Summary Card
Extensor Tendon Anatomy
The extensor tendons form a complex system for coordinated finger, wrist, and thumb movement, divided into extrinsic (originating from the forearm) and intrinsic (within the hand) components.
Zones of Injury
The Kleinert and Verdan Classification divides extensor tendon injuries into seven zones based on anatomical location, later expanded to nine zones. The thumb has its own five-zone system.
Clinical Assessment
Assessing extensor tendon injuries involves a stepwise approach: evaluating the wound, function, and neurovascular status, complemented by specific tests such as Elson’s test.
Management
Extensor tendon injuries are managed nonoperatively or operatively, depending on severity, chronicity, and functional impairment. Local protocols may vary, and institutional guidelines should be consulted.
Primary Contributor: Dr Kurt Lee Chircop, Educational Fellow
Verified by thePlasticsFella ✅
Anatomy of Extensor Tendon Injuries
The extensor tendons form a complex system for coordinated finger, wrist, and thumb movement, divided into extrinsic (originating from the forearm) and intrinsic (within the hand) components.
The extensor tendons form a complex system that allows for coordinated movement of the fingers, wrist, and thumb. They are divided into extrinsic and intrinsic and terminal components (von Schroeder, 1997).
Extrinsic Extensor Tendons
The extrinsic extensor tendons begin in the posterior forearm, primarily at the lateral epicondyle of the humerus, and extend into the hand to control wrist and finger movements.
- Innervation: radial nerve, with most receiving their supply from its deep branch, the posterior interosseous nerve (PIN).
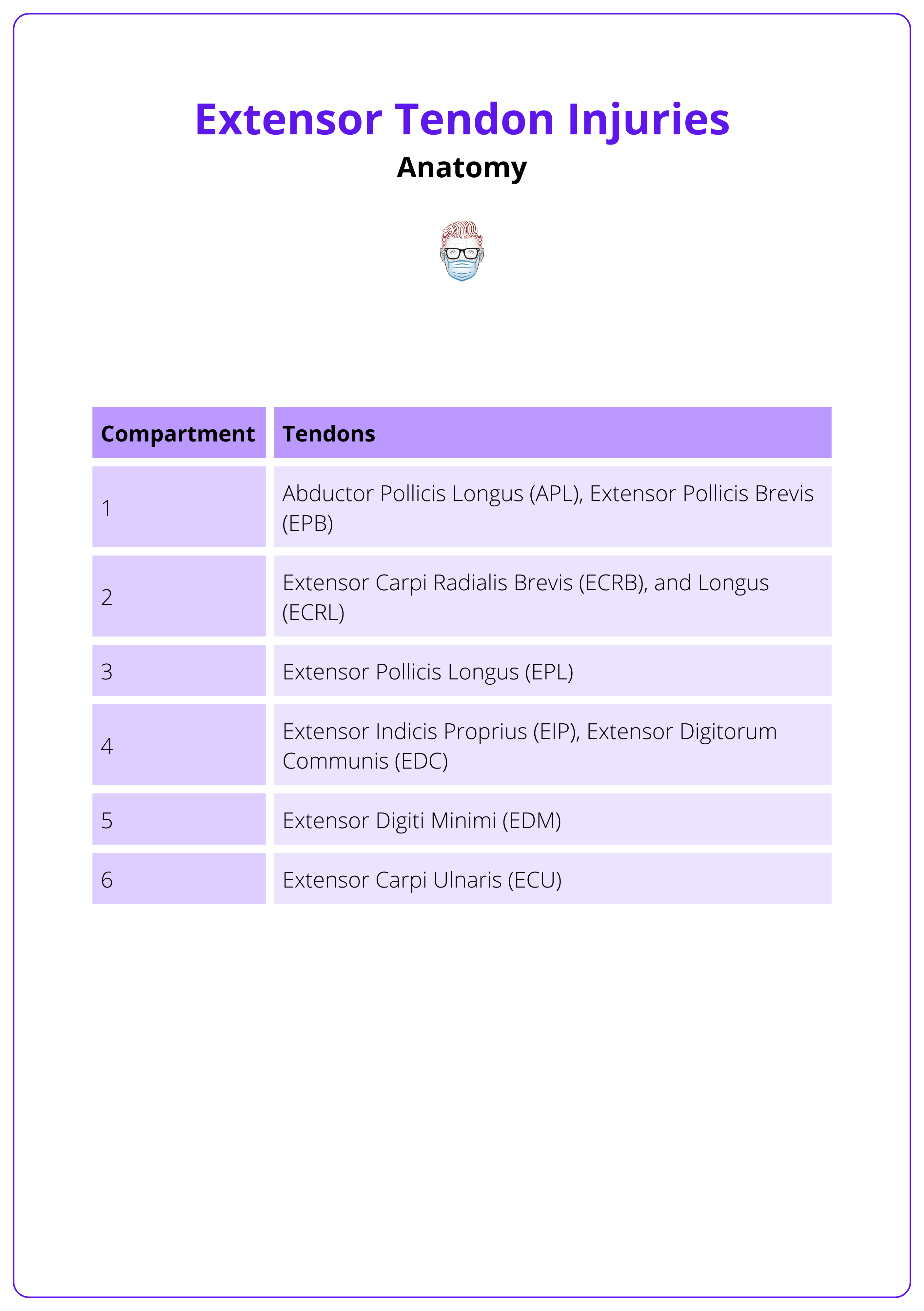
- Pathway: six dorsal compartments, each housed within a synovial sheath and secured by the extensor retinaculum—a fibrous band that prevents tendon bowstringing during movement (von Schroeder, 1997).
