Summary Card
Definition
Dupuytren’s disease is a benign fibroproliferative disorder affecting the fascia of the palm and fingers.
Epidemiology
More common in older men of Northern European descent and is linked to family history, alcoholism, diabetes, epilepsy, & manual labour.
Pathoanatomy
Normal fascial anatomy becomes diseased with the formation of cords and nodules causing progressive contracture, usually on the ulnar hand. Cleland’s ligaments are not affected by the disease process.
Clinical Assessment
A progressive history and clinically palpable disease with a fixed flexion deformity. It is a clinical diagnosis.
Management
Treatment aims to release contractures using non-operative methods like Collagenase injections and needle aponeurotomy, or surgical release such as fasciotomy or fasciectomy.
Primary Contributor: Dr Kurt Lee Chircop, Educational Fellow.
Reviewer: Dr Waruguru Wanjau, Educational Fellow.
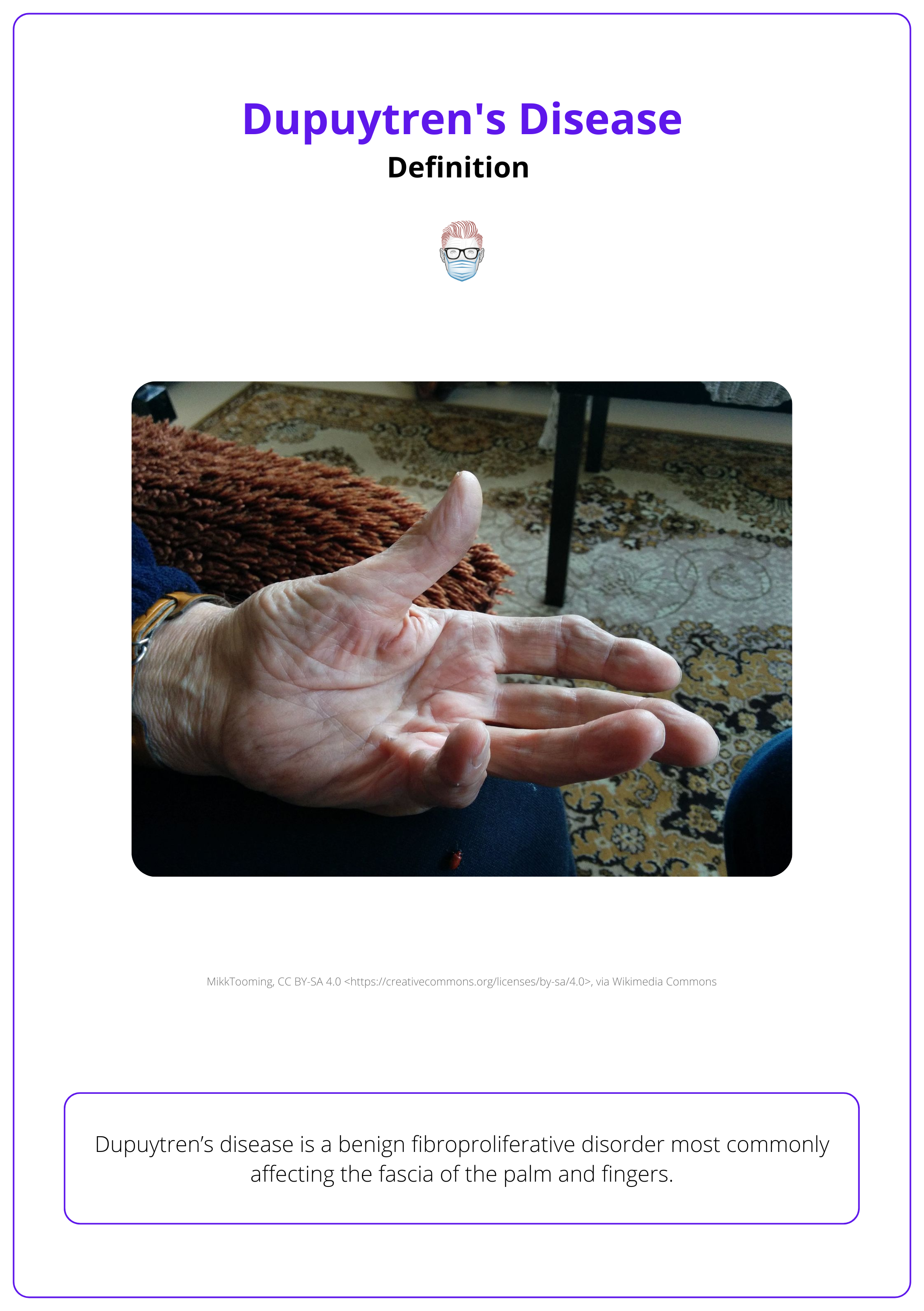
Definition of Dupuytren's Disease
Dupuytren’s disease is a benign fibroproliferative disorder most commonly affecting the fascia of the palm and fingers.
