlude the vessel distal to the anastomosis with forceps.
2. Use a second pair of forceps to empty a segment of the vessel.
3. Release the proximal forceps and watch for segment refill.
Tips:
- Use forceps with parallel jaws for reliable occlusion.
- Perform the test distal to the anastomosis and follow the natural blood flow direction for accuracy.
What Does the Evidence Say?
Vasopressors in Microsurgery: Challenging the Dogma
Noradrenaline use did not adversely affect free flap survival in microvascular reconstructive surgeries (Rajan et al., 2019). Various vasopressors, including phenylephrine, ephedrine, and calcium chloride, have been safely used in different surgical phases without increasing flap compromise or failure rates (Fang et al., 2017). While some studies noted a slightly higher re-exploration rate with vasopressor use, overall flap outcomes remained unaffected (Rajan et al., 2019).
The judicious use of vasopressors in microsurgery may be safe and potentially beneficial for maintaining hemodynamic stability without compromising flap viability.
Articles of the Week
3 Interesting Articles with 1 Sentence Summaries
In DIEP flap breast reconstruction, preoperative CT-angiography significantly reduces both flap loss and operative time compared to Doppler ultrasound.
microvascular free flaps show a 4.4% failure rate, with operative time exceeding 625 minutes identified as a significant independent risk factor.
Reconstructive microsurgery has evolved from free flap techniques to advanced procedures such as limb transplantation as its key principles continue to shape complex reconstructions.