The layout of these six compartments is outlined below, each containing specific tendons that contribute to precise and coordinated hand function.
The EPL tendon winds around Lister’s tubercle, changing direction before inserting into the thumb’s distal phalanx. Ruptures often occur at this point due to attrition.
Intrinsic Extensor Mechanism
Intrinsic tendons originate entirely within the hand, while extrinsic tendons come from the forearm. Intrinsic and extrinsic tendons can insert into the extensor hood. Intrinsic tendons typically flex the MCP joints and extend the IP joints.
Lumbricals
- Function: Flex the MCP joints, extending the PIPJ and DIPJ
- Origin: From the tendons of flexor digitorum profundus.
- Insertion: Into the radial side of the extensor expansion on fingers 2–5.
Palmar and Dorsal Interossei
- Function: IP joint extension; dorsal interossei abduct & palmar interossei adduct fingers.
- Origin: From the metacarpal bones.
- Insertion: Into the lateral bands of the extensor expansion on fingers 2–5.
Thenar Muscles
Some intrinsic thumb muscles such as abductor pollicis brevis and adductor pollicis, partially insert into the extensor mechanism of the thumb. These attachments help fine-tune and stabilize thumb movements through the dorsal apparatus.
The extensor expansion is highlighted in the image below.
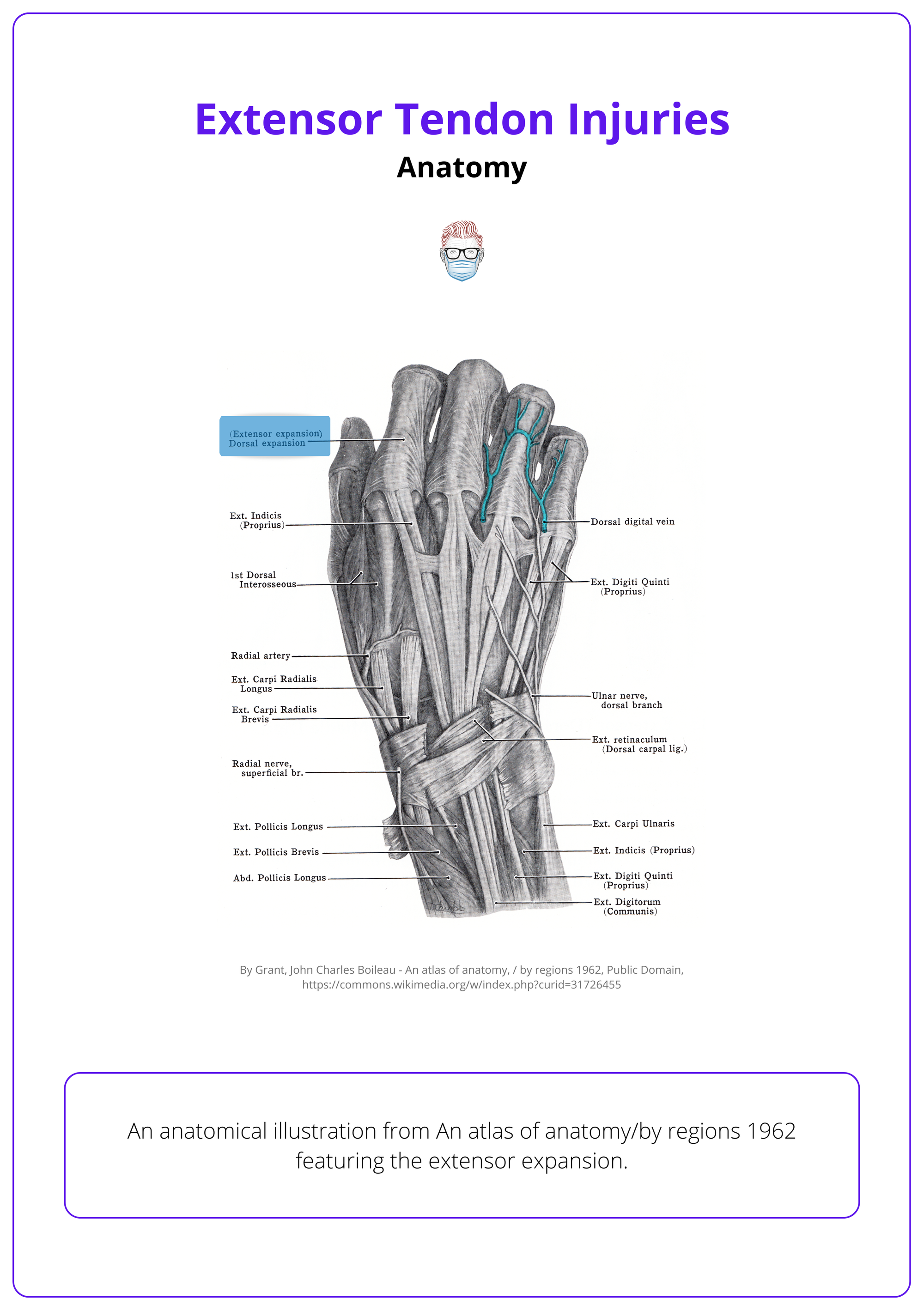
This common insertion site known as the extensor hood or extensor expansion, is a specialized connective tissue that allows multiple tendons to attach to the phalanges. It is stabilized by sagittal bands.
Terminal Extensor Tendons
Once both intrinsic and extrinsic tendons insert into the extensor hood, the extensor mechanism continues distally and divides into structures responsible for extending the finger joints.