Dupuytren’s disease is a benign fibroproliferative disorder affecting the fascia of the palm and fingers. It begins with nodular formation, and progresses to longitudinal cord development.
The image below further illustrates Dupuytren’s disease.
Epidemiology of Dupuytren's Disease
Dupuytren’s disease is more common in older men of Northern European descent. It is linked to family history, alcoholism, diabetes, epilepsy, and manual labour.
Dupuyten’s disease can affect any ethnic group but it is more common in individuals of northern European descent. The disease is more prevalent in men, with incidence rising with age.
The disease is often linked with (Ruettermann, 2021):
- Family history: autosomal dominant with variable penetrance
- Medical Conditions: Alcohol Dependency, Diabetes, Epilepsy
- Manual labour or repeated trauma is controversial.
Anatomy of Dupuytren's Disease
The fascia develops pathological nodules and cords that progress to join contractures. Cleland’s ligaments are spared.
The palmar fascia is a complex structure. To understand Dupuytren's disease effectively, it is crucial to distinguish between the anatomy of normal palmar fascia and its pathological changes.
Normal Palmar Fascia Anatomy
Overview
The fascial anatomy of the palm is a complex structure. It originates at the wrist and extends towards the digits. It can be divided into four main anatomic components (Rayan, 1999)
- Palmar (central) aponeurosis
- Thenar (radial) aponeurosis
- Hypothenar (ulnar) aponeurosis
- Fingers: palmo-digital fascia & digital fascia
The image below shows the fascial anatomy of the palm.
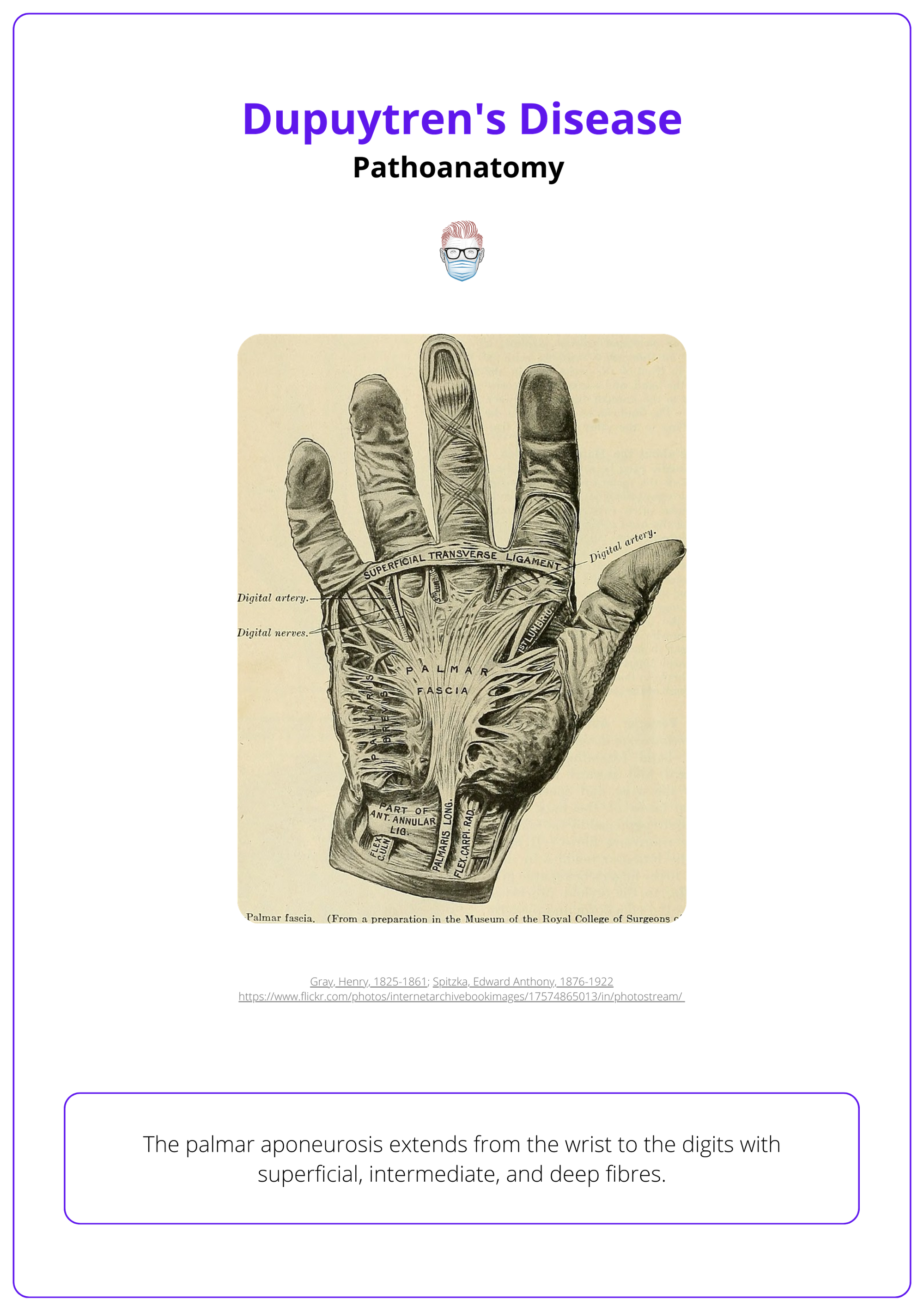
Palmar Aponeurosis
