Summary Card
Definition
Giant Cell Tumours (GCTs) are nodular tumours found on the tendon sheath, commonly in the hands.
Pathophysiology
Previously thought to be inflammatory, GCTs are now considered a neoplastic process due to the discovery of a chromosomal abnormality in synovial cells expressing CSF1.
Clinical Features
It is a slow-growing lesion with occasional pain or sensory disturbances.
Investigations
Diagnosed through physical examination of a firm nodular mass that does not transilluminate. Imaging techniques such as X-ray, ultrasound, or MRI can be used for confirmation.
Treatment
Treatment is through marginal surgical excision. Radiation and CSF receptor inhibitors can also be considered.
Complications
Recurrence is common, often due to incomplete resection. Factors increasing recurrence include tendon involvement, joint extension, and extracapsular spread.
Primary Contributor: Dr Waruguru Wanjau, Educational Fellow.
Reviewer: Dr Suzanne Thomson, Educational Fellow.
Definition of Giant Cell Tumours of the Tendon Sheath
Giant Cell Tumours are nodular tumours commonly found on the tendon sheath, particularly in the hands.
Giant cell tumour can also be referred to as tenosynovial giant cell tumours, localized nodular tenosynovitis, xanthoma, or Pigmented Villonodular Synovitis (PVS). They are the second most common soft-tissue tumour seen in the hand, following ganglion cysts.
They are classified into localised or diffuse (Somerhausen NSA, 2002).
- Localized: Clear boundaries.
- Diffuse: tends to invade adjacent tissues with poorly defined margins, even when only a small area is involved (Kitagawa, 2020).
There are 2 types of tumours:
- Type I: Single lesions, and are more frequently detected.
- Type II: Two or more distinct tumours that are not joined together.
The image below illustrates a giant cell tumour of the tendon sheath.
Although rare, GCT can also occur in other parts of the body such as the spine, ankle, knee, and feet.
Pathophysiology of Giant Cell Tumours of the Tendon Sheath
Giant cell tumours were once thought to be inflammatory, but are now considered neoplastic due to a discovered chromosomal abnormality in synovial cells expressing CSF1.
Giant Cell Tumours (GCT) were initially believed to be caused by inflammation (Reilley, 1999). However, they are now recognized as neoplastic due to a clonal chromosomal abnormality in synovial cells that express CSF1 (Kitagawa, 2020).
Pathogenesis
- Chromosomal: Clonal chromosomal abnormality in synovial cells.
- CSF1 Gene Translocation: ~65 of patients with TSGCT (Kitagawa, 2020).
- Macrophages: CSF1 attracts macrophages, aiding tumour formation.
Cellular Characteristics
GCTs feature diverse cell types:
- Lipid-laden foam cells
- Multinucleated giant cells
- Round or polygonal stromal cells
- Hemosiderin deposits in a collagenous stroma (Khurana, 2023)
Clinical Features of Giant Cell Tumours of the Tendon Sheath
Diagnosis is through a physical exam of a firm nodular mass that does not transilluminate. It is a slow-growing lesion with occasional pain or sensory disturbances.
Classic Symptoms
Giant Cell Tumours of the Tendon Sheath typically present in women between the ages of 30-50 with these distinct symptoms:
- Growth: These tumours are typically painless and slow-growing, sometimes entering a dormant stage (Kitagawa, 2020).
- Texture: Firm and nodular.
- Transilluminate: It does not transilluminate.
- Location: Usually affects the tendon sheath, joint capsule, ligaments, tendons, palmar plate, and periosteum, but rarely the skin. Rarely, they involve extensor, lateral or circumferential areas. (Khurana, 2023).
- Sensory Effects: Sensory disturbances are rare (Fotiadis, 2011).
The image below illustrates the clinical presentation of a Giant cell tumour.
Differential Diagnosis
The differential diagnoses for Giant Cell Tumours include:
- Ganglion cyst: Common, non-cancerous lumps on tendons or joints.
- Desmoid tumour: Rare, non-metastasizing fibrous tumours.
- Fibroma/Fibrosarcoma: Benign or malignant fibrous tissue tumours.
- Glomangioma: Benign vascular tumours causing pain.
- Foreign body granuloma: Inflammatory reactions to foreign substances.
- Epidermoid cyst: Benign cysts from the epidermis.
- Sebaceous gland cyst: Benign cysts from blocked sebaceous glands.