- Central Slip: Passes over the middle phalanx and inserts at its base, extending the proximal interphalangeal (PIP) joint.
- Lateral Bands: Two bands run along either side of the finger and converge to insert at the base of the distal phalanx, enabling extension of the distal interphalangeal (DIP) joint.
- Oblique Retinacular Ligament: Runs from the proximal phalanx and flexor sheath to the lateral bands, linking PIP and DIP joint extension (Shrewsbury, 1977).
Juncturae Tendinum are fibrous links between extensor digitorum tendons that coordinate finger extension and prevent tendon retraction (Hirai, 2001).
Zones of Extensor Tendon Injury
The Kleinert and Verdan Classification divides extensor tendon injuries into seven zones based on anatomical location, later expanded to nine zones. The thumb has its own five-zone system.
The Kleinert and Verdan Classification divided extensor tendon injuries into 7 zones based on anatomical location, with 2 further zones added in later modifications (Kleinert, 1989). The thumb is divided into 5 zones in a similar manner.
The most commonly injured structures in each zone of the hand are summarised below.
- Zone I (DIP Joint): Mallet Finger.
- Zone II (Middle Phalanx): Tendon laceration or avulsion.
- Zone III (PIP Joint): Boutonnière Deformity.
- Zone IV (Proximal Phalanx): Extensor tendon rupture.
- Zone V (MCP Joint): "Fight bite," Sagittal Band Rupture.
- Zone VI (Metacarpals): Lacerations, EDC injuries.
- Zone VII (Wrist): Retinaculum injury, tendon bowstringing.
- Zone VIII (Distal Forearm): Muscle belly injuries.
- Zone IX (Proximal Forearm): Neuromuscular injuries.
These hand zones are illustrated below.
