Summary Card
Overview
Injectable fillers are essential tools in nonsurgical facial rejuvenation, offering tailored solutions for restoring volume, contouring, and smoothing wrinkles.
Classification
Injectable fillers are primarily divided into physical fillers, which provide immediate volume (e.g., HA), and biostimulatory fillers, which promote long-term collagen production (e.g., PLLA, CaHA, PCL).
Indications and Filler Selection
Filler choice depends on anatomy, patient goals, and material properties. Common indications include volume restoration, wrinkle correction, lip shaping, skin rejuvenation, and scar treatment.
Injection Technique
Filler injections require a thorough pre-treatment evaluation, detailed anatomical planning, and tailored use of needles or cannulas depending on the target area, injection depth, and vascular risk.
Contraindications and Adverse Effects
Injectable fillers are contraindicated in certain medical conditions and carry a risk of adverse effects ranging from mild swelling to serious complications like vascular occlusion and, rarely, blindness.
Primary Contributor: Dr Benedetta Agnelli, Educational Fellow
Verified by thePlasticsFella ✅
Overview of Injectable Fillers
Injectable fillers are versatile, noninvasive treatments used to restore volume, contour the face, and reduce wrinkles.
Fillers offer a customizable solution for facial rejuvenation by either filling tissue directly or stimulating collagen production, depending on the material and placement depth.
While no filler meets every ideal trait, most aim to strike a balance between safety, performance, and natural results.
- Biocompatible and Non-immunogenic: Minimizes inflammation
- Safe and Predictable: Consistent results with minimal complications.
- Durable but Reversible: Long-lasting with reversibility (e.g., hyaluronidase)
- Easy to Inject and Natural Feeling: smooth and feel undetectable.
- Ages with the Patient: Should adapt with facial changes over time.
Fillers can be classified by how long they last and their mechanism of action.
- Temporary (e.g., Hyaluronic Acid):
Most commonly used; hydrating, reversible, and ideal for fine lines and lips. - Semi-Permanent (e.g., CaHA, PLLA):
Longer-lasting; adds volume and stimulates collagen. - Permanent (e.g., PMMA):
Long-term results but less forgiving; reserved for select cases.
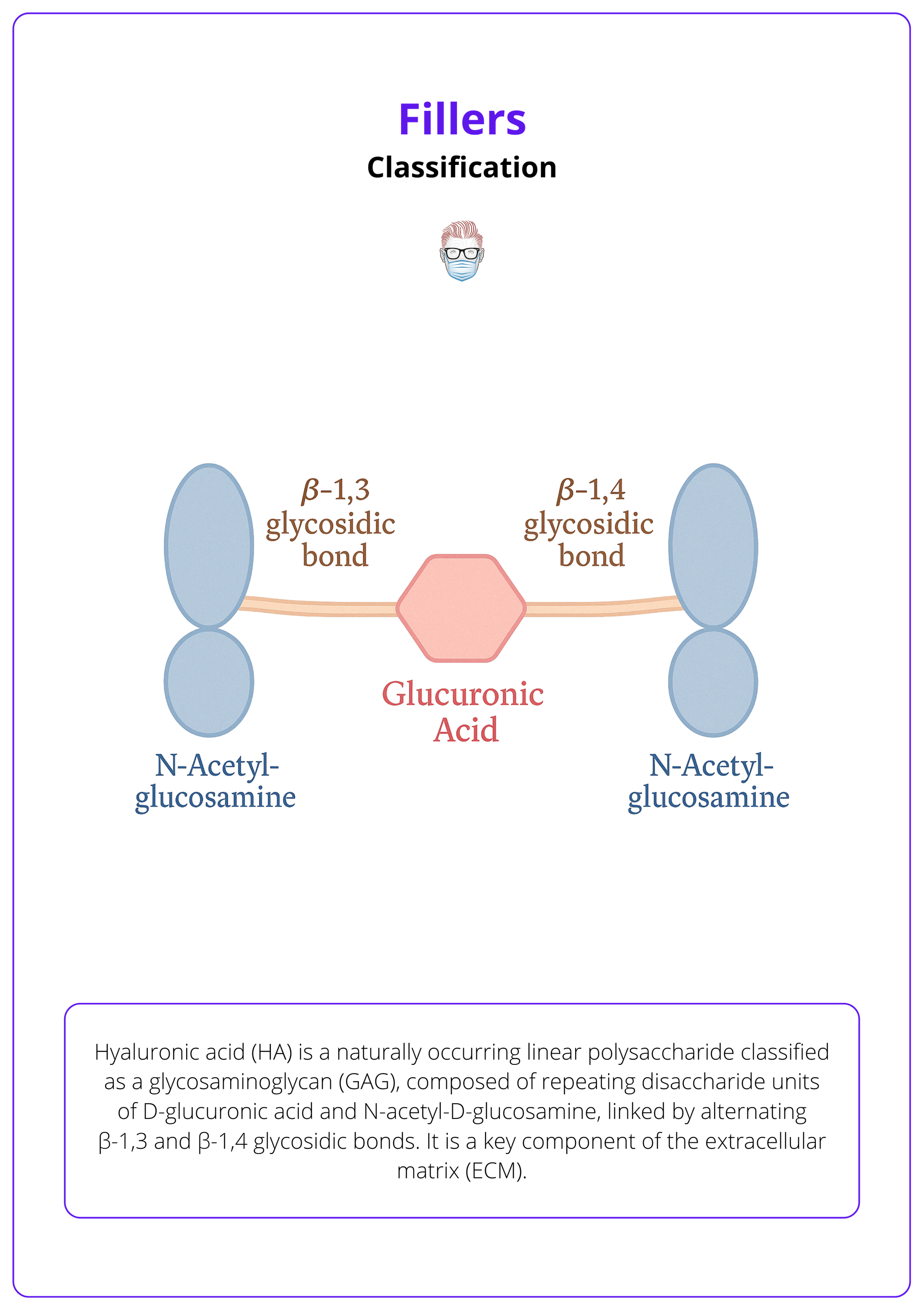
About half of the 15 grams of hyaluronic acid in a 70 kg human is found in the skin (Juncan, 2021).
