Summary Card
Definition
A glomus tumour is a benign lesion from glomus cells in the Sucquet-Hoyer canal, typically on the nail bed or palm.
Classification
The glomus body, aiding thermoregulation and common in the finger dermis, can develop benign hamartomas called glomus tumours.
Diagnosis
A glomus tumour typically presents with fingertip pain, tenderness, cold sensitivity, and nail changes, diagnosed through clinical tests, imaging (US and MRI), and histology.
Management
Complete excision of glomus tumours is advised for pain relief and to reduce recurrence; laser or sclerotherapy is recommended for multiple, inoperable lesions.
Primary Contributor: Dr Kurt Lee Chircop, Educational Fellow.
Reviewer: Dr Waruguru Wanjau, Educational Fellow.
Definition of Glomus Tumours
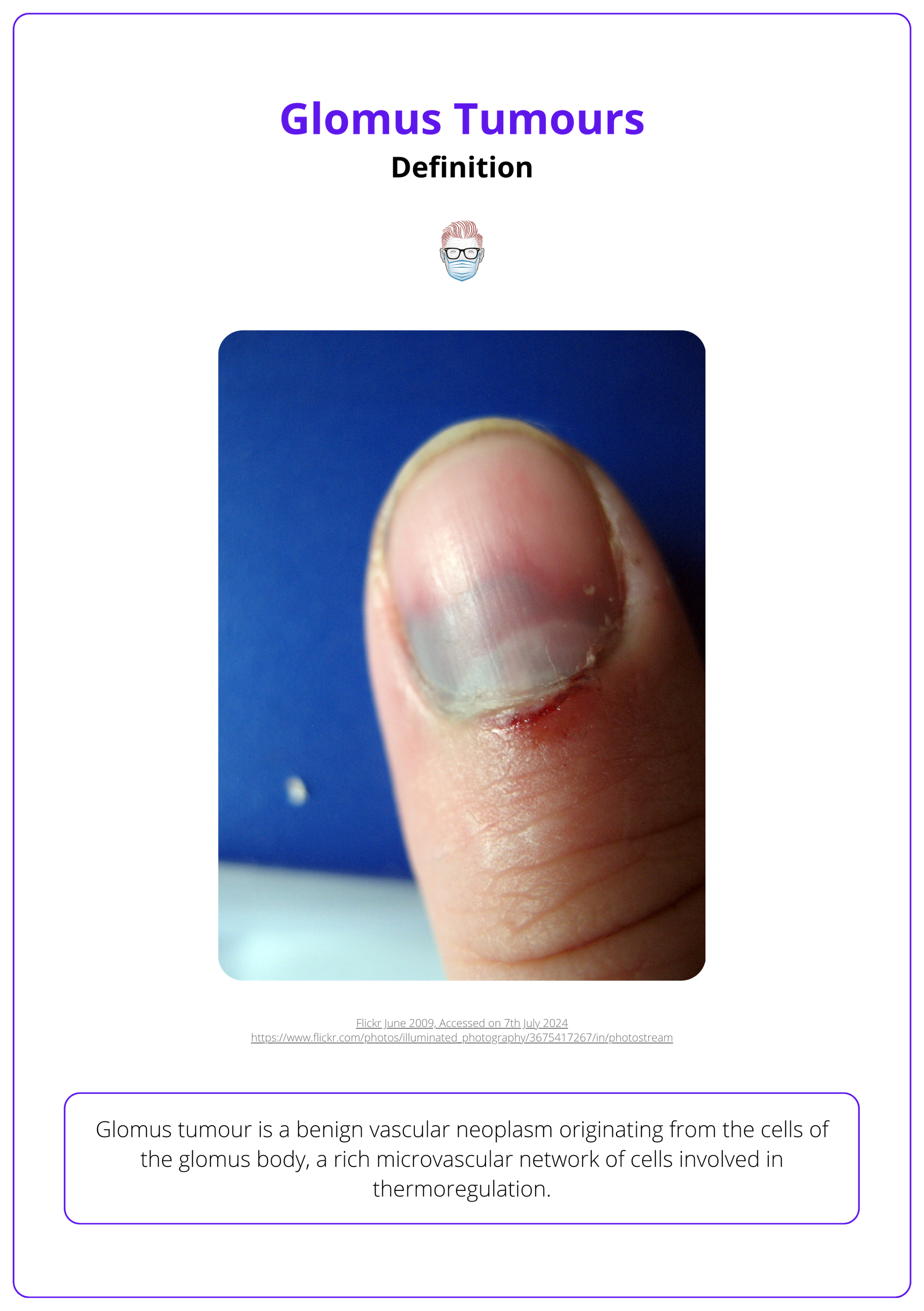
Glomus tumour is a benign vascular neoplasm originating from the cells of the glomus body, a rich microvascular network of cells involved in thermoregulation.
