Summary Card
Overview
Autologous fat grafting is the transfer of adipose tissue to correct volume and contour abnormalities in reconstructive and aesthetic surgery, leveraging its biocompatibility and regenerative potential.
Basic Principles
Fat grafting transfers adipocytes, preadipocytes, and stromal tissue. Preadipocytes play a crucial role in graft survival and regeneration. Optimal outcomes depend on atraumatic surgical technique, processing, and controlled reinjection.
Indications
Fat grafting is used across multiple anatomical areas for volume restoration, contour correction, and tissue repair. It plays a key role in breast reconstruction, facial rejuvenation, and orthopedic applications.
Surgical Technique
The technique involves fat harvesting (syringe or suction), processing (sedimentation, filtration, or centrifugation), and injection into the recipient site.
Complications
Fat grafting complications can occur at both the recipient and donor sites. Issues include fat resorption, necrosis, embolism, infection, and aesthetic deformities.
Primary Contributor: Benedetta Agnelli, Educational Fellow
Verified by thePlasticsFella ✅
Overview of Fat Grafting
Autologous fat grafting is the transfer of adipose tissue to correct volume and contour abnormalities in reconstructive and aesthetic surgery, leveraging its biocompatibility and regenerative potential.
Fat grafting, also known as lipofilling, is the free, non-vascularized transplantation of adipose tissue. It is widely used in reconstructive and aesthetic surgery due to it's favourable characteristics:
- Biocompatibility: Uses the patient’s own tissue, eliminating rejection risk.
- Low Immunogenicity: Reduce inflammatory response & foreign body reactions.
- Cost-Effectiveness: Avoids synthetic fillers and implant-related complications.
- Accessibility and Versatility: Adaptable to multiple anatomical regions.
The primary goal of fat grafting is long-term volume maintenance, though its main limitation remains the unpredictable resorption of the graft over time.
The first adipose tissue transfer was reported by Neuber et al. in 1893, using forearm fat to correct a facial scar, achieving excellent aesthetic results.
Basic Principles of Fat Grafting
Fat grafting involves the transfer of adipocytes, preadipocytes, and stromal tissue. Preadipocytes play a critical role in graft survival and regeneration. Optimal outcomes depend on an atraumatic surgical technique, proper fat processing, and controlled reinjection.
Biology of Adipose Tissue
Fat grafting transfers a mixture of adipocytes, preadipocytes, and surrounding stromal tissue. The biological components of fat grafting contribute significantly to graft survival and tissue regeneration.
- Adipocytes (Mature Fat Cells): These cells provide volume but are highly susceptible to ischemia, leading to potential cell loss after transplantation.
- Preadipocytes (Adipogenic Precursor Cells): These adipose-derived stem cells tolerate ischemia better than mature adipocytes, enabling:
- Survival and differentiation into new adipocytes.
- Stimulation of angiogenesis.
- Enhanced long-term graft retention.
- Stromal Vascular Fraction (SVF): This fraction contains mesenchymal stem cells (MSCs) and other regenerative cells that promote:
- Tissue repair by differentiating into adipocytes or other supportive cells.
- Angiogenesis by releasing vascular growth factors.
- Improved graft integration by interacting with local tissue.
The use of SVF and MSCs in fat grafting remains under research and is not yet FDA-approved for routine clinical use.
Factors Affecting Graft Retention
Fat graft survival is dependent on proper revascularization. Initially, fat grafts rely on plasmatic diffusion for nourishment before new vascular networks form.
Eto's Three-Zone Survival Theory (2012)
Fat grafts follow a predictable survival pattern based on oxygenation levels:
- Survival Zone (Outer Layer): Well-oxygenated; adipocytes and adipose-derived stem cells (ASCs) survive.
- Regenerative Zone (Intermediate Layer): Adipocytes undergo ischemic death, but ASCs survive, differentiate, and promote angiogenesis.
- Necrotic Zone (Central Core): Poorly vascularized; cells undergo resorption or fibrosis.
Revascularization Process:
- Starts within 48 hours, progressing from the periphery inward.
- ASCs resist ischemia better than adipocytes, playing a key role in regeneration.
- Adipogenesis (fat cell formation) continues for up to 3 months, while phagocytosis of dead adipocytes lasts for weeks.
The image below illustrates the three-zone survival for fat grafts.