Classification of Injectable Fillers
Injectable fillers are categorized as physical fillers (immediate volume), biostimulatory fillers (collagen stimulation), and autologous fillers (from the patient’s own tissue)
Classification of fillers is essential for selecting the appropriate product based on desired duration, mechanism of action, and anatomical site. While physical and biostimulatory fillers dominate non-autologous options, autologous fillers (fat grafting) are discussed separately due to their unique surgical handling.
- Physical Fillers: Provide immediate volume replacement.
- Biostimulatory Fillers: Promote collagen synthesis.
Physical Fillers
Physical fillers provide immediate volume restoration by physically occupying space within soft tissues.
Hyaluronic Acid (HA)
Naturally occurring GAG that maintains skin hydration and elasticity. Modified via crosslinking to extend durability when used as a filler — endogenous HA has a very short half-life.
The structure of hyaluronic acid is illustrated below.
The physicochemical properties of HA fillers shape their clinical performance, with variations tailored to different anatomical areas and goals
- Rheology: The elastic modulus (G′) determines stiffness—high G′ for deep support (e.g., jawline), low G′ for dynamic areas (e.g., lips).
- Cohesivity: Indicates the gel’s ability to hold together; higher cohesivity resists migration and retains shape.
- Extrusion Force: Affects ease of injection; influenced by particle size and crosslinking.
- Swelling Factor: Measures water absorption post-injection; more crosslinking means less swelling and more predictable volume.
These properties of fillers are illustrated below.
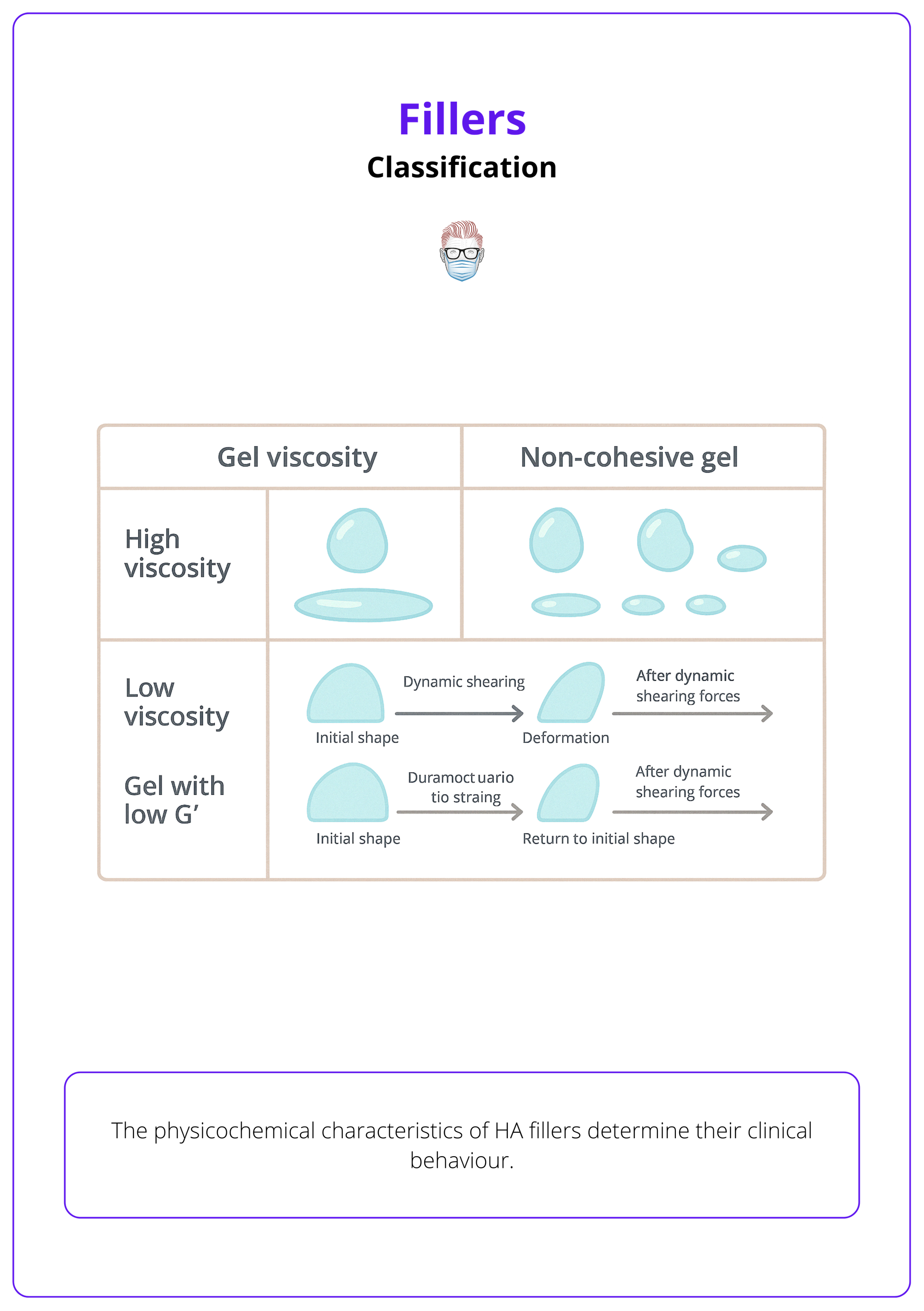
Adding lidocaine to HA fillers enhances comfort without significantly changing their physical properties (Guo, 2023).