Investigations of Giant Cell Tumours of the Tendon Sheath
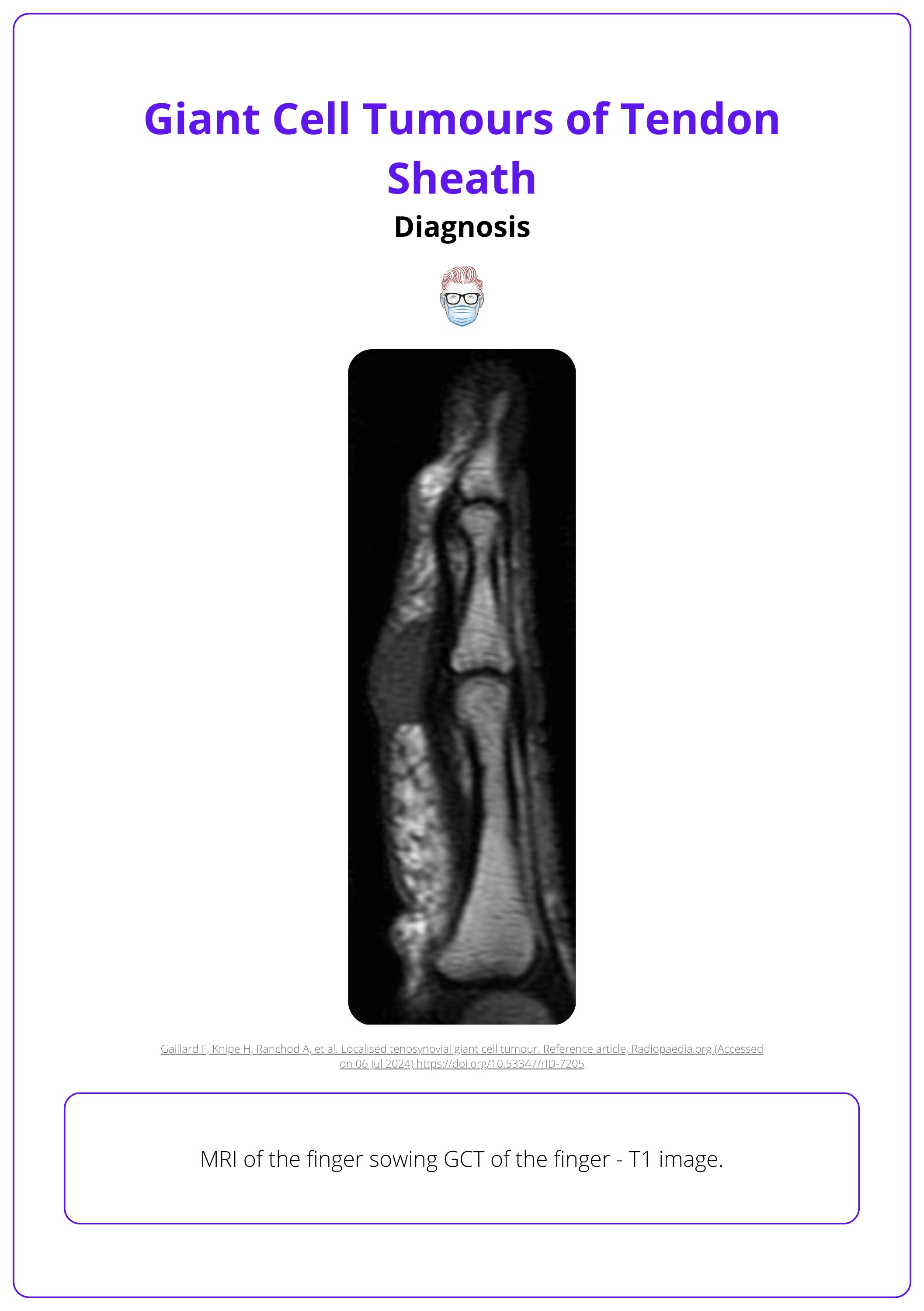
Investigations focus on pre-operative imaging (X-ray, ultrasound, or MRI) which can be confirmed histologically.
When diagnosing Giant Cell Tumours (GCT), several imaging techniques are used to identify and characterize the tumour.
- X-ray:
- Reveals pressure-type bone erosion.
- Ultrasound:
- Shows a solid, homogeneous, hypoechoic mass, often related to the flexor tendons of the fingers.
- Doppler studies indicate increased vascularity.
- MRI:
- T1-weighted images: Typically show isointense to slightly hyperintense signals compared to muscle.
- T2-weighted images: Display heterogeneous signal intensity with a mix of high and low signals.
- Gadolinium contrast: Highlights a contrast effect, enhancing visualization of the tumour.
The image below illustrates an MRI of the finger.
Histology
Microscopically, all tumours contain multinucleated giant cells, histiocytes, and hemosiderin deposits.
Differentiating between GCT and a ruptured ganglion cyst is difficult using an ultrasound.
Treatment of Giant Cell Tumours of the Tendon Sheath
The main treatment is marginal surgical excision, with radiation therapy and CSF receptor inhibitors as additional options.
Effective treatment of Giant Cell Tumours (GCT) of the tendon sheath is crucial for preserving hand function and preventing recurrence. The primary approach is surgical, with other therapies available for specific cases.
Surgical Treatment
Marginal excision is the primary treatment for Giant Cell Tumours of the tendon sheath. This surgical approach aims to remove the tumour while preserving hand function.