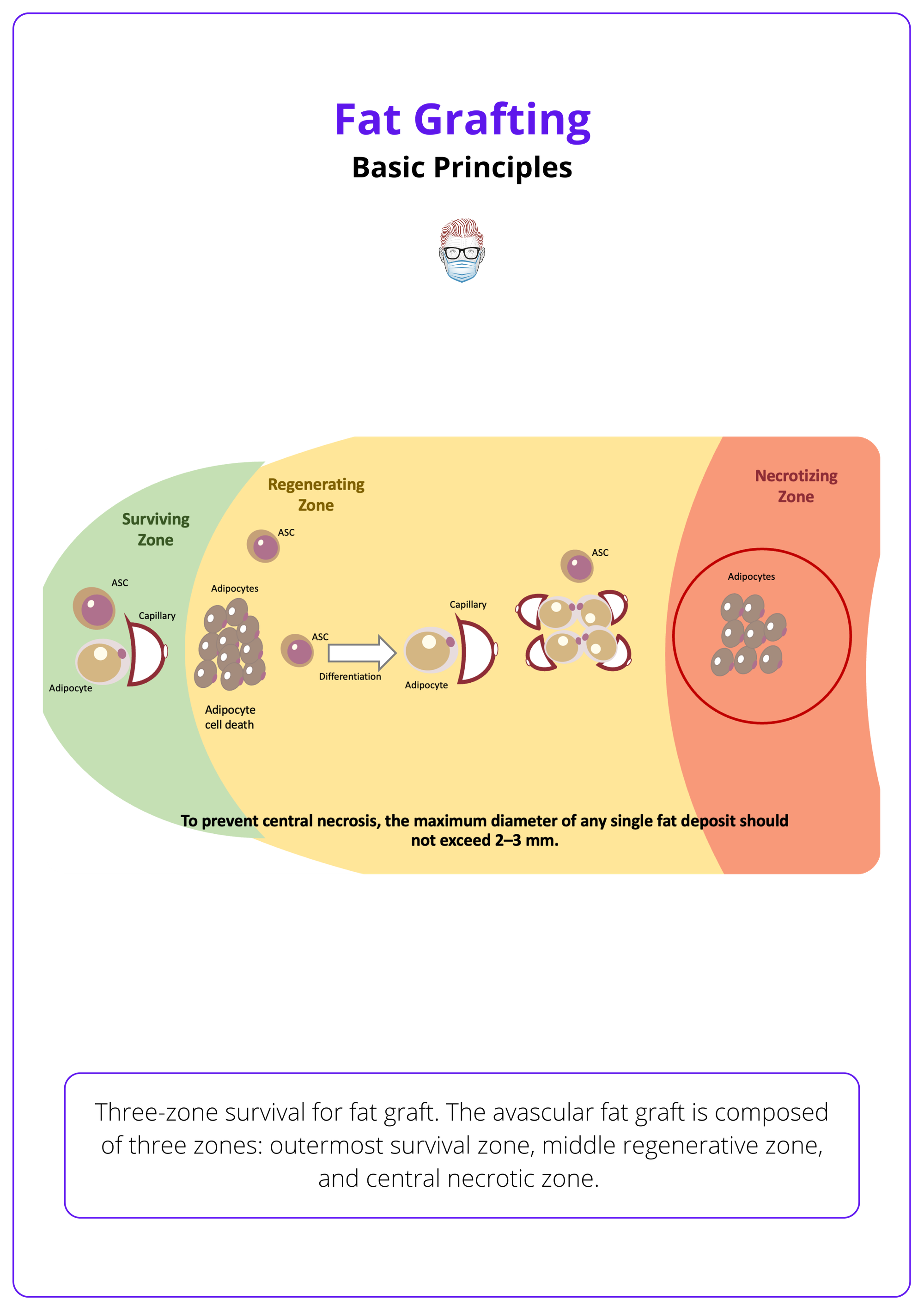
Adipose-derived stem cells (ASCs) can survive up to three days in severe ischemic conditions (Shih, 2020).
Enhancing Graft Retention
Three primary steps can significantly improve fat graft survival:
- Atraumatic Harvesting: Gentle liposuction techniques minimize damage to adipocytes and maintain donor site integrity.
- Proper Processing: Purification methods (e.g., centrifugation or filtration) remove contaminants like blood and oil, improving graft viability.
- Optimized Reinjection: Controlled injection techniques in small aliquots enhance vascular integration and prevent necrotic cyst formation.