Glomus tumours are described as benign hamartomas of the glomus apparatus, originating from modified smooth muscle cells of the Sucquet-Hoyer canal (Morey, 2016). Demographic analysis shows:
- 1 to 5% of all hand tumours, usually in the subungual region.
- More common in females.
- Usually occurs between the 2nd-5th decade (Trehan, 2015).
Extradigital glomus tumours show equal distribution between the genders (Chou, 2016).
A glomus tumour is illustrated in the image below.
The glomus body, in the finger's reticular dermis, regulates skin temperature and includes an afferent arteriole, Sucquet-Hoyer canal, primary collecting vein, and intraglomerular reticulum.
Classification of Glomus Tumours
The WHO classifies glomus tumors into three types: solid glomus tumors (glomus cells), glomangiomas (vascular cells), and glomangiomyomas (vascular and smooth muscle cells).
WHO Classification
The World Health Organization (WHO) classifies glomus tumours according to the predominance of glomus cells, vascular structures, and smooth muscle cells into 3 distinct entities (Sethu, 2016):
- Solid glomus tumours: Most common, with a predominance of glomus cells.
- Glomangioma: With a predominance of vascular cells.
- Glomangiomyoma: With a predominance of both vascular and smooth muscle cells.
Benign vs. Malignant Glomus Tumors
Glomus tumors are typically benign, but they can occasionally transform into malignant forms or arise as malignant glomus tumors, known as glomangiosarcomas.
These malignant lesions have a high rate of local recurrence but a very low rate of metastasis. Risk factors for malignancy include:
- Deeper location
- Size greater than 2 cm
- Rapid growth
- Atypical mitosis
- High pathological grade
A familial variant of glomus tumour has been associated with chromosome 1p21–22 and involves truncating mutations in the glomulin gene (Brouillard, 2002).
Diagnosis of Glomus Tumours
Glomus Tumours usually exhibit a triad of symptoms: sharp pain in the fingertips, pinpoint tenderness, and heightened sensitivity to cold. It can be confirmed on ultrasound or MRI.
Clinical Assessment
Glomus tumors typically present as small (<2 cm), solitary lesions in the acral regions, often subungual. They appear as blue or red blanchable papules or nodules in the deep dermis or subcutis. Multiple tumors may be present in up to 10% of cases (Sethu, 2016)
Typical Symptoms (Chou, 2016):
- Stabbing pain in the fingertips
- Pinpoint tenderness
- Cold hypersensitivity
Diagnostic Signs (Tang, 2013):
- Love’s Maneuver: Pinpoint pressure applied to the nail elicits pain using a fine needle.
- Hildreth’s Sign: Pain and pinpoint tenderness reduce with proximal inflation of a tourniquet, causing transient ischemia.
Subungual glomus tumors can cause nail changes such as ridging, erythronychia, splitting, and thickening. Any subungual nodule that alters nail color or structure should raise suspicion for a glomus tumor (Lu, 2018).
Glomus tumours are rare outside the fingers, with case reports noting occurrences in the gastrointestinal tract, mediastinum, trachea, mesentery, cervix, and vagina (Chou, 2010 & Filice, 2008 & Almaghrabi, 2017).
Imaging
- Ultrasound: detection of lesions as small as 3mm, and helps with depth assessment (Matsunaga, 2007).
- MRI: Tumours show a high signal intensity on T2-weighted and STIR images (Drape, 1996).