Procedure Tips:
- Careful Resection: The surgery should be performed cautiously, ideally under loupe magnification, to ensure precision.
- Pseudocapsule Presence: GCTs often have a pseudocapsule with clear boundaries, which helps in identifying the tumour margins.
- Adhesion and Invasion: Despite the clear boundaries, GCTs may partially adhere to or invade surrounding tissues, requiring meticulous surgical technique to avoid damage to adjacent structures.
This is detailed in the video below.
The main objectives are to achieve complete tumour excision and to maintain the function and neurovascular integrity of the affected digit.
Other Treatments
- Radiation Therapy: Occasionally recommended for progressive GCT cases, particularly those at risk of requiring amputation(Kitagawa, 2020).
- CSF Receptor Inhibitors: May be considered in certain cases as part of the treatment plan.
Complications of Giant Cell Tumours of the Tendon Sheath
Recurrence of GCT is common and often results from incomplete resection. Factors such as tendon involvement, joint extension, and extracapsular spread increase the risk of recurrence.
Understanding the complications associated with Giant Cell Tumours (GCT) of the tendon sheath is crucial for effective treatment and management. Recurrence is a common issue, often due to incomplete resection.
Recurrence Rates and Causes
- Reported Recurrence Rates: Range from 5-50%.
- Main Cause of Recurrence: Incomplete resection is the primary reason for tumour recurrence.
Risk Factors for Recurrence
- Tendon and Joint Involvement: Higher recurrence risk due to infiltration and joint spread.
- Type II Tumours: Undetected satellite lesions cause incomplete excision.
- Primary Location: Higher recurrence at DIPJ or thumb IPJ, especially with osteoarthritis or bone erosion.
- Neurovascular and Extracapsular Spread: Increases recurrence risk and complicates resection.
- Piecemeal Resection: Leads to incomplete removal and recurrence.
Conclusion
1. Tenosynovial Giant Cell Tumors (TSGCTs): Gained a comprehensive understanding of the nature, classification, and epidemiology of TSGCTs.
2. Pathophysiology: Learned about the shift in understanding from inflammatory to neoplastic nature of TSGCTs due to genetic discoveries, emphasizing the role of CSF1 in their development.
3. Diagnostic Techniques: Reviewed the diagnostic process for TSGCTs, emphasizing the importance of physical examination, imaging modalities like X-ray, ultrasound, and MRI, and the role of histology in confirming the diagnosis.
4. Treatment Options: Explored treatment methods including surgical excision, radiation therapy, and novel treatments like CSF1 receptor inhibitors.
5. Complications: Discussed the common complications associated with TSGCTs, particularly recurrence, and factors that influence it.
Further Reading
- Fotiadis E, Papadopoulos A, Svarnas T, Akritopoulos P, Sachinis NP, Chalidis BE. Giant cell tumour of tendon sheath of the digits. A systematic review. Hand (N Y). 2011 Sep;6(3):244-9. doi: 10.1007/s11552-011-9341-9. Epub 2011 Jun 1. PMID: 22942846; PMCID: PMC3153624.
- Reilly KE, Stern PJ, Dale JA. Recurrent giant cell tumours of the tendon sheath. J Hand Surg Am. 1999 Nov;24(6):1298-302. doi: 10.1053/jhsu.1999.1298. PMID: 10584957.
- Briët JP, Becker SJ, Oosterhoff TCh, Ring D. Giant cell tumour of tendon sheath. Arch Bone Jt Surg. 2015 Jan;3(1):19-21. Epub 2015 Jan 15. PMID: 25692164; PMCID: PMC4322119.
- Somerhausen NSA, Cin PD. Giant cell tumour of tendon sheath. In Fletcher, C.D., Unni, K.K. and Mertens, F. eds., 2002. p. 110―1. Pathology and genetics of tumours of soft tissue and bone(Vol. 4). Iarc.
- Anderson WJ, Doyle LA. Updates from the 2020 World Health Organization Classification of Soft Tissue and Bone Tumours. Histopathology. 2021 Apr;78(5):644-657. doi: 10.1111/his.14265. Epub 2021 Jan 12. PMID: 33438273.
- Kitagawa Y, Takai S. Optimal Treatment for Tenosynovial Giant Cell tumour of the Hand. J Nippon Med Sch. 2020 Sep 9;87(4):184-190. doi: 10.1272/jnms.JNMS.2020_87-408. Epub 2020 Apr 30. PMID: 32350187.
- Khurana A, Singh JP, Preeti, Littlefield Z, Young S, Shah A. Demystifying Giant Cell Tumours of Tendon Sheath (GCTTS): A Case Series of 18 Cases with Review of Literature. Indian J Orthop. 2023 Sep 21;57(11):1858-1873. doi: 10.1007/s43465-023-00990-8. PMID: 37881282; PMCID: PMC10593659.


