Summary Card
Overview
Finger amputation refers to the loss of a digit due to trauma or surgery, with thumb injuries being the most functionally significant. Replantation aims to restore function, sensation, and aesthetics.
Indications
Replantation is preferred for thumb, multiple-digit, and distal injuries. Contraindications include severe crush injuries, prolonged ischemia (>12 hours warm, >3 days cold), and multilevel amputations.
Clinical Assessment
Preoperative preparation involves assessing ischemia time, injury mechanism, and comorbidities, conducting X-rays and vascular studies, starting antibiotics and anticoagulation, and preserving the amputated part in a cold water bath.
Decision-Making Factors
Injury type impacts survival — sharp injuries (~90%) have the best prognosis, while avulsions (~60%) often require vein grafts. Fingers tolerate ischemia better than muscle-containing tissues.
Surgical Procedure
The replantation process follows a stepwise approach: bone fixation, tendon and nerve repair, arterial and venous anastomosis, and skin closure. Postoperatively, vascular monitoring and early mobilization.
Post-Operative Care
Optimal recovery requires vascular monitoring, anticoagulation, immobilization, and early rehabilitation.
Complications
Key complications include venous insufficiency (blue, swollen) and arterial thrombosis (pale, cold), managed through elevation, leech therapy, or surgical revision.
Updated by: Dr Hatan Mortada, Educational Fellow.
Verified by thePlasticsFella ✅
Overview of Finger Replantation
Finger amputation refers to the loss of a digit due to trauma or surgery, with thumb injuries being the most functionally significant. Replantation aims to restore function, sensation, and aesthetics.
Finger amputation, also referred to as re-implantation or re-attachment surgery, involves the loss of a digit, ranging from distal fingertip injuries to proximal hand amputations.
Understanding the distinction between replantation and revascularization is crucial in determining the appropriate surgical approach.
- Replantation refers to the reattachment of a completely amputated part with the goal of restoring function, sensation, and aesthetics.
- Revascularization, in contrast, is the restoration of blood flow to an incompletely amputated digit where some soft tissue connections remain intact.
A successful outcome depends on careful patient selection, precise microsurgical technique, and structured post-operative rehabilitation (Bregman, 2023).
The first successful digital replantation was performed in 1965, marking a major milestone in microsurgery.
Indications for Finger Replantation
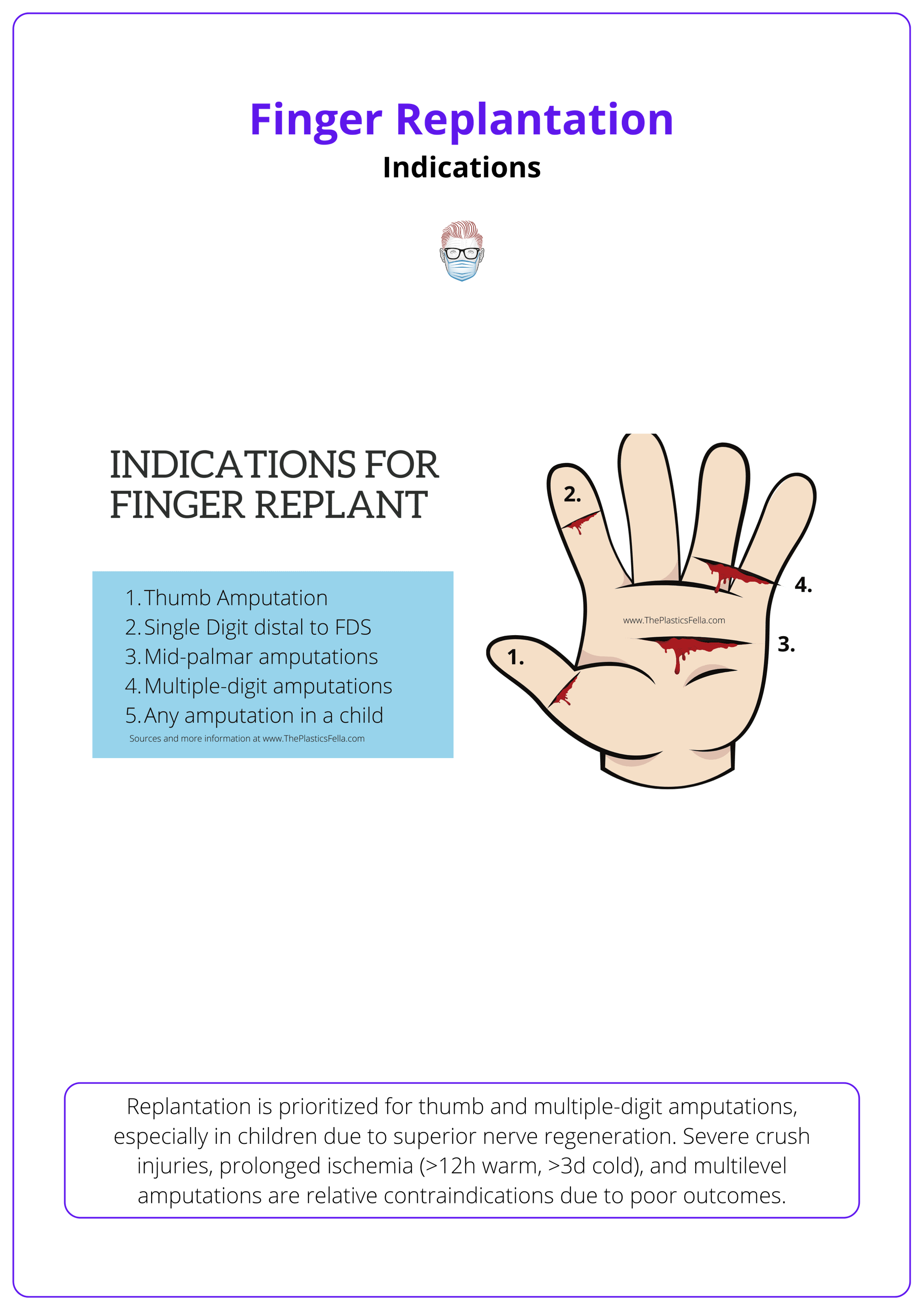
Replantation is prioritized for thumb and multiple-digit amputations, especially in children due to superior nerve regeneration. Severe crush injuries, prolonged ischemia (>12h warm, >3d cold), and multilevel amputations are relative contraindications due to poor outcomes.