Collagen Fillers
Collagen is a key structural protein of the ECM, and its loss contributes to the visible signs of aging.
The fillers restore dermal structure but are less commonly used due to short duration and immunogenicity risks in animal-derived forms. Recombinant collagen is gaining attention for better safety.
Isologen involves culturing a patient’s own fibroblasts from a skin biopsy to produce injectable collagen—a personalized autologous filler.
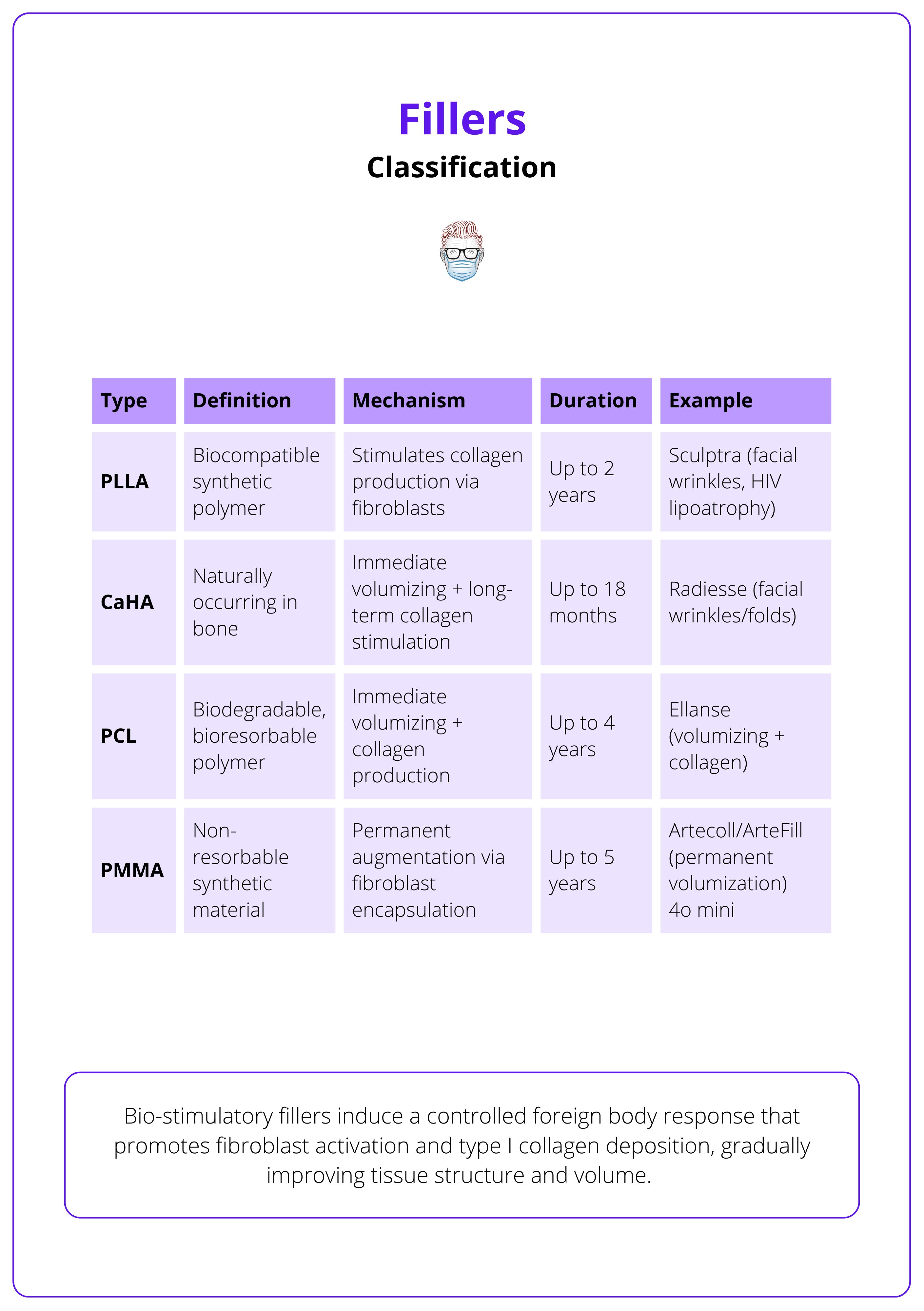
Biostimulatory Fillers
Bio-stimulatory fillers induce a controlled foreign body response that promotes fibroblast activation and type I collagen deposition, gradually improving tissue structure and volume.
Poly(L-lactic acid) (PLLA)
- Definition: Semipermanent, biocompatible synthetic polymer.
- Mechanism of Action: Stimulation of collagen production through fibroblast activation. Gradual volume restoration over several months, as the microspheres are broken down by macrophages, leads to collagen deposition.
- Duration: Up to 2 years.
- Example: Sculptra is FDA-approved for facial wrinkles and HIV-associated lipoatrophy.
Calcium hydroxylapatite (CaHA)
- Definition: Semipermanent, naturally occurring substance, primarily found in human bone.
- Mechanism of Action: CaHA provides an immediate volumizing effect followed by long-term collagen stimulation as fibroblasts grow around the microspheres.
- Duration: Up to 18 months.
- Example: Radiesse (CaHA suspended in a carrier gel) to treat moderate to severe facial wrinkles and folds. The product is injected deep into the dermis using a linear technique.
Polycaprolactone (PCL)
- Definition: Biocompatible, biodegradable, and bioresorbable polymer.
- Mechanism of Action: Like PLLA, PCL degrades into CO2 and H2O, which are eliminated from the body.
- Duration: Up to 4 years.