Histology
Glomus tumor cells have round to oval nuclei, pale eosinophilic cytoplasm, distinct borders, and minimal mitotic activity & pleomorphism. They are immunoreactive for αSMA, MSA, and h-caldesmon, and contain type IV collagen. These markers distinguish glomus tumors from hemangiomas and S100-positive paragangliomas (Mravic, 2015).
Type I neurofibromatosis is associated with glomus tumors, showing similar sex distribution, tumor location, and burden as isolated glomus tumors (Harrison, 2014).
Differential Diagnosis
Benign and malignant lesions can resemble glomus tumors. The most common tumor presenting similarly is an epithelial inclusion cyst. Initially thought to be a subset of glomus tumors, it can be distinguished by the following characteristics:
- Prominent vascular components with dilated vessels, possible thrombosis, and phlebolith formation
- Positive for epithelial markers with focal ductal differentiation
- Naevus cells positive for S100 and Melan-A, unlike glomus tumors
Other tumors to consider include:
- Blue Naevus: Rare in the subungual region but may cause diagnostic uncertainty.
- Angioleiomyoma
- Dermatologic Manifestation of Kaposi Sarcoma
- Glomangioma: More common in children and adolescents, typically multifocal, hereditary, and generally painless (Boon, 2004).
Management of Glomus Tumours
Complete excision is advised for solitary glomus tumours to alleviate pain and prevent recurrence, with varied techniques for different locations and low recurrence rates if completely excised.
Solitary Glomus Tumours
For solitary glomus tumours, complete removal of the tumour capsule is advised to alleviate pain and reduce the risk of recurrence.
Most subungual lesions are treated by removing the entire nail and excising the tumour, though other techniques include:
- Excision via the nail bed margin
- The trap-door method
- A nail-conserving technique by Lee et al (Pahwa, 2010).
In the transungual approach, the nail plate is removed, the tumour is excised, and the nail bed is repaired.
Multiple Glomus Tumours
For multiple glomus tumours, excision is challenging due to poor circumscription and numerous lesions, making laser therapy (argon, CO2, Nd) and sclerotherapy more effective options (Gould, 1991).
These tumours have a low incidence of recurrence if completely excised.
Conclusion
1. Basic Characteristics of Glomus Tumors: You've gained a foundational understanding of glomus tumors, including their origin from glomus cells, typical locations, and the severe pain they can cause.
2. Pathology and Classification: You are now familiar with the components of the glomus body, the classification of glomus tumors into different types based on cell predominance, and the potential for malignant transformation.
3. Diagnostic Techniques: You've recognized the importance of clinical examination, imaging techniques like ultrasound and MRI, and histology in diagnosing glomus tumors.
4. Management Strategies: You've learned that complete surgical excision is the preferred treatment for solitary tumors to alleviate pain and prevent recurrence, and alternative therapies like laser or sclerotherapy for multiple lesions.
5. Complications and Outcomes: Understanding potential complications and outcomes of treatment for better preparation and management of patient expectations regarding glomus tumors.
Further Reading
- Morey, Vivek Machhindra, Bhavuk Garg, and Prakash P. Kotwal. "Glomus tumours of the hand: review of literature."Journal of clinical orthopaedics and trauma 7.4 (2016): 286-291.
- Trehan, S. K., Soukup, D. S., Mintz, D. N., Perino, G., & Ellis, S. J. (2015). Glomus Tumors in the Foot: Case Series. Foot & ankle specialist, 8(6), 460–465. https://doi.org/10.1177/1938640015583514
- Chou, T., Pan, S. C., Shieh, S. J., Lee, J. W., Chiu, H. Y., & Ho, C. L. (2016). Glomus Tumor: Twenty-Year Experience and Literature Review. Annals of plastic surgery, 76 Suppl 1, S35–S40. https://doi.org/10.1097/SAP.0000000000000684
- Chou, H. P., Tiu, C. M., Chen, J. D., & Chou, Y. H. (2010). Glomus tumor in the stomach. Abdominal imaging, 35(4), 390–392. https://doi.org/10.1007/s00261-009-9552-5
- Filice, M. E., Lucchi, M., Loggini, B., Mussi, A., & Fontanini, G. (2008). Glomus tumour of the lung: case report and literature review. Pathologica, 100(1), 25–30.