The decision to replant depends on viability, functional recovery, and patient factors (Peterson, 2018).
The focus of replanting any part of the upper extremity is maximizing functional outcomes rather than simply ensuring the survival of the amputated part. Functional success depends on,
- Level of amputation.
- Arterial intima damage
- Soft tissue condition.
- Patient factors such as age, occupation, and cultural significance.
Indications for Finger Replantation
Replantation is considered when it significantly improves function (Barbary, 2013). Key indications include,
- Thumb Amputation: essential for 40-50% of hand function; salvageable thumb is better than a prosthetic.
- Multiple-Digit Amputation: particularly when the thumb or middle finger is involved.
- Zone 1 (Distal to FDS Insertion): improve function despite potential DIP stiffness.
- Mid-Palm/Hand Amputation: preferrable to prosthetics when function can be restored.
- Pediatric Cases: superior nerve regeneration and adaptability enhance outcomes.
Zone 2 (Proximal to FDS Insertion) is controversial due to high risk of PIP stiffness (Zhu, 2021).
Indications for finger replantation are summarised in the image below.
Contraindications for Replantation
Replantation is unlikely to succeed in cases with:
- Severe Crush Injuries: High risk of thrombosis and poor recovery.
- Multilevel Amputations: Complex reconstruction with low success rates.
- Prolonged Ischemia: >12h warm ischemia has poorer outcomes, >3d cold ischemia may be viable but remains controversial.
- Life-Threatening Injuries: Patient stabilization takes priority.
The general indications and contraindications for replantation are summarized in the table below.
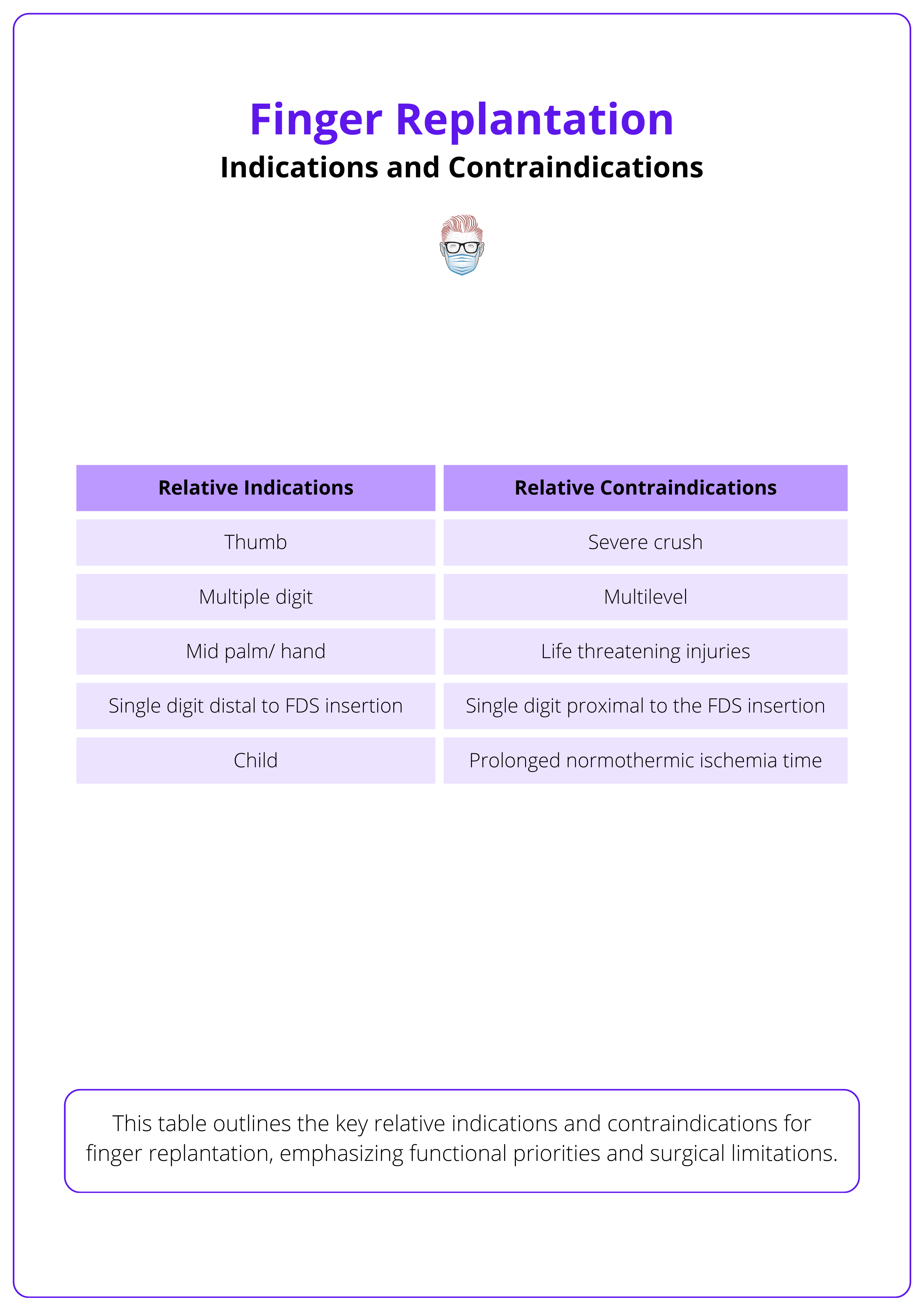
Thumb and index finger amputations should be prioritized, as they are the most functionally important digits.