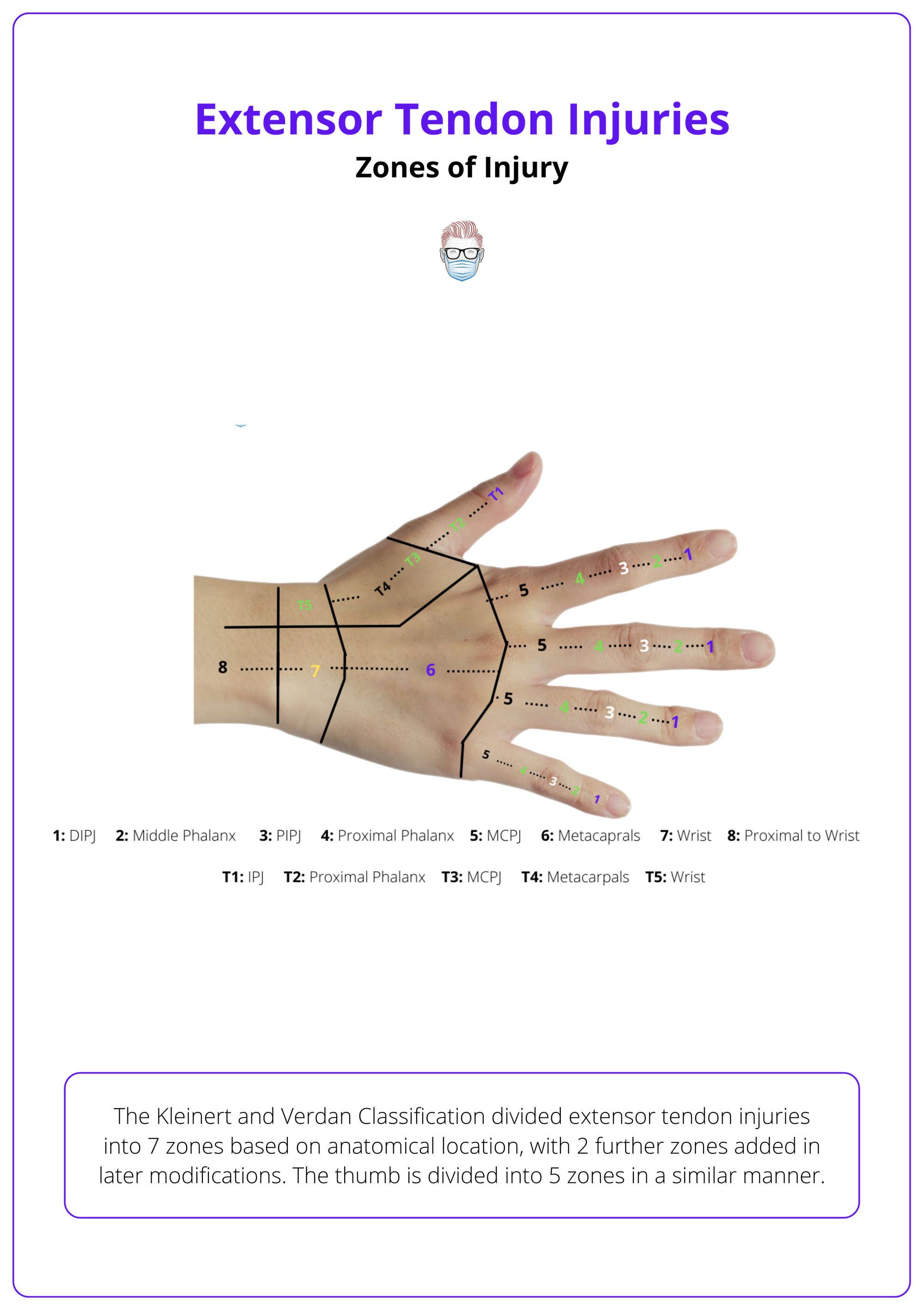
Odd numbered zones correspond to joints while even numbered zones correspond to bones starting from distal to proximal.
Clinical Assessment of Extensor Tendon Injuries
A systematic evaluation focusing on the wound, tendon function, and neurovascular integrity is critical in diagnosing extensor tendon injuries, with Elson’s test serving as a pivotal diagnostic tool for central slip injuries
Extensor tendon injuries, though often less complex than flexor tendon injuries, require careful assessment due to their intricate anatomy and potential for functional compromise.
History
Extensor tendon injuries occur through diverse mechanisms, from sharp trauma to underlying pathological conditions (Hanz, 2008; Matzon, 2010).
- Sharp Lacerations: Commonly caused by glass, knives, or industrial machinery, these clean-cut injuries may clearly transect tendons.
- Crush Injuries: Often resulting from door entrapment or machinery, these can involve deeper soft tissues including tendons and joints.
- Mallet Finger (Zone I): Results from forced flexion of an extended distal interphalangeal (DIP) joint, typically seen in sports.