The image below shows properly processed fat grafts prepared for injection.
Larger volumes injected at once may lead to central necrosis, reducing the effectiveness of the graft.
Indications for Fat Grafting
Fat grafting is used across multiple anatomical areas for volume restoration, contour correction, and tissue repair. It plays a key role in breast reconstruction, facial rejuvenation, and emerging orthopedic applications.
Fat grafting is widely utilised across multiple anatomical regions for both reconstructive and aesthetic purposes. It is commonly used in three main domains:
- Aesthetic Enhancement (Breast, Buttocks, Face, Hands, Genitalia)
- Reconstructive Applications (Post-surgical corrections, trauma, and congenital conditions)
- Regenerative & Emerging Applications (Orthopedics, scar therapy, radiation damage)
Aesthetic Enhancement
Fat grafting is a preferred method for natural soft tissue augmentation due to its biocompatibility and lifelong integration.
- Breast Augmentation: Enhances volume naturally without implants.
- Brazilian Butt Lift (BBL): Augments the buttocks for improved shape and contour.
- Facial Volume Restoration: Treats age-related volume loss, hollowed eyes, and sunken cheeks.
- Lip & Malar Augmentation: Subtly enhances lip fullness and cheek projection.
- Hand Rejuvenation: Improves skin texture and volume, reducing visibility of veins and tendons.
- Genital Enhancement: Used for penile enlargement and labial augmentation.
Reconstructive Applications
Fat grafting plays a critical role in correcting defects and restoring soft tissue integrity in reconstructive surgery.
- Post-Mastectomy & Lumpectomy Corrections: Fills contour irregularities in breast reconstruction.
- Nipple Reconstruction: Enhances soft tissue volume post-mastectomy.
- Congenital Breast Deformities: Corrects conditions such as micromastia, tuberous breast, and Poland’s syndrome.
- Post-Traumatic & Surgical Defect Repair: Restores facial and body contours after accidents or surgeries.
- Correction of Liposuction Irregularities: Treats asymmetries and indentations from body contouring procedures.
Regenerative & Emerging Applications
Fat grafting is increasingly studied for its regenerative potential, particularly in scar treatment, orthopedic medicine, and radiation damage repair.
- Scar Therapy: Improves elasticity and softens hypertrophic or retracting scars.
- Radiation-Induced Skin Damage: Enhances tissue quality and hydration.
- Cartilage & Tendon Regeneration: Investigated for orthopedic conditions such as osteoarthritis and joint repair.
Contraindications for Fat Grafting
Absolute Contraindications
- Active Infection or Inflammation: Increases risk of fat necrosis and poor healing.
- Severe Vascular Compromise: conditions like peripheral artery disease may lead to graft failure.
Relative Contraindications
- Uncontrolled Systemic Diseases: Diabetes, cardiovascular disease, or autoimmune disorders may impair healing.
- History of Extensive Radiation Therapy: Compromised blood supply can reduce fat graft viability.
- Psychological Considerations: Unrealistic expectations or body dysmorphia should be carefully evaluated.
- Insufficient Donor Fat: Patients with low body fat may require alternative augmentation options.
Combining fat grafting with platelet-rich plasma (PRP) or stem cell-enriched fat is an emerging technique that may improve graft survival and integration.
Surgical Technique of Fat Grafting
Fat grafting involves three main steps: fat harvesting (via suction, syringe aspiration, or excision), processing (sedimentation, filtration, or centrifugation), and injection into the recipient site using precise volumetric techniques.
Step 1: Fat Harvesting
The goal of fat harvesting is to extract adipocytes while minimizing trauma to maximize graft survival. The deep subcutaneous fat layer is the ideal donor site due to its high adipocyte concentration and minimal contamination with blood, debris, and dermal appendages (Sommer, 2000).
Suction-Assisted Fat Harvest (Liposuction-Based)
- Negative-pressure liposuction enables large-volume fat harvesting.
- Fast and efficient, but excess suction pressure may damage adipocytes, reducing viability.
Syringe Aspiration (Coleman Technique)
- 17G blunt cannula minimizes cellular trauma.
- 10-mL Luer-Lok syringe enables controlled low-pressure aspiration.
- Crosshatch technique ensures uniform fat retrieval.
- Ideal for small-volume grafting (e.g., facial fat grafting) (Coleman, 2001).