Clinical Assessment for Finger Replantation
Preoperative preparation for replantation involves assessing ischemia time, injury mechanism, and comorbidities, conducting X-rays and vascular studies, starting antibiotics and anticoagulation, and preserving the amputated part in a cold water bath to minimize tissue degradation.
Preoperative Preparation
A thorough preoperative evaluation is essential to improve replantation success rates and minimize complications. The key steps include:
- Clinical Assessment: Evaluate ischemia time, injury mechanism, and patient comorbidities.
- Imaging: X-rays to assess fractures and vascular studies if perfusion is unclear.
- Antibiotics & Anticoagulation: These are initiated to prevent infection and thrombosis.
- Digit Preservation: The amputated part should be wrapped in sterile gauze, placed in a waterproof container, and stored in a cold water bath (not frozen) to slow tissue degradation.
Decision-Making Factors for Finger Replantation
Injury type impacts survival — sharp injuries (~90%) have the best prognosis, while avulsions (~60%) often require vein grafts. Fingers tolerate ischemia better than muscle-containing tissues, but survival rates drop beyond 24 hours.
Replantation success depends on 4 important factors: injury mechanism, ischaemia time, anatomical location, and patient factors.
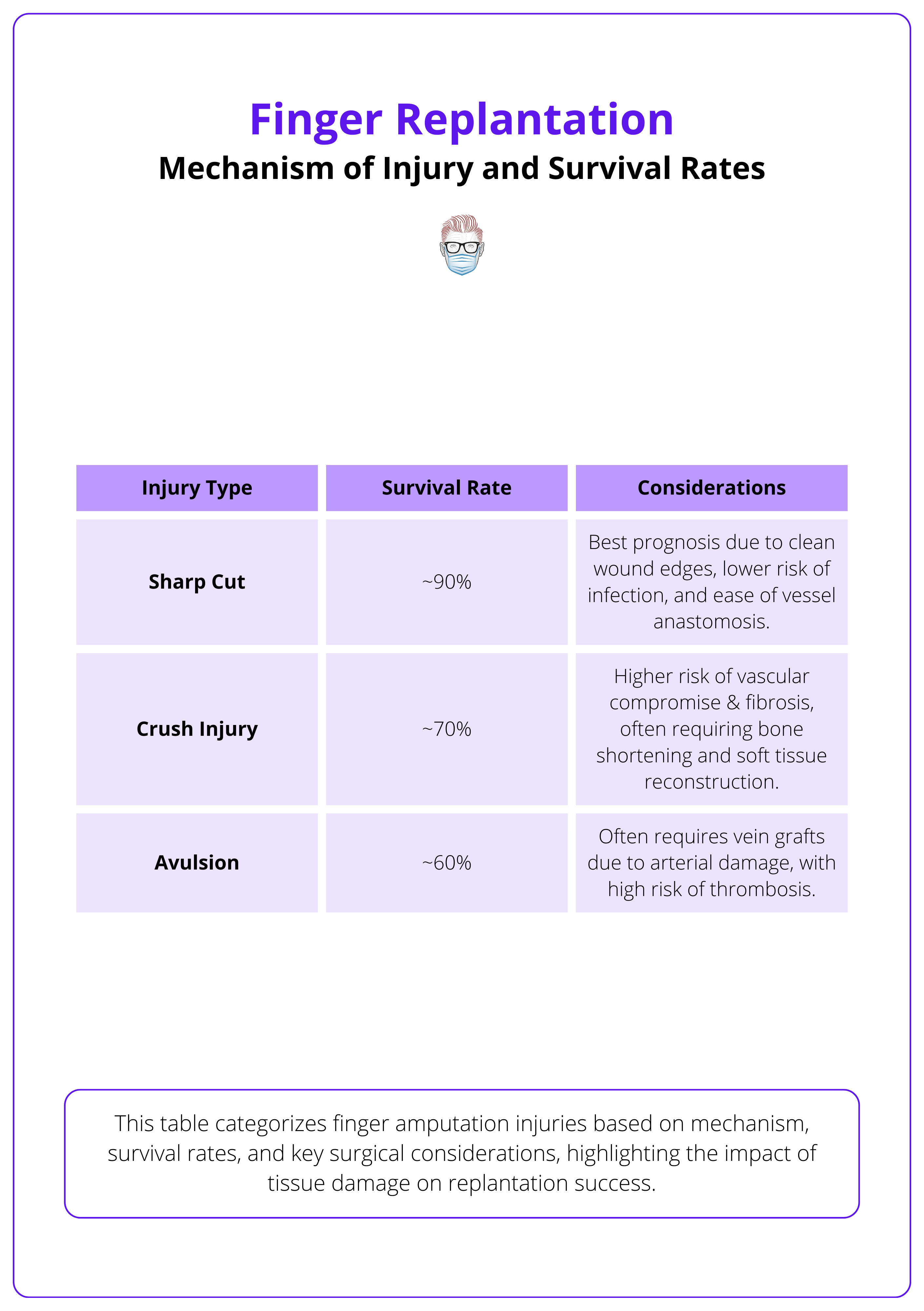
Mechanism of Injury & Survival Rates
Finger amputations are classified into three major types, each with varying success rates.