- Example: Ellanse, a filler containing 30% PCL microspheres and 70% carboxymethylcellulose (CMC) gel, offers both immediate (volumizing) and long-lasting effects (collagen production and neovascularization).
Poly(methyl methacrylate) (PMMA)
- Definition: Non-resorbable synthetic material, providing permanent tissue augmentation.
- Mechanism of Action: PMMA microspheres are encapsulated by fibroblasts and collagen fibers.
- Duration: Up to 5 years.
- Example: Artecoll, made of 20% PMMA microspheres suspended in a bovine collagen solution. Similarly, ArteFill (BellaFill) provides permanent volumization.
These biostimulatory fillers are summarised in the table below.
Understanding the physicochemical characteristics of fillers (like G′, cohesivity, and swelling) helps match the right product to each anatomical site and patient goal.
Indications and Filler Selection
Filler selection is tailored to anatomical region, patient goals, and filler characteristics, optimizing outcomes in volume restoration, wrinkle treatment, lip shaping, skin rejuvenation, and scar correction.
Successful filler outcomes rely on individualized treatment, matching product properties to anatomical demands, tissue dynamics, and patient goals. The selection of injectable fillers is guided by:
- Facial anatomy and injection depth
- Rheological properties of the filler (e.g., G′, cohesivity, extrusion force)
- Patient preferences and the desired results
Volume Restoration and Contour Enhancement
- Areas: Midface, temples, chin, jawline, and periorbital hollows.
- Use: Deep injections with volumizing fillers.
- Filler Characteristics: High G′, high viscosity, and good lift capacity.
- Preferred Fillers: HA, CaHA, or PCL.
- Outcome: Structural support, definition, and long-lasting contour improvement.
Fine Lines and Superficial Wrinkles
- Areas: Perioral lines, crow’s feet, and forehead lines.