Surgical Excision
- Precision harvesting for small areas.
- Ideal for autologous fat banking or when liposuction is unsuitable.
Tumescent Infiltration Techniques
Tumescent solutions reduce bleeding, bruising, and tissue trauma, facilitating fat extraction. Options include:
- Dry Technique: No infiltration; higher bleeding risk.
- Wet Technique: Minimal fluid infiltration.
- Super-Wet Technique: Fluid volume approximates aspirated fat volume.
- Tumescent Technique: Large volumes of fluid with epinephrine and lidocaine for pain control and vasoconstriction.
The table below summarises the surgical technique of fat grafting.
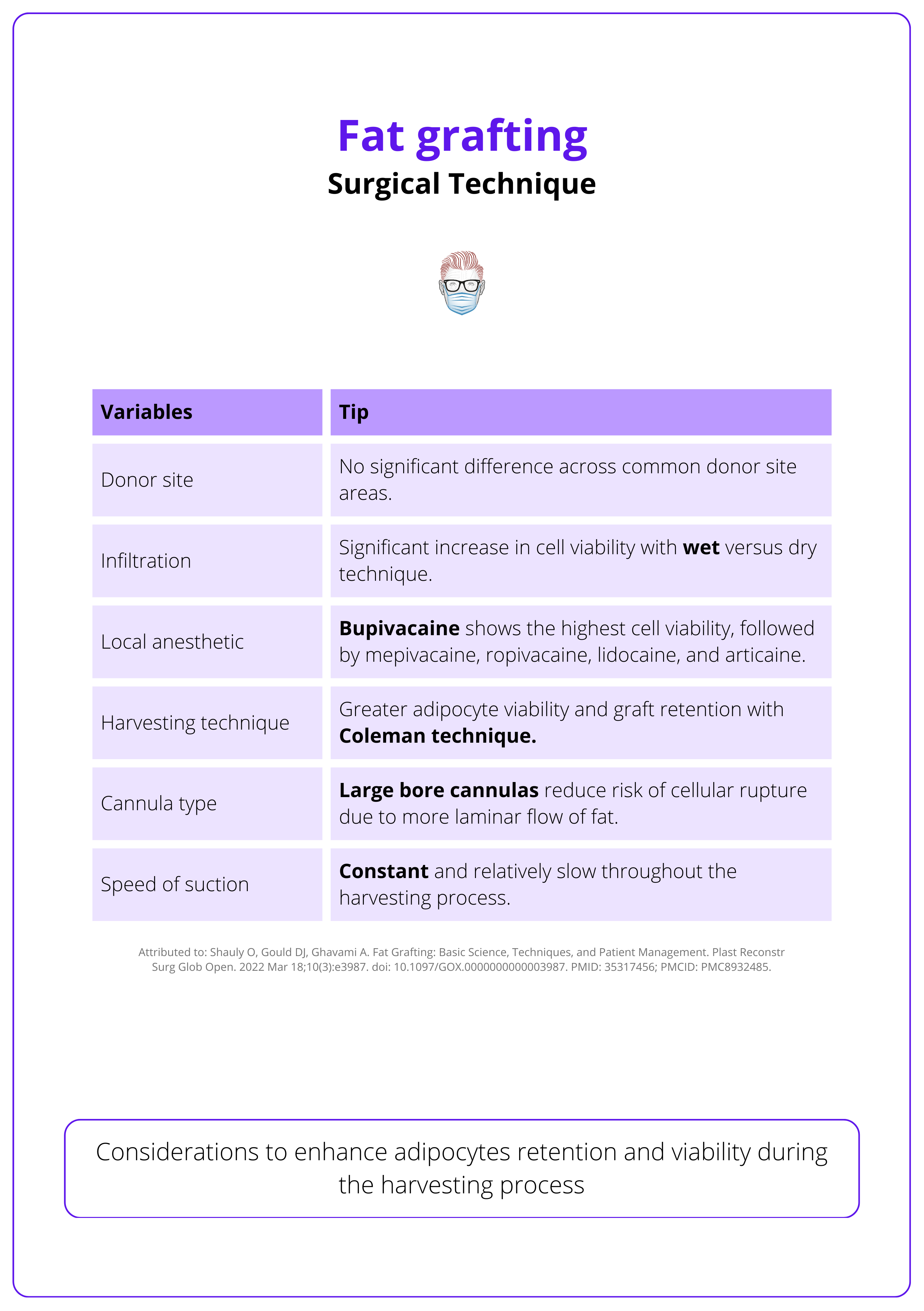
Maintain continuous negative pressure in the harvesting syringe, keeping the plunger at the 2–3 cc mark to avoid excessive force.