- Sharp Injuries (~90% survival): Best prognosis due to clean-cut tissue planes.
- Crush Injuries: Poor prognosis due to extensive soft tissue damage.
- Avulsion Injuries (~60% survival): Often require vein grafts due to vessel retraction.
The injury mechanisms and their survival rates are summarized in the table below.
Ischemia Time Considerations
Fingers have a higher tolerance for ischemia compared to muscle-containing tissues (Chang, 2024):
- <12 hours: 93% survival, optimal function.
- 12–24 hours: 87% survival, risk of stiffness and sensory loss.
- >24 hours: 65% survival, often requires secondary procedures.
- Cold ischemia >3 days: Possible, but with diminished function.
Fingers tolerate ischemia longer than other tissues because they lack muscle, allowing replantation success even after prolonged ischemia
Anatomical Zones & Functional Outcomes:
The FDS insertion defines key anatomical zones.
- Distal Zone (beyond FDS insertion): Better DIP joint motion, protective sensation.
- Proximal Zone (proximal to FDS insertion): Higher risk of PIP joint stiffness.
Anatomical zones and their functional outcomes are summarised below.
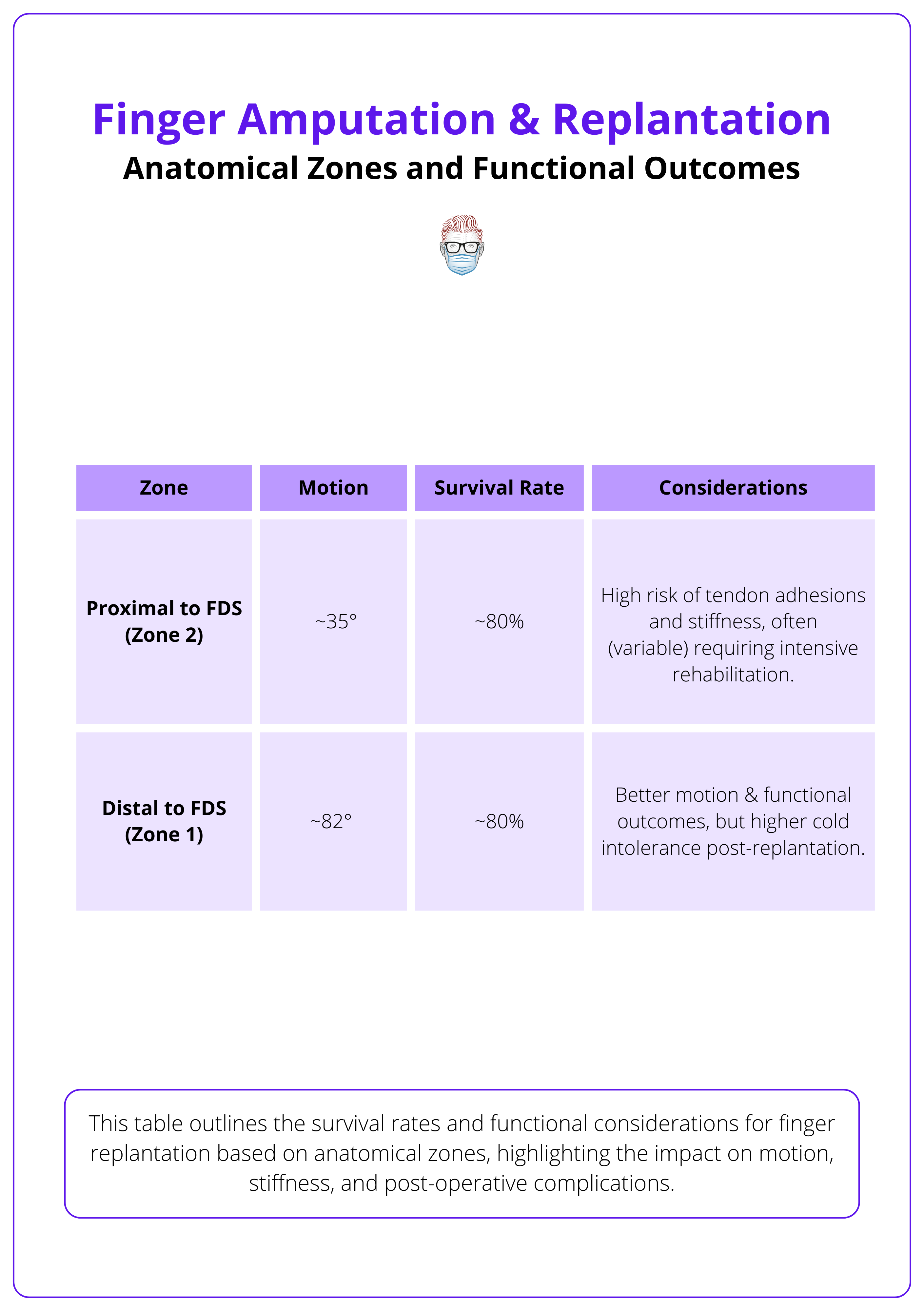
Studies using Tamai and Ishikawa classifications suggest that distal tip replantation preserves length, sensation, and motion without significantly affecting grip strength or cold intolerance (Sebastin, 2012).