- Use: Superficial placement using micro-aliquots.
- Filler Characteristics: Low G′ HA for smooth integration.
- Advantage: Maintains mobility and subtle correction without lumpiness.
Lips and Perioral Region
- Challenge: High mobility requires a filler that is both durable and flexible.
- Filler Characteristics: Medium G′, moderate cohesivity.
- Preferred Use: Soft HA fillers to enhance vermilion border, volume, and symmetry.
- Goal: Subtle augmentation with natural movement and minimized migration.
Skin Quality Improvement
- Indications: Crepey texture, dullness, and mild laxity.
- Filler Type: Biostimulatory agents such as PLLA and PCL.
- Mechanism: Stimulates neocollagenesis and elastin formation.
- Effect: Progressive improvement in skin tone, firmness, and elasticity.
- Note: Requires multiple sessions with clear patient education on gradual results.
Scar Correction
- Indications: Atrophic or rolling scars (e.g., acne scars).
- Filler Options: HA and CaHA for temporary lifting; PMMA for long-term correction.
- Technique: Subcision followed by subdermal bolus or fanning technique.
- Outcome: Smoother skin surface through elevation and stimulation of dermal remodeling.
Below is an anatomically based chart for filler selection.

Injection Technique of Fillers
Safe and effective filler injections require thorough patient evaluation, precise anatomical planning, and a strategic choice between needles and cannulas based on treatment goals and vascular risk.
Pre-Treatment Considerations
Proper assessment and preparation are foundational to successful outcomes.
- Medical History: Screen for allergies, medications, and autoimmune disorders.
- Contraindications: Avoid treatment in cases of infection, recent dental work, or active inflammation.
- Facial Assessment: Analyze symmetry, skin quality, and volume loss.
- Patient Expectations: Discuss goals clearly and manage expectations.
- Photography: Capture baseline images for reference and documentation.
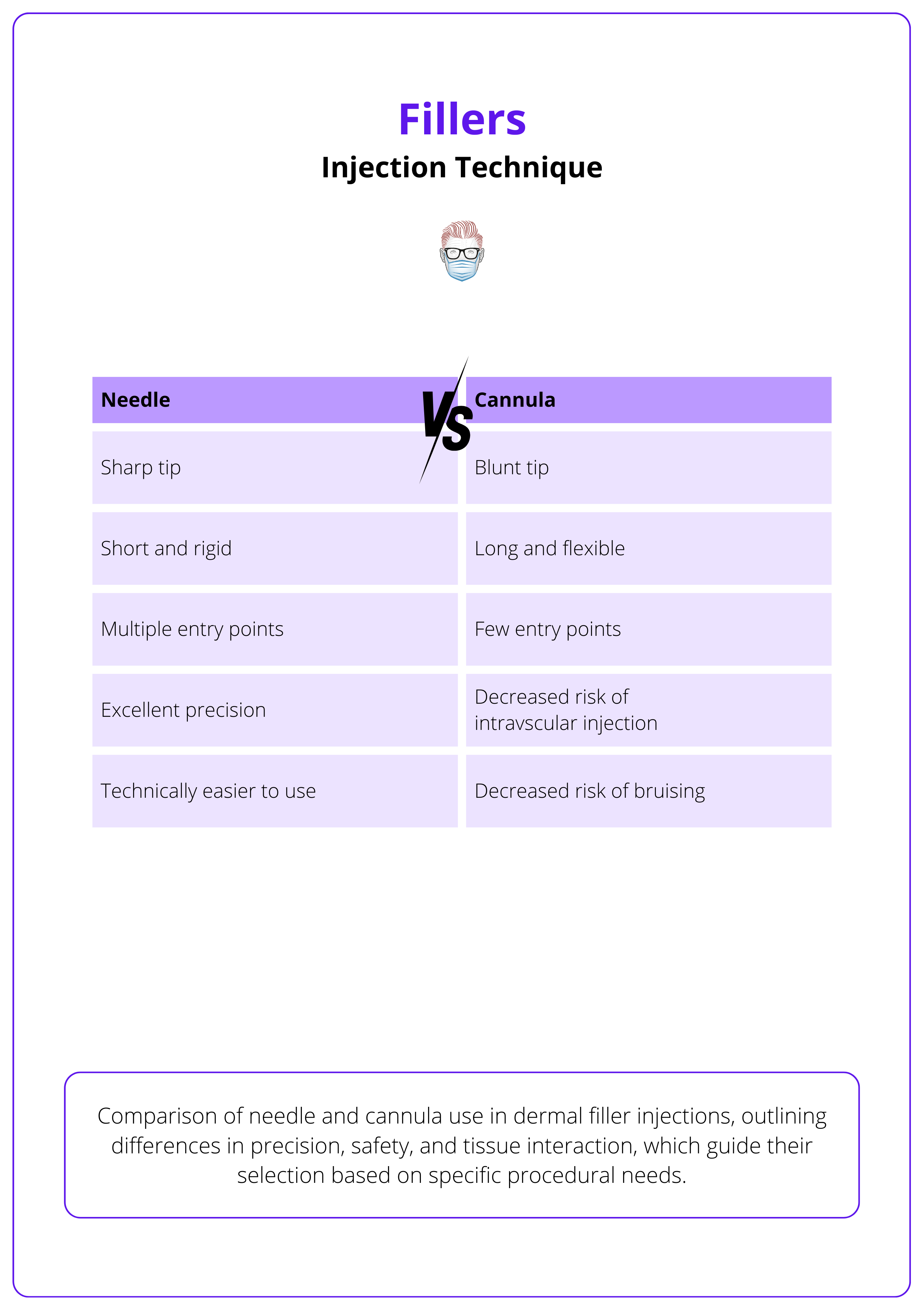
Needle and cannula selection is guided by anatomical location, filler rheology, and depth of injection.