Step Two: Processing
After fat harvesting, processing is essential to remove impurities such as oil, blood, and inflammatory byproducts, ensuring optimal graft survival. This is achieved through three primary methods: Sedimentation, Filtration, and Centrifugation.
Sedimentation
This is the the least traumatic method and has features of:
- Gravity separation or decantation (layers based on density over time).
- Retains fewer stromal and stem cell components
- Less effective at eliminating pro-inflammatory substrates
Filtration
Effectively removes contaminants and inflammation and has features of:
- Preservation of viable adipocytes and adipose-derived MSCs.
- Can be manual or automated.
- Can be integrated with washing (normal saline or lactated Ringer’s solution).
Centrifugation
Involves loading lipoaspirate into 10-mL Luer-Lok syringes and centrifuging at 3000 rpm for 3 minutes. It is widely regarded as the gold standard because:
- Precise separation of graft components based on density.
- Optimisation of the concentration of adipocytes and MSCs.
This process yields four distinct layers,
- Upper Oil Layer: Oil (ruptured fat cells) – discarded.
- Middle Fat Layer: Viable adipocytes – used for grafting.
- Lower Aqueous Layer: Blood, residual anesthetic, and water – discarded.
- SVF (Stromal Vascular Fraction) Pellet: Rich in stem cells, retained in specific protocols.
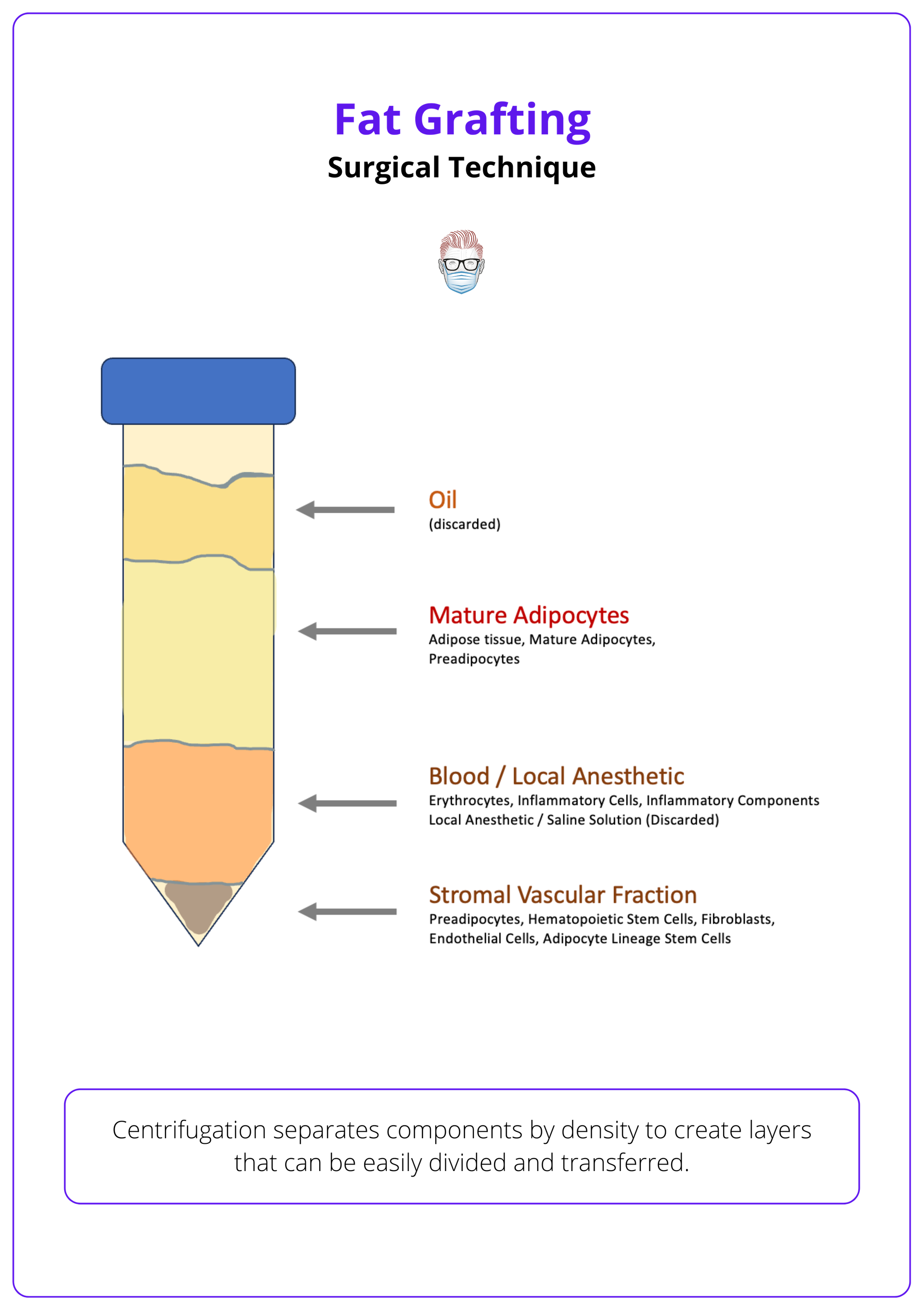
Microfat (≥0.7 mm cannulas) allows precise fat placement in delicate areas, while Nanofat (filtered into a liquid suspension) is rich in stem cells and ideal for skin rejuvenation, not volumization! (Tonnard, 2013).
Step 3: Engraftment (Injection & Placement)
The final step involves precise injection of purified fat into the recipient site.
Injection Technique
- A small incision is made to match the cannula diameter.
- Fat is injected in small aliquots (droplets) upon withdrawal to maximize oxygenation and perfusion.
- Fat is distributed in a crosshatch pattern with long radial passes from multiple angles.
- Digital manipulation is used to smooth out clumps or minor irregularities.
For large-volume fat transfer, 10–60 mL syringes improve efficiency, radial injections ensure even distribution, and intramuscular placement enhances graft survival.
Cannula Selection
- Small-gauge cannulas (e.g., 18G–22G) minimize trauma to the recipient site.