- Sagittal Band Rupture (Zone V): Often results from forced extension of a flexed finger, which is common in contact sports. Suspect it if the MCP joint stays flexed with no active extension. Diagnosis is confirmed when the patient can’t initiate MCP extension but can hold it once passively extended.
- Closed Ruptures: Often seen in patients with rheumatoid arthritis or following attrition over implants, particularly the extensor pollicis longus (EPL) near Lister’s tubercle.
- "Fight Bite" Injuries (Zone V): Occur during clenched-fist impacts against teeth; high risk for infection and deep structural damage.
An extensor tendon injury of zone VI is illustrated in the image below.

Examination
A structured approach is essential in evaluating extensor tendon injuries to prevent misdiagnosis, especially in cases masked by compensatory mechanisms.
- Wound Assessment: Determines the affected tendon zone, as described below, and possible involvement of joint capsules or bones.
- Functional Testing: Assess each joint individually—look for extensor lag or inability to extend joints. Resisted Movement can uncover partial tendon injuries or imbalances.
- Palpation: A palpable defect or tenderness along the tendon path may indicate rupture or laceration.
- Neurovascular Examination: Full Sensory and Vascular Evaluation: To identify associated digital nerve or vessel injuries.
- Elson’s Test: Used to identify central slip injuries (distal to Zone III); a positive result is when the PIP joint cannot extend against resistance while the DIP remains rigid, indicating a central slip rupture (Hart, 1993). This is visualised below
Juncturae Tendinum allow compensation by adjacent tendons, potentially masking proximal injuries. Always test each finger in isolation (von Schroeder, 1997).
Investigations
While clinical examination is paramount, imaging complements the assessment, particularly in uncertain or chronic cases.
- X-rays: Avulsion Fractures and joint involvement, especially helpful in suspected bony mallet finger or joint misalignment.
- Ultrasound (US): Tendon integrity and fluid collections can visualize partial or complete ruptures and associated effusions.
- MRI: Detailed soft tissue evaluation, which is reserved for complex or delayed presentations; ideal for assessing retraction or chronic injuries (Colzani, 2016).
Management of Extensor Tendon Injuries
Extensor tendon injuries are managed either conservatively or surgically depending on the extent of damage, chronicity, and functional impairment, with local protocols guiding specific treatment decisions.
Management strategies for extensor tendon injuries hinge on several factors, including the zone of injury, tendon integrity, timing of presentation, and institutional protocols. While some injuries heal well with splinting alone, others require surgical intervention to restore function and prevent deformity (Griffin, 2012).
Non-operative Management
Conservative treatment remains effective for select extensor tendon injuries, particularly partial lacerations or stable closed injuries.
Immobilization with Early Protected Motion
- Indication: Lacerations involving <50% of tendon width in any zone.
- Rationale: Allows tendon healing while preserving joint motion when active extension is intact.
DIP Extension Splinting
- Indications: Acute Zone I injuries (mallet finger), nondisplaced bony mallet injuries, and chronic mallet fingers with a congruent joint.
- Protocol: Full-time splinting for 6 weeks or part-time for 4–6 weeks; maintain PIP motion to avoid stiffness (Lutz, 2015).
PIP Extension Splinting
- Indications: Closed central slip injuries (Zone III).
- Protocol: Full-time for 6 weeks or part-time for 4–6 weeks; ensure DIP flexion is maintained (Lutz, 2015).
MCP Extension Splinting
- Indications: Closed sagittal band ruptures (Zone V).
- Protocol: Full-time splinting for 4–6 weeks (Lutz, 2015).
Operative Management
Surgical repair is indicated for extensive tendon lacerations, unstable avulsion fractures, and chronic injuries that compromise function.
Tendon Repair
- Indication: Lacerations >50% of tendon width in any zone.
- Approach: Use existing wound or extend via longitudinal dorsal incision.
- Suture Technique
- Increased number of strands improves repair strength.
- Use locking stitches and thicker suture material (Yoon, 2019).
- Optional circumferential epitendinous suture for added strength.
Fixation of Bony Avulsion Injuries
- Indications: Bony mallet finger with volar subluxation of the distal phalanx.
- Techniques
- Closed reduction with percutaneous pinning
- Extension block pinning
- Open reduction and internal fixation (ORIF)
Tendon Reconstruction
- Indications: Chronic ruptures or irreparable injuries (Hanz, 2008).
- Options
- Tendon grafting or extensor turndown
- Lateral band mobilization
- Transverse retinacular ligament reconstruction
- FDS slip transfer
Staged Reconstruction (Hunter Technique)
- Stage 1: Silicone rod placement to maintain sheath integrity in scarred or deficient beds.