Patient-Related Factor
Certain patient characteristics influence replantation success.
- Age: Children have superior nerve regeneration and better outcomes.
- Smoking: Conflicting evidence, but potential microvascular impact.
- Comorbidities: Diabetes may impair microvascular healing.
Children have the highest replantation success rates due to their exceptional nerve regeneration ability.
Surgical Procedure for Finger Replantation
The replantation process follows a stepwise approach: bone fixation, tendon and nerve repair, arterial and venous anastomosis, and skin closure. Postoperatively, vascular monitoring and early mobilization.
Finger replantation prioritizes survival and function, following the "Macro Before Micro" principle — stabilizing bone before soft tissue repair. Beyond reattachment, the goal is to restore hand stability, movement, and sensation. Key considerations include.
- Bone Shortening: Facilitates tension-free closure and vascular anastomosis.
- Tendon Length Preservation: Reduces adhesions and maintains mobility.
- Vein Grafting: Necessary when direct anastomosis is not feasible.
- Replantation Priority: Thumb > Long > Ring > Small > Index
- Multiple Amputations: Structure-first repair is more efficient than digit-by-digit reconstruction (Ono, 2020).
These steps of finger replanting are illustrated below.
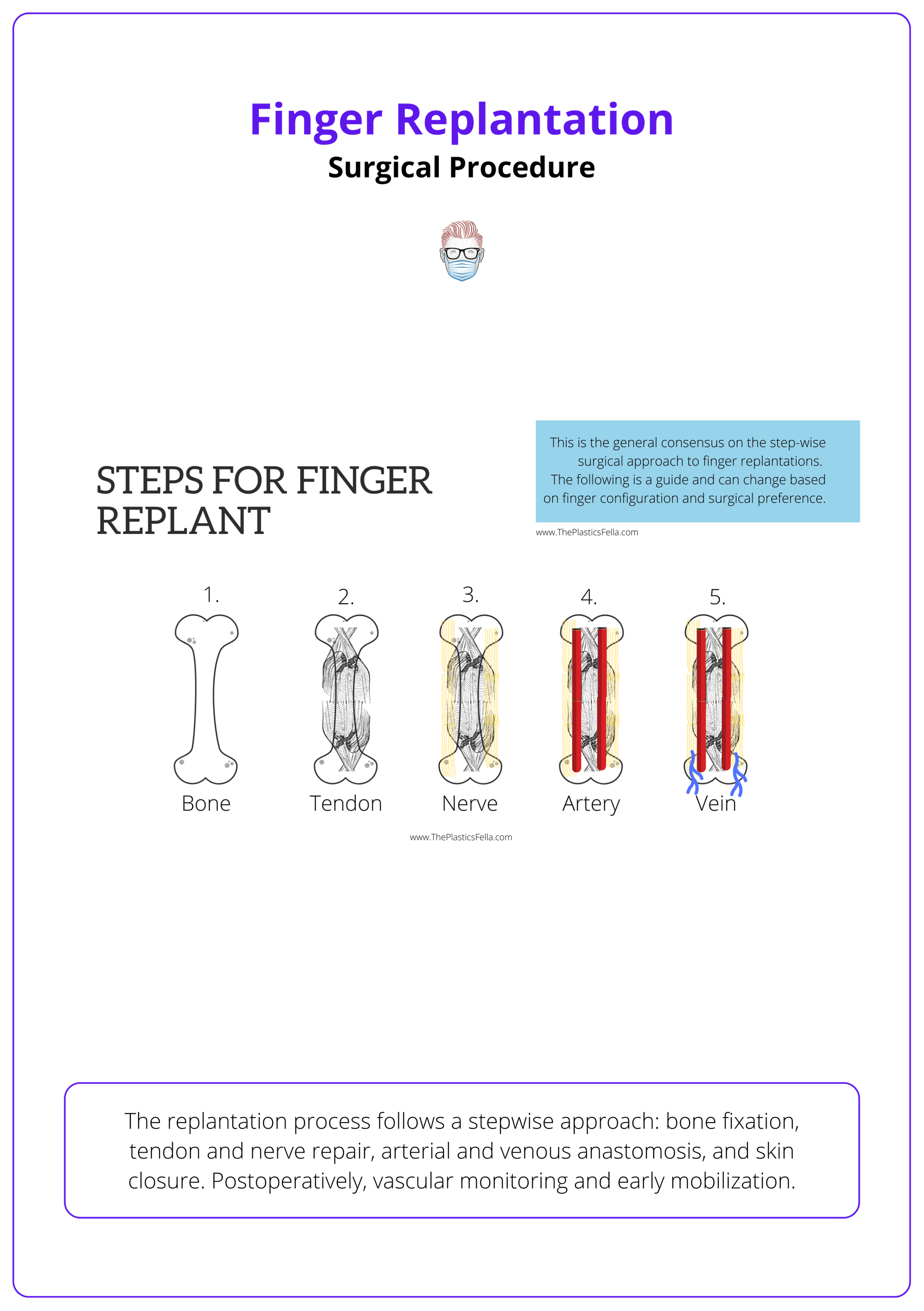
Bone Fixation
- The first step in replantation is stabilising the skeletal framework to allow precise soft tissue repair.