- Needles: Allow precision in tight planes but carry higher vascular risk.
- Cannulas: Blunt tips reduce trauma and intravascular risk—ideal for high-risk areas.
- Anesthesia: Use topical agents, nerve blocks, or lidocaine-containing fillers; adjuncts include ice or vibration tools to enhance comfort.
The table below compares the use of needles and cannulas in dermal filler injections.
Injection Techniques by Facial Region
Upper Face
- Forehead and Glabella: Commonly considered danger zones. Inject at least 2 cm above the eyebrow, in a deep plane (supraperiosteal). Pay close attention to supratrochlear, supraorbital, and superficial temporal vessels (Ahn, 2024).
- Temples: Injections can be performed at various depths, from superficial to deep planes, depending on clinical indications. Care must be taken to avoid superficial temporal vessels and the middle temporal vein (De Maio, 2017).
Midface
- Tear Trough: Use of low G′ HA with minimal swelling potential. Injections should be deep, at the supraperiosteal level or underneath the orbicularis oculi muscle. avoiding the superficial vasculature (Sharad, 2012).
- Malar Region: Injections can be performed at various depths, either with bolus or linear threading techniques. Pay attention to infraorbital vessels and nerves.
- Nose: Injections should be performed on the midline, in a supraperiosteal/supraperichondral plane, keeping fingers on the sides to avoid filler lateral displacement. Be alert to the presence of anastomosis of periorbital vessels in the subcutaneous plane (Singh, 2019).
In nasal filler injections, use boluses of 0.05–0.1 mL and avoid exceeding 1 mL total, to minimize the risk of vascular compression and necrosis due to HA’s hydrophilic effect.
Lower Face
- Lips: Multiplanar approach using medium G′ HA for both volume and definition. Injection must consider dynamic movement and vascular anatomy.
- Chin and Jawline: Deep structural augmentation using high G′ fillers, often with a cannula for linear threading along mandibular border (Vazirnia, 2020).
- Nasolabial Folds and Marionette Lines: Combination of deep structural support and superficial softening using appropriate filler rheology.
Beyond facial applications, several fillers, especially biostimulatory agents such as PLLA or high-viscosity HA, are used for body contouring. Common off-label indications include the volumisation of hands, correction of skin laxity in the neck and décolleté, and gluteal augmentation using diluted or layered injection techniques.
Contraindications and Adverse Effects of Fillers
Injectable fillers are contraindicated in specific medical conditions and can cause adverse effects ranging from mild swelling to serious complications like vascular occlusion and, in rare cases, blindness
While fillers are generally safe and well-tolerated, patient selection and clinical vigilance are critical. A comprehensive understanding of contraindications and potential complications allows for safer outcomes and timely management when issues arise
Contraindications
Recognizing absolute and relative contraindications helps reduce the risk of complications and ensures ethical, informed treatment decisions.
- Absolute Contraindications:
- Allergy: Known hypersensitivity to any filler component.
- Infection: Active infection or inflammation at the treatment site.
- Pregnancy/Breastfeeding: Lack of safety data; avoid use.
- Severe Allergies/Anaphylaxis: High risk of adverse immune reactions.
- Uncontrolled Autoimmune Disease: Heightened risk of immune-related complications.
- Systemic Infections or Recent Dental Work: Increased infection risk (defer treatment for ≥2 weeks post dental procedures).
- Relative Contraindications:
- Anticoagulant or Antiplatelet Use: Higher risk of bruising or hematoma.
- Immunosuppression: Slower healing, increased infection risk.
- Psychological Concerns: Unrealistic expectations or body dysmorphic disorder may lead to dissatisfaction and over-treatment.
Adverse Effects
Adverse reactions can be classified by timing—immediate, early, or delayed. Most are self-limiting, but serious events require prompt intervention.