- Larger cannulas (e.g., 14G–16G) may improve adipocyte survival by reducing shear forces.
- Cannula choice depends on recipient site anatomy, fat viscosity, and injection depth.
Overcorrect (by ~20%) to account for postoperative resorption of tumescent fluid and partial graft loss.
Complications of Fat Grafting
Fat grafting complications can occur at both the recipient and donor sites, including fat resorption, necrosis, embolism, infection, and aesthetic deformities.
Recipient Site Complications
- Fat Resorption & Volume Fluctuation: Graft volume may change over time, requiring at least 6 months before assessing permanent results or considering additional grafting.
- Aesthetic Deformities: Uneven fat distribution can occur due to poor technique or over-injection in one area.
- Fat Necrosis & Calcifications: Common in breast reconstruction, sometimes leading to microcalcifications that mimic malignancy on mammograms; an experienced radiologist can differentiate them.
- Pseudocyst Formation: Breakdown of grafted fat may cause cystic fluid collections, which may require aspiration or excision if symptomatic.
- Fat Embolism & Vascular Complications: Arterial occlusion can lead to blindness, stroke, or skin necrosis in rare cases.
- Lipoid Meningitis: A rare condition where fat unintentionally migrates into the cerebrospinal fluid (CSF).
Donor Site Complications
- Aesthetic Deformities: Uneven fat removal may result in contour irregularities.
- Hematoma & Seroma Formation: Fluid or blood accumulation may require drainage.
- Infection & Poor Healing: Improper wound care or preexisting conditions can increase infection risk.
Fat graft volume fluctuates with weight changes! Since grafted fat cells retain metabolic function, weight gain or loss can affect the final contour.
Conclusion
1. Overview: Autologous fat grafting transfers adipose tissue to correct volume and contour abnormalities in reconstructive and aesthetic surgery. It is biocompatible, low-risk, and widely used for soft tissue augmentation.
2. Basic Principles: Fat grafting transfers adipocytes, preadipocytes, and stromal vascular fractions (SVF), with preadipocytes promoting angiogenesis and tissue regeneration.
3. Indications: Used for volume restoration and contour correction in breast reconstruction, facial rejuvenation, gluteal augmentation, hand rejuvenation, scar treatment, and emerging orthopedic applications.
