In this week's edition
- ✍️ Letter from P'Fella
Fellowship FOMO: Are we overselling the dream? - 🤓 The Sunday Quiz
How well do you know lymphedema? - 🖼️ Image of the Week
Stemmer’s sign: Affected vs. unaffected limb. - 🚑 Technique Tip
How to prepare for an LVA. - 🎙️ Behind the 'Fella
Taking suggestions for podcast guests! - 📖 What Does the Evidence Say
Does LVA actually work for lymphedema? - 🔥 Articles of the Week
Immediate lymphatic recon, consensus guidelines on lymphedema, & LVA in advanced stage: with 1 sentence summaries. - 💕 Feedback
Suggest ideas & give feedback!
A Letter from P'Fella
Fellowship FOMO: Are We Overselling the Dream?
Fellowships are a cornerstone of plastic surgery training — no question. They offer exposure to cutting-edge techniques, new surgical systems, and mentorship that can define a career. But here’s the thing: if every fellowship is “amazing,” then are we really being honest?
The truth is, fellowships have become a non-negotiable in our field. The days of jumping straight from residency to consultant life are fading. Now, if you don’t do a fellowship, you’re the outlier. While some fellowships truly deliver on the promise of mastery and independence, others? They’re just expensive gap years dressed up as training.
The Fellowship Illusion
Why does every fellowship get hyped?
- No one wants to admit theirs was a letdown - Who’s going to say, “I wasted a year doing cases I could’ve done as a senior resident”?
- Institutions sell prestige - Whether it’s high-volume trauma, elite aesthetics, or reconstructive giants, every program has a PR machine.
- The unspoken rule - Say good things, or risk burning bridges.
But let’s be real — fellowships are not created equal. The best ones give you autonomy, technical finesse, and a global perspective on plastic surgery. The worst? You’re a glorified assistant, running clinics while someone else gets the real experience.
So, Was It Worth It?
If fellowships are essential, then we need to start talking about which ones are actually worth it. So let’s cut through the fluff.
Drop your answers below. Let’s separate the true gold-standard fellowships from the ones running on reputation alone.
With love,
P'Fella ❤️
The Sunday Quiz
How Well Do You Know Lymphedema?
Welcome to the next round of The Weekly Quiz.
Each edition of thePlasticsPaper includes a quiz question designed to challenge and engage our readers. Keep your wits about you and join in every week — the winner at the end of six rounds will earn you a one-year subscription to thePlasticsPro.

Image of the Week
Stemmer’s Sign: Affected vs. Unaffected Limb
In this section, we feature an anatomical illustration. This week, we're looking at Stemmer’s sign, which is considered pathognomic for the presence of lymphedema.
In unilateral lower extremity lymphedema, the affected limb shows an inability to ‘tent’ the interdigital skin fold, unlike the normal limb (A). This finding is considered pathognomonic for lymphedema.

Technique Tip
How to Prepare for an LVA
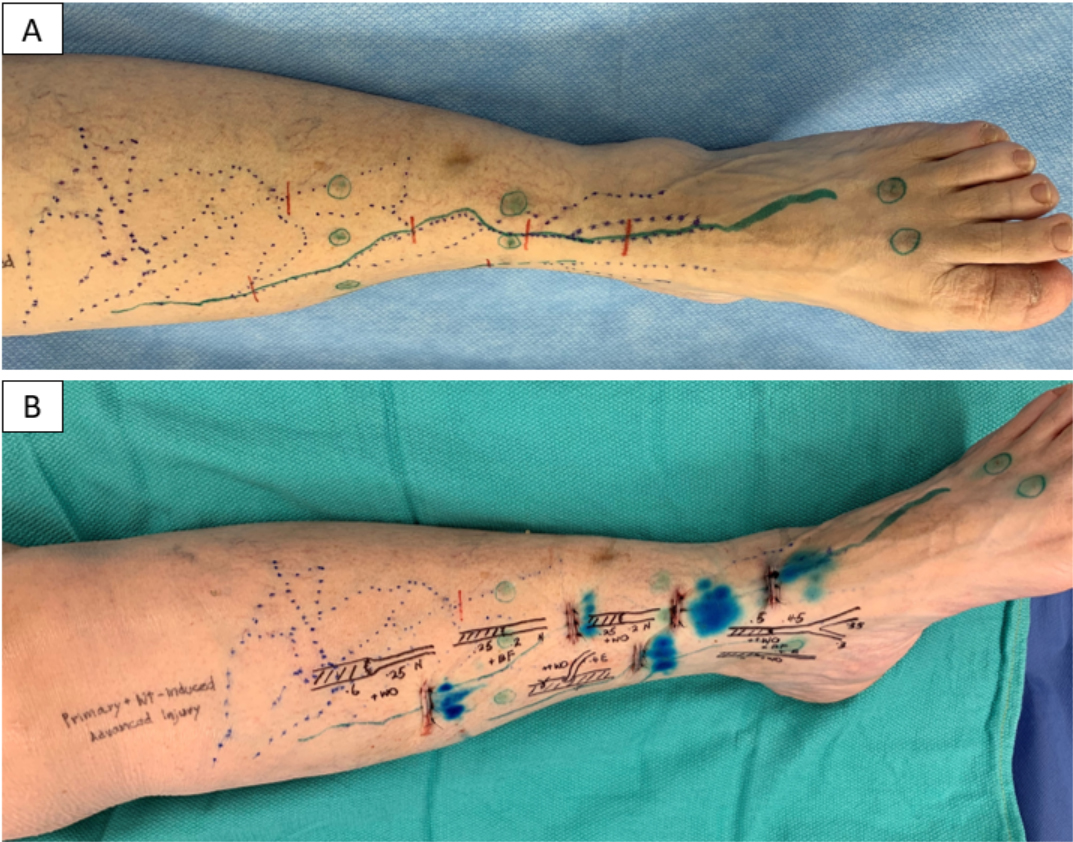
This week’s technique focuses on LVA incision planning.
(A) Lymphatic channels (solid green) are mapped with ICG lymphography, and veins (dotted blue) with an infrared vein finder. Incisions (2–3 cm) are placed where veins and lymphatics intersect (red lines). ICG injection sites (green circles) follow a distal-to-proximal sequence.
(B) Post-op image shows selected venules and lymphatics at each incision, with diagrams of anastomotic configurations. Blue staining from isosulfan blue enhances lymphatic visualization.
Behind the 'Fella
Give Us Your Podcast Guest Suggestions!
We're setting up an exciting new season of exclusive team meetings, where we take you behind the scenes of the platform and discuss hot topics in plastic surgery with our fellows — this time with some new features in the mix!
If you could have a conversation with one person in plastic surgery, who would it be?
What Does the Evidence Say?
Does LVA Actually Work for Lymphedema?
Factors influencing success include early-stage lymphedema, upper extremity location, and discontinuation of conservative treatment post-surgery (Klingelhoefer et al., 2019). The surgeon's experience does not significantly impact outcomes, although proficiency increases over time (Nicolás Pereira et al., 2018). Various techniques, such as sleeve-in anastomosis, have demonstrated efficacy (Chung et al., 2019).
Articles of the Week
3 Interesting Articles with 1 Sentence Summaries
Immediate lymphatic reconstruction reduces secondary lymphedema risk after lymph node surgery, with LYMPHA showing promising outcomes.
Evidence supports lymphovenous bypass and vascularized lymph node transfer as effective for lymphedema management, though optimal treatment and long-term efficacy remain uncertain.
Preoperative imaging can identify functional lymphatics in advanced lower extremity lymphedema, enabling lymphovenous anastomosis to reduce limb volume and cellulitis incidence.