Immediate and Early Adverse Effects
- Local Reactions: Redness, swelling, tenderness, or bruising at the injection site.
- Nodules/Irregularities: Often due to superficial injection or improper technique.
- Hypersensitivity Reactions: Can range from localized swelling to generalized allergic response.
- Infection: Uncommon but potentially serious; may require antibiotics or drainage.
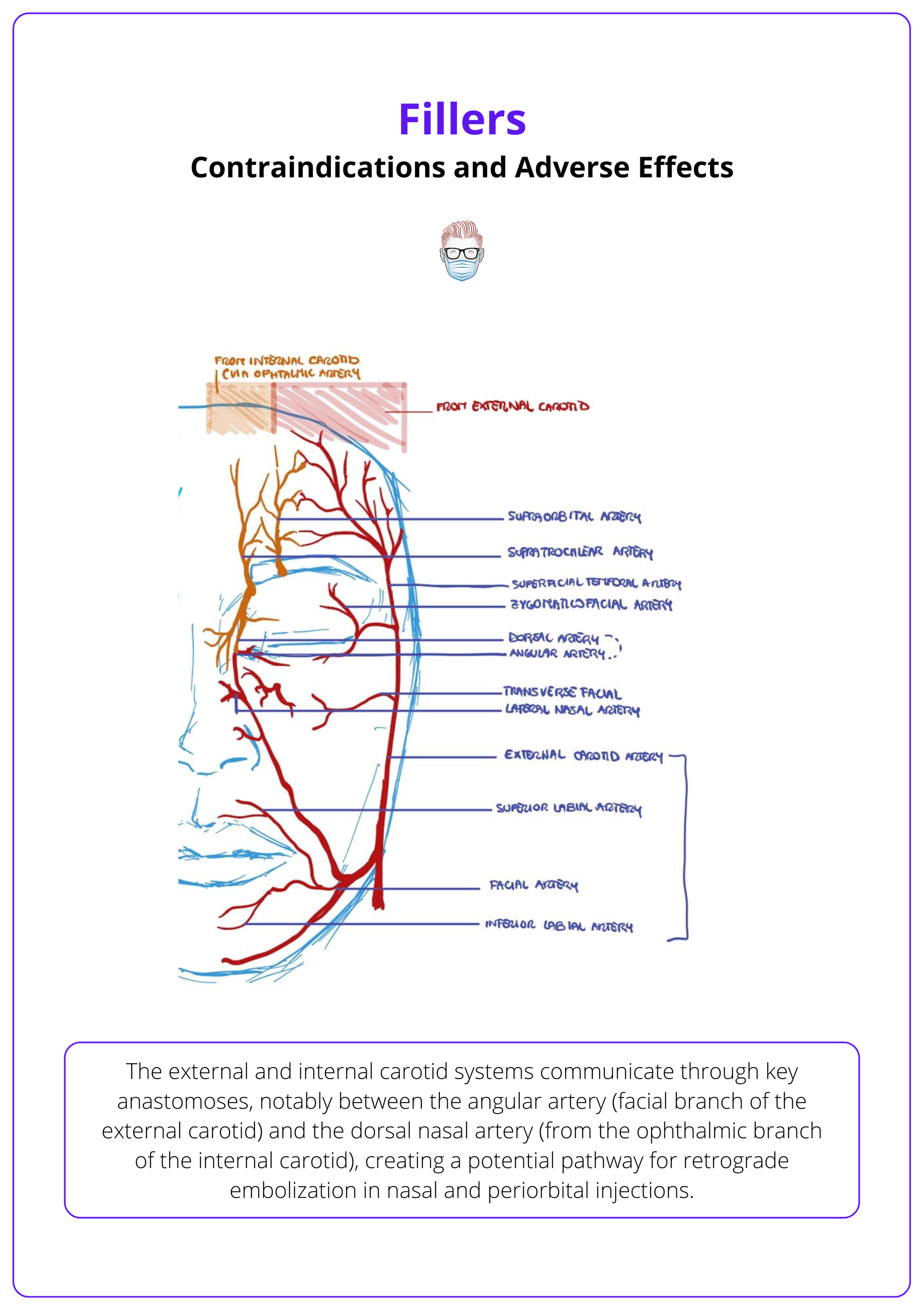
- Vascular Compromise:
- Cause: Intravascular injection or compression of vessels.
- Outcome: Ischemia, necrosis, or blindness (via retrograde embolization into the ophthalmic artery).
- Signs: Blanching, severe pain, livedo reticularis, delayed capillary refill.
- Emergency Protocol for HA Fillers:
- Immediate injection of hyaluronidase
- Warm compresses and massage
- Consider vasodilators like nitroglycerin paste
- Refer urgently if vision is affected
Delayed Adverse Effects
- Granulomas: Immune-mediated nodular inflammation that may appear weeks to months later.