- Stage 2: Tendon graft insertion after 3–6 months (Colzani, 2016)
Immediate irrigation and debridement (I&D) is required for fight bite injuries to the MCP joint, with the wound closed loosely or in a delayed fashion and treated with culture-specific antibiotics, particularly targeting Eikenella corrodens, a common mouth flora pathogen.
Outcomes
With early repair and rehabilitation, extensor tendon injuries typically have a good prognosis (Colzani, 2016). Poor outcomes often correlate with delayed presentation, poor compliance, or joint stiffness at the time of treatment.
Extensor tendon injuries can lead to various complications (Lutz, 2015).
- Adhesion Formation: Causes loss of finger flexion, commonly seen in Zone IV and VII and in older patients. Early protected ROM and dynamic splinting (especially in Zone IV) may prevent this.
- Tendon Rupture: Caused by poor suture material or technique, aggressive therapy, or patient noncompliance.
- Swan Neck Deformity: Caused by prolonged DIP flexion, leading to dorsal subluxation of lateral bands and PIP hyperextension.
- Boutonnière Deformity: Caused by central slip disruption and volar subluxation of the lateral bands leading to DIP hyperextension.
Conclusion
1. Anatomy: Extensor tendons enable finger and wrist movement, divided into extrinsic (forearm origin) and intrinsic (hand-based) systems.
2. Extensor Mechanism: The extensor hood stabilizes the MCP joint; central slip and lateral bands insert into middle and distal phalanges. These injuries are caused by sharp trauma, hyperflexion, or attrition.
3. Assessment: Evaluate wound, tendon function, and neurovascular status; use Elson’s test for central slip injuries. X-ray rules out fractures, US confirms tendon integrity, and MRI helps in chronic or complex cases.
4. Mallet Finger: Zone I injury from forced DIP flexion; presents with DIP droop and is treated with extension splinting.
5. Management: Partial tendon injuries or closed injuries in Zones I, III, and V often managed with splinting. Operative management is indicated for complete lacerations, bony avulsions, or chronic tendon defects.
6. Complications: Include adhesions, tendon rupture, boutonnière or swan-neck deformity; early motion helps prevent stiffness.
Further Reading
- von Schroeder, Herbert P., and Michael J. Botte. "Anatomy of the extensor tendons of the fingers: variations and multiplicity." The Journal of hand surgery 20.1 (1995): 27-34.
- Hirai, Yoshimasa, et al. "An anatomic study of the extensor tendons of the human hand." The Journal of hand surgery 26.6 (2001): 1009-1015.
- Shrewsbury, Marvin M., and Richard K. Johnson. "A systematic study of the oblique retinacular ligament of the human finger: its structure and function." The Journal of Hand Surgery 2.3 (1977): 194-199.
- Kleinert, Harold E. "Report of the committee on tendon injuries." The Journal of Hand Surgery 14.2 (1989): 381-385.
- Hanz, Kevin R., et al. "Extensor tendon injuries: acute management and secondary reconstruction." Plastic and Reconstructive Surgery 121.3 (2008): 109e-120e.
- Matzon, Jonas L., and David J. Bozentka. "Extensor tendon injuries." The Journal of hand surgery 35.5 (2010): 854-861.
- Hart, Raymond G., Dennis T. Uehara, and Joseph E. Kutz. "Extensor tendon injuries of the hand." Emergency medicine clinics of north america 11.3 (1993): 637-649.
- Colzani, Giulia, et al. "Traumatic extensor tendon injuries to the hand: clinical anatomy, biomechanics, and surgical procedure review." Journal of hand and microsurgery 8.01 (2016): 002-012.
- Bendre, Anup A., Brian J. Hartigan, and David M. Kalainov. "Mallet finger." JAAOS-Journal of the American Academy of Orthopaedic Surgeons 13.5 (2005): 336-344.
- Griffin, M., Hindocha, S., Jordan, D., Saleh, M., & Khan, W. (2012). Management of extensor tendon injuries. The Open Orthopaedics Journal, 6, 36.
- Lutz, Kristina, Joey Pipicelli, and Ruby Grewal. "Management of complications of extensor tendon injuries." Hand Clinics 31.2 (2015): 301-310.
- Yoon, Alfred P., and Kevin C. Chung. "Management of acute extensor tendon injuries." Clinics in plastic surgery 46.3 (2019): 383-391.