- Methods: K-wires, interosseous wires, mini-plates, or screws.
- Bone Shortening: Typically required to prevent excessive tension on vessels and nerves.
Extensor & Flexor Tendon Repair
- Tendon repair is essential for functional movement and grip strength.
- Techniques: Core and epitendinous sutures for durability and minimal gap formation.
- Priority: Spend time on a good flexor tendons repair
Two surgical teams working simultaneously can significantly reduce operative time.
Nerve Repair
- Nerve coaptation is crucial in proximal amputations to restore sensory and motor function.
- Preferred Method: Direct coaptation whenever possible.
- Nerve Grafting: Required when there is significant nerve loss. Common donor nerves: posterior interosseous nerve, sural nerve
Arterial Anastomosis
- Adequate arterial supply is critical for digit survival.
- At Least One Artery Must Be Repaired: Preferably tension-free.
- Vein Grafting: Used when direct arterial repair is not possible due to vessel damage or retraction.
Venous Repair
- Venous outflow is equally important as arterial inflow; inadequate venous drainage leads to venous congestion and failure.
- Two or More Veins Should Be Repaired: If possible, to improve drainage.
- Preferred Veins: Dorsal veins are larger, more accessible, and preferred for anastomosis. Volar veins are an alternative if dorsal veins are unavailable.
- Salvage Techniques: If venous repair is inadequate, leech therapy or controlled external bleeding can be used to manage congestion.
The survival rate of replantation increases significantly with successful venous repair, reducing the risk of congestion.
Skin Closure
- Skin coverage ensures wound healing and prevents infection while also supporting venous drainage.
- Options: Direct closure, local flaps, or skin grafting depending on tissue loss.
- Delayed Closure: Considered in cases with excessive swelling or questionable perfusion.
Post-Operative Care of a Finger Replant
Optimal recovery requires vascular monitoring, anticoagulation, immobilization, and early rehabilitation.
There is no universal postoperative protocol for replantation. Early vascular monitoring, tailored anticoagulation, structured rehabilitation, and patient involvement are critical to achieving the best functional outcomes.
Vascular Monitoring
- Frequent checks are essential to identify arterial insufficiency or venous congestion.
- Assess capillary refill, skin color, and temperature regularly.
- Maintain a warm environment to promote vasodilation and circulation.
- Avoid vasoconstrictors such as caffeine, nicotine, and chocolate.
Anticoagulation
- There is no consensus on anticoagulation in finger replantation, and practices vary widely (Retrouvey, 2019). Common approaches include,
- Systemic: Aspirin, intravenous heparin, LMWH, dextran.
- Local: Heparin ("chemical leech") applied at the surgical site.
- No Thromboprophylaxis: Some surgeons avoid anticoagulation due to lack of strong evidence.
Hand Therapy
- Strict movement protocols prevent stress on vascular anastomoses and avoid adhesions.
- Positioning should maintain alignment while avoiding excessive tension on repaired structures.
- Start motion exercises within 2-3 weeks, balancing mobility with repair protection.
Secondary Procedures
- Delayed rehabilitation may necessitate additional surgery to improve function:
- Flexor Tenolysis: Releases adhesions to restore tendon movement.
- DIP Joint Arthrodesis: Performed when joint mobility remains severely restricted.
Rehabilitation should begin as early as possible but must be individualized based on injury and repair stability.
Complications of Finger Replantation
Replantation has a high survival rate (80-90%) in ideal candidates. Early complications, such as arterial thrombosis and venous congestion, require urgent management. Long-term issues, including joint stiffness and cold intolerance, affect functional recovery.
Successful replantation depends on early vascular monitoring, infection control, and structured rehabilitation to prevent complications and optimize function. In cases of severe injury, amputation may be a more practical option to avoid prolonged recovery with uncertain functional gains.
Early Complications
The first 72 hours are critical for vascular monitoring and infection control. Venous insufficiency and arterial thrombosis are the two most common complications in finger replantation surgery.
Arterial Thrombosis
- Signs: Pale, cold, dusky digit.
- Management: Immediate revision surgery, loosening of dressings, and nerve block to restore perfusion.
Venous Congestion
- Signs: Blue, swollen, congested digit.
- Management: Leech therapy, vein grafts, or surgical re-exploration to relieve venous obstruction.
Infection
- Signs: Redness, swelling, pus formation.
- Management: Aggressive IV antibiotics, wound care, and surgical drainage if needed.
The table below compares the arterial and venous complications.