- Filler Migration: Displacement of filler, often in highly mobile or overfilled areas.
- Tyndall Effect: Bluish discoloration from superficial HA placement, more common under thin skin.
The adverse effects of fillers are illustrated and described below.
Conclusion
1. Overview: Injectable fillers are essential tools in nonsurgical facial rejuvenation, offering immediate or progressive aesthetic enhancement depending on the product type.
2. Classes of Injectable Fillers: Fillers can be broadly classified as volumising agents or biostimulatory agents that stimulate collagen production for long-term improvement.
3. Filler selection and Indications: Optimal filler choice is guided by anatomical considerations, patient goals, and rheological properties. Common indications include contour restoration, fine line correction, lip enhancement, skin quality improvement, and scar revision.
4. Injection Techniques: Effective treatment requires thorough pre-injection assessment, anatomical planning, and the strategic use of needles or cannulas based on target depth and vascular risk.
5. Contraindications and Adverse Effects: Fillers are contraindicated in patients with allergies, infections, or uncontrolled systemic conditions. While most side effects are mild and self-limited, serious complications such as vascular occlusion and, rarely, blindness may occur.
Further Reading
- Juncan AM, Moisă DG, Santini A, Morgovan C, Rus LL, Vonica-Țincu AL, Loghin F. Advantages of Hyaluronic Acid and Its Combination with Other Bioactive Ingredients in Cosmeceuticals. Molecules. 2021 Jul 22;26(15):4429. doi: 10.3390/molecules26154429. PMID: 34361586; PMCID: PMC8347214.
- Guo J, Fang W, Wang F. Injectable fillers: current status, physicochemical properties, function mechanism, and perspectives. RSC Adv. 2023 Aug 10;13(34):23841-23858. doi: 10.1039/d3ra04321e. PMID: 37577103; PMCID: PMC10413051.
- Alster TS, West TB. Human-derived and new synthetic injectable materials for soft-tissue augmentation: current status and role in cosmetic surgery. Plast Reconstr Surg. 2000 Jun;105(7):2515-25; discussion 2526-8. doi: 10.1097/00006534-200006000-00034. PMID: 10845309.
- Watson D, Keller GS, Lacombe V, Fodor PB, Rawnsley J, Lask GP. Autologous fibroblasts for treatment of facial rhytids and dermal depressions. A pilot study. Arch Facial Plast Surg. 1999 Jul-Sep;1(3):165-70. doi: 10.1001/archfaci.1.3.165. PMID: 10937098.
- Rostan E. Collagen fillers. Facial Plast Surg Clin North Am. 2007 Feb;15(1):55-61, vi. doi: 10.1016/j.fsc.2006.11.001. PMID: 17317556.
- Kapoor KM, Chatrath V, Li CQ, Bertossi D. Pinch Anatomy of Forehead: An Injection Guide for Forehead Filler Treatment. Facial Plast Surg. 2022 Apr;38(2):156-162. doi: 10.1055/a-1730-8436. Epub 2022 Mar 10. PMID: 34983076.
- Ahn HS, Kim HM, Oh W, Yi KH, Kim J, Kim HJ. Singular entry point technique for forehead and temple filler augmentation: Anatomical and clinical perspectives. J Cosmet Dermatol. 2024 Oct;23(10):3195-3201. doi: 10.1111/jocd.16411. Epub 2024 Jun 4. PMID: 38837504.
- de Maio M, Swift A, Signorini M, Fagien S; Aesthetic Leaders in Facial Aesthetics Consensus Committee. Facial Assessment and Injection Guide for Botulinum Toxin and Injectable Hyaluronic Acid Fillers: Focus on the Upper Face. Plast Reconstr Surg. 2017 Aug;140(2):265e-276e. doi: 10.1097/PRS.0000000000003544. PMID: 28746271.
- Sharad J. Dermal Fillers for the Treatment of Tear Trough Deformity: A Review of Anatomy, Treatment Techniques, and their Outcomes. J Cutan Aesthet Surg. 2012 Oct;5(4):229-38. doi: 10.4103/0974-2077.104910. PMID: 23378704; PMCID: PMC3560162.
- Singh S. Practical Tips and Techniques for Injection Rhinoplasty. J Cutan Aesthet Surg. 2019 Jan-Mar;12(1):60-62. doi: 10.4103/JCAS.JCAS_137_18. PMID: 31057272; PMCID: PMC6484576.
- Vazirnia A, Braz A, Fabi SG. Nonsurgical jawline rejuvenation using injectable fillers. J Cosmet Dermatol. 2020 Aug;19(8):1940-1947. doi: 10.1111/jocd.13277. Epub 2019 Dec 31. PMID: 31889377.