- Almaghrabi, A., Almaghrabi, N., & Al-Maghrabi, H. (2017). Glomangioma of the Kidney: A Rare Case of Glomus Tumor and Review of the Literature. Case reports in pathology, 2017, 7423642. https://doi.org/10.1155/2017/7423642
- Sethu, C., & Sethu, A. U. (2016). Glomus tumour. Annals of the Royal College of Surgeons of England, 98(1), e1–e2. https://doi.org/10.1308/rcsann.2016.0005
- Mravic M, LaChaud G, Nguyen A, Scott MA, Dry SM, James AW. Clinical and histopathological diagnosis of glomus tumor: an institutional experience of 138 cases. Int J Surg Pathol. 2015 May;23(3):181-8. doi: 10.1177/1066896914567330. Epub 2015 Jan 22. PMID: 25614464; PMCID: PMC4498398.
- De Chiara A, Apice G, Mori S, Silvestro G, Losito SN, Botti G, Ninfo V. Malignant glomus tumour: a case report and review of the literature. Sarcoma. 2003;7(2):87-91. doi: 10.1080/1357714031000081207. PMID: 18521375; PMCID: PMC2395518.
- Harrison, B., & Sammer, D. (2014). Glomus tumors and neurofibromatosis: a newly recognized association. Plastic and reconstructive surgery. Global open, 2(9), e214. https://doi.org/10.1097/GOX.0000000000000144
- Brouillard P, Boon LM, Mulliken JB, Enjolras O, Ghassibé M, Warman ML, Tan OT, Olsen BR, Vikkula M. Mutations in a novel factor, glomulin, are responsible for glomuvenous malformations ("glomangiomas"). Am J Hum Genet. 2002 Apr;70(4):866-74. doi: 10.1086/339492. Epub 2002 Feb 13. PMID: 11845407; PMCID: PMC379115.
- Lu, H., Chen, L. F., & Chen, Q. (2018). Rupture of a subungual glomus tumor of the finger. BMC cancer, 18(1), 505. https://doi.org/10.1186/s12885-018-4377-7
- Tang CY, Tipoe T, Fung B. Where is the Lesion? Glomus Tumours of the Hand. Arch Plast Surg. 2013 Sep;40(5):492-5. doi: 10.5999/aps.2013.40.5.492. Epub 2013 Sep 13. PMID: 24086799; PMCID: PMC3785579.
- Matsunaga, A., Ochiai, T., Abe, I., Kawamura, A., Muto, R., Tomita, Y., & Ogawa, M. (2007). Subungual glomus tumour: evaluation of ultrasound imaging in preoperative assessment. European journal of dermatology : EJD, 17(1), 67–69. https://doi.org/10.1684/ejd.2007.00190
- Drapé, J. L., Idy-Peretti, I., Goettmann, S., Guérin-Surville, H., & Bittoun, J. (1996). Standard and high resolution magnetic resonance imaging of glomus tumors of toes and fingertips. Journal of the American Academy of Dermatology, 35(4), 550–555. https://doi.org/10.1016/s0190-9622(96)90678-7
- Boon LM, Mulliken JB, Enjolras O, Vikkula M. Glomuvenous malformation (glomangioma) and venous malformation: distinct clinicopathologic and genetic entities. Arch Dermatol. 2004 Aug;140(8):971-6. doi: 10.1001/archderm.140.8.971. PMID: 15313813.
- Lee, H. J., Kim, P. T., Kyung, H. S., Kim, H. S., & Jeon, I. H. (2014). Nail-preserving excision for subungual glomus tumour of the hand. Journal of plastic surgery and hand surgery, 48(3), 201–204. https://doi.org/10.3109/2000656X.2013.861842
- Pahwa, M., Pahwa, P., & Kathuria, S. (2010). Glomus tumour of the nail bed treated with the 'trap door' technique: a report of two patients. The Journal of dermatological treatment, 21(5), 298–300. https://doi.org/10.3109/09546630903277610
- Gould E. P. (1991). Sclerotherapy for multiple glomangiomata. The Journal of dermatologic surgery and oncology, 17(4), 351–352. https://doi.org/10.1111/j.1524-4725.1991.tb01710.x