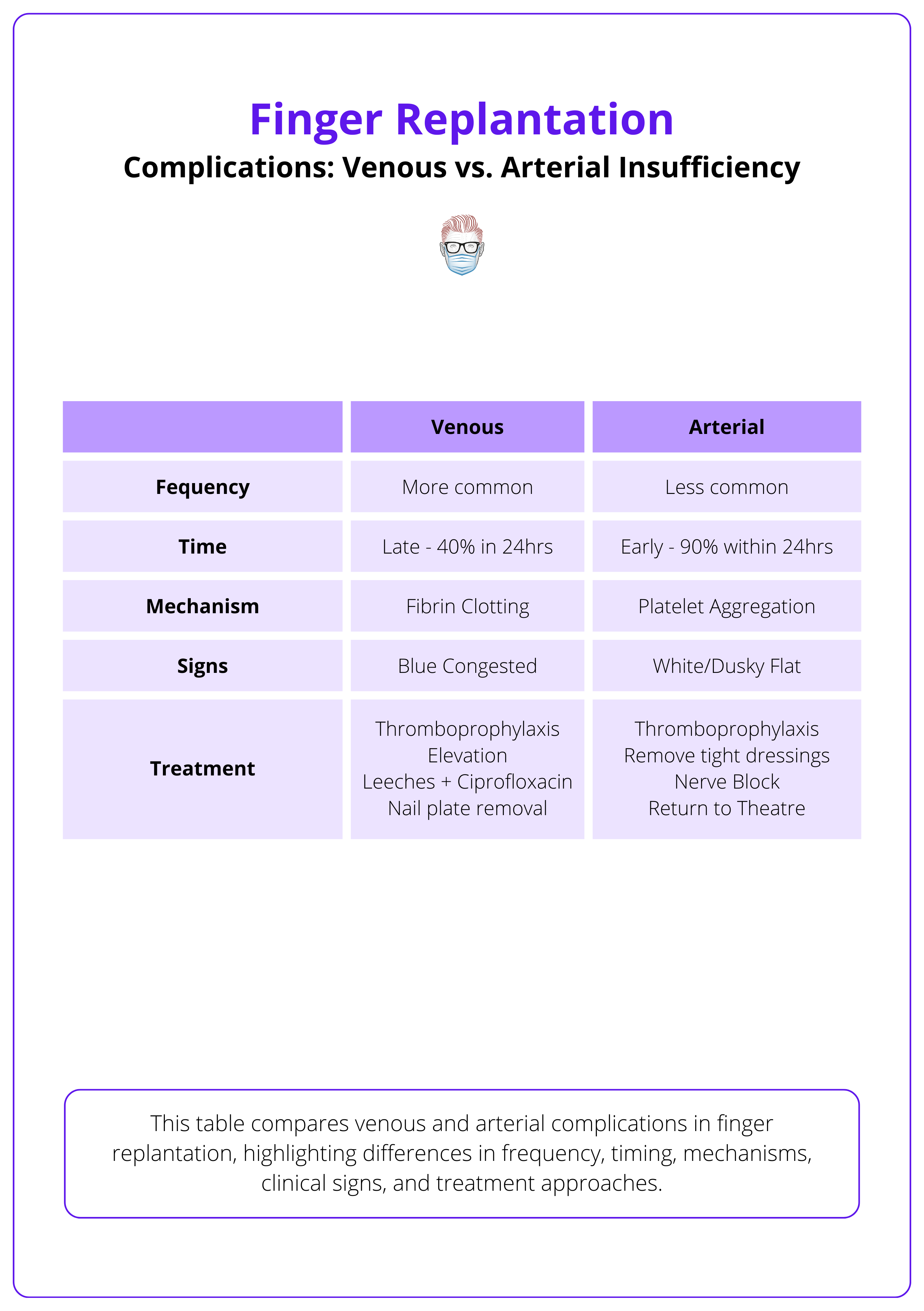
90% of vascular complications occur within the first 24-72 hours — early detection and intervention are critical to prevent digit loss
Late Complications
Delayed complications impact movement, sensation, and circulation, often requiring secondary interventions. While replantation can restore function, long-term success depends on injury severity, surgical precision, and rehabilitation commitment.
Joint Stiffness
- Cause: Prolonged immobilization, tendon adhesions, or capsular contracture.
- Management: Early rehabilitation, secondary tenolysis, or capsulotomy.
Cold Intolerance
- Signs: Pain and discomfort in cold exposure.
- Management: Conservative treatment with patient education and protective gloves.
Neuroma Formation
- Signs: Localized pain, hypersensitivity at the nerve injury site.
- Management: Excision or nerve grafting if symptomatic.
Common complications and their management options are summarised in the table below.