4. Surgical Technique: The procedure involves harvesting (syringe aspiration or suction-assisted liposuction), processing (sedimentation, filtration, or centrifugation), and reinjection (small aliquots, multiplanar technique, controlled deposition).
5. Complications: Risks include fat resorption, necrosis, pseudocyst formation, embolism (potentially causing blindness or stroke), donor site contour irregularities, and infections.
6. Outcomes: Fat survival varies; resorption occurs over months. Permanent volume is assessed after ~6 months, with overcorrection (~20%) recommended to account for initial loss.
Further Reading
- Shauly O, Gould DJ, Ghavami A. Fat Grafting: Basic Science, Techniques, and Patient Management. Plast Reconstr Surg Glob Open. 2022 Mar 18;10(3):e3987. doi: 10.1097/GOX.0000000000003987. PMID: 35317456; PMCID: PMC8932485.
- Coleman SR. Structural fat grafts: the ideal filler? Clin Plast Surg. 2001 Jan;28(1):111-9. PMID: 11248861.
- Coleman SR, Katzel EB. Fat Grafting for Facial Filling and Regeneration. Clin Plast Surg. 2015 Jul;42(3):289-300, vii. doi: 10.1016/j.cps.2015.04.001. PMID: 26116934.
- Sommer B, Sattler G. Current concepts of fat graft survival: histology of aspirated adipose tissue and review of the literature. Dermatol Surg. 2000 Dec;26(12):1159-66. PMID: 11134994.
- Tonnard P, Verpaele A, Peeters G, Hamdi M, Cornelissen M, Declercq H. Nanofat grafting: basic research and clinical applications. Plast Reconstr Surg. 2013 Oct;132(4):1017-1026. doi: 10.1097/PRS.0b013e31829fe1b0. PMID: 23783059.
- Trepsat F. Lipostructure du tiers moyen du visage [Midface reshaping with micro-fat grafting]. Ann Chir Plast Esthet. 2009 Oct;54(5):435-43. French. doi: 10.1016/j.anplas.2009.03.008. Epub 2009 May 15. PMID: 19446945.
- Mashiko T, Yoshimura K. How does fat survive and remodel after grafting? Clin Plast Surg. 2015 Apr;42(2):181-90. doi: 10.1016/j.cps.2014.12.008. Epub 2015 Jan 29. PMID: 25827562.
- Eto H, Kato H, Suga H, Aoi N, Doi K, Kuno S, Yoshimura K. The fate of adipocytes after nonvascularized fat grafting: evidence of early death and replacement of adipocytes. Plast Reconstr Surg. 2012 May;129(5):1081-1092. doi: 10.1097/PRS.0b013e31824a2b19. PMID: 22261562.
- Shih L, Davis MJ, Winocour SJ. The Science of Fat Grafting. Semin Plast Surg. 2020 Feb;34(1):5-10. doi: 10.1055/s-0039-3402073. Epub 2020 Feb 15. PMID: 32071573; PMCID: PMC7023968.
- Schiraldi L, Sapino G, Meuli J, Maruccia M, Cherubino M, Raffoul W, di Summa PG. Facial Fat Grafting (FFG): Worth the Risk? A Systematic Review of Complications and Critical Appraisal. J Clin Med. 2022 Aug 11;11(16):4708. doi: 10.3390/jcm11164708. PMID: 36012947; PMCID: PMC9410081.
- Ørholt M, Larsen A, Hemmingsen MN, Mirian C, Zocchi ML, Vester-Glowinski PV, Herly M. Complications after Breast Augmentation with Fat Grafting: A Systematic Review. Plast Reconstr Surg. 2020 Mar;145(3):530e-537e. doi: 10.1097/PRS.0000000000006569. PMID: 32097306.
- Liao X, Zhou H, Deng T. The composition, function, and regulation of adipose stem and progenitor cells. J Genet Genomics. 2022 Apr;49(4):308-315. doi: 10.1016/j.jgg.2022.02.014. Epub 2022 Feb 28. PMID: 35240306.
- Duhoux A, Chennoufi M, Lantieri L, Hivelin M. Complications of fat grafts growth after weight gain: report of a severe diplopia. J Plast Reconstr Aesthet Surg. 2013 Jul;66(7):987-90. doi: 10.1016/j.bjps.2012.11.038. Epub 2012 Dec 24. PMID: 23270665.