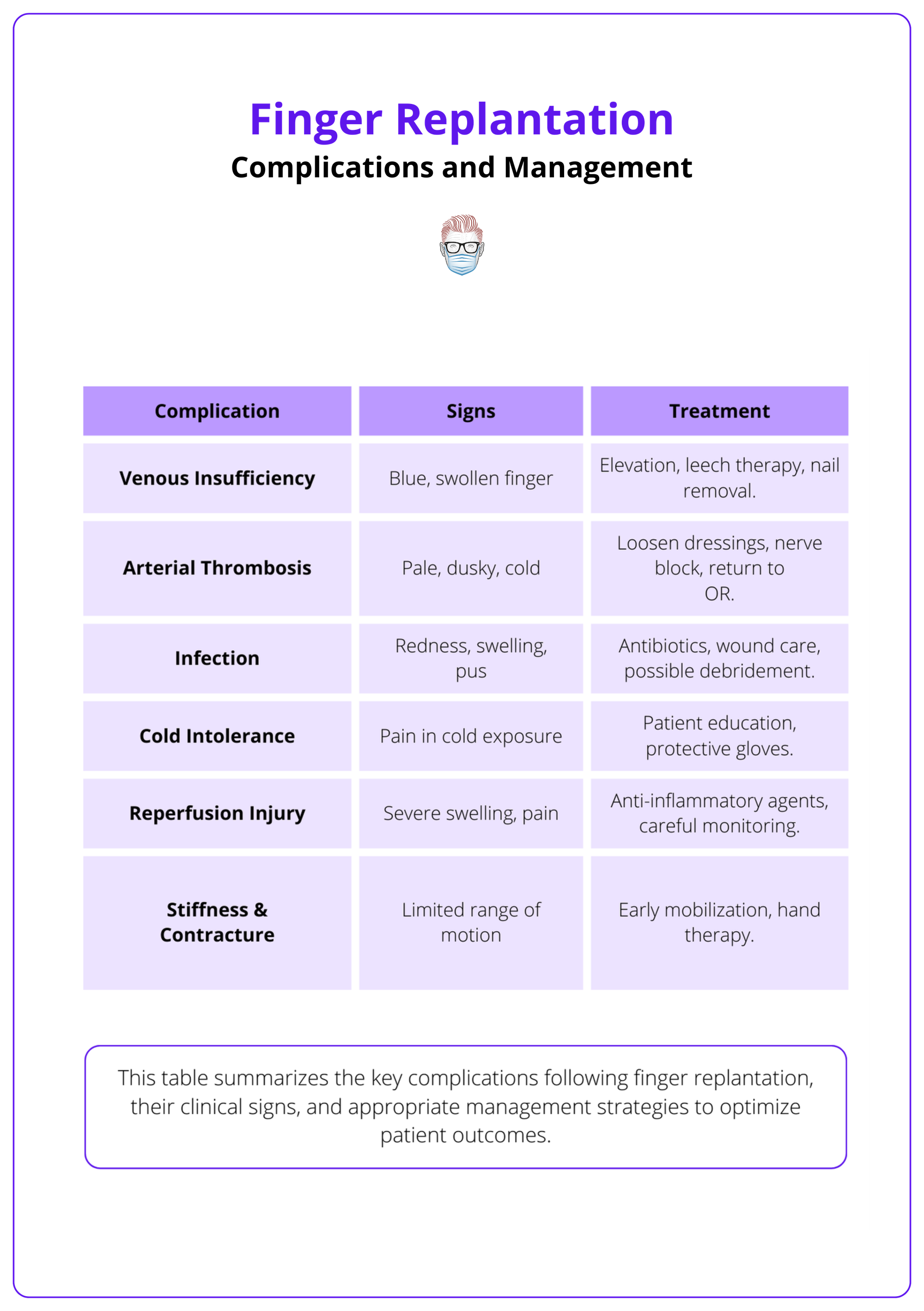
Cold intolerance is one of the most common long-term complications, significantly impacting daily activities and patient satisfaction.
Conclusion
1. Overview: Understanding the causes and classification of finger amputation and replantation, along with the importance of functional restoration.
2. Indications & Contraindications: Recognizing the key factors influencing the decision for replantation versus revision amputation.
3. Principles: Identifying the mechanism of injury, ischemia time considerations, and anatomical factors that impact surgical outcomes.
4. Procedure: Learning the stepwise surgical approach, including bone fixation, tendon and nerve repair, and vascular anastomosis.
5. Complications: Familiarising with common post-operative issues such as arterial thrombosis, venous insufficiency, infection, and stiffness.
6. Discussion: Comparing the benefits and drawbacks of replantation versus amputation for optimal patient outcomes.
Further Reading
- Rebowe RE, Tannan SC. Digit Replantation. [Updated 2022 Sep 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448187/
- Pet MA, Ko JH. Indications for Replantation and Revascularization in the Hand. Hand Clin. 2019;35(2):119-130. doi:10.1016/j.hcl.2018.12.003
- Chang MK, Lim JX, Sebastin SJ. Current trends in digital replantation—a narrative review. Annals of Translational Medicine. 2024 Feb 26.
- Maricevich M, Carlsen B, Mardini S, Moran S. Upper extremity and digital replantation. Hand (N Y). 2011;6(4):356-363. doi:10.1007/s11552-011-9353-5
- Kleinert HE, Juhala CA, Tsai TM, Van Beek A. Digital replantation—selection, technique, and results. Orthopedic Clinics of North America. 1977 Apr 1;8(2):309-18.
- Sears ED, Chung KC. Replantation of finger avulsion injuries: a systematic review of survival and functional outcomes. J Hand Surg Am. 2011;36(4):686-694. doi:10.1016/j.jhsa.2010.12.023
- Scheker LR, Becker GW. Distal finger replantation. The Journal of hand surgery. 2011 Mar 1;36(3):521-8.
- Hayashi, Kota MD1; Hattori, Yasunori MD, PhD1; Chia, Dawn Sinn Yii MBBS2; Sakamoto, Sotetsu MD1; Sonezaki, Shicho MD1; Doi, Kazuteru MD, PhD1. Fingertip Replantation: Surgical Technique, Tips, and Tricks. Plastic and Reconstructive Surgery 153(1):p 168-171, January 2024. | DOI: 10.1097/PRS.0000000000010521