The palmar aponeurosis is a triangular facial layer with its apex overlying the palmaris longus. It gives rise to the pretendinous bands, which subsequently further divide at the metacarpal heads into 3 layers:
- Superficial: attaches to the skin at the palmar digital crease.
- Central: produces 2 spiral bands which merge with lateral digital sheath.
- Deep: insert on the interosseous muscle fascia and deep transverse metacarpal ligament.
Other structures
- Spiral bands travel distally and dorsally to form the web space coalescence. As they progress distally, they rotate 90° and pass from the coronal plane into the sagittal plane.
- The natatory ligament is a 3-dimensional support system spanning all 4 web spaces.
- Cleland’s and Grayson's ligaments surround the neurovascular bundle in a dorsal and volar manner, respectively. These ligaments are illustrated in the image below.
The PL tendon fibres blend with the PA and fan toward the thenar fascia, making the PL tendon prominent when pinching or cupping the hand with the wrist flexed.
Pathological Palmar Fascia Anatomy
Dupuytren’s disease is characterised by the development of nodules and cords within the palmar fascia. Initially, pathological nodules develop in the palm, and progressive cord formation then extends to the fingers.
It is described into 3 distinct phases:
- Proliferative: Nodule formation
- Involutional: Thickened nodules form cords
- Residual: Acellular scarring causes signification contractures
This usually affects the ulnar hand with the ring and little finger most commonly involved.
Cord formation results in varying degrees of contracture pathognomic with Dupuytren’s disease as summarised in the table below (Leibovic, 2018).
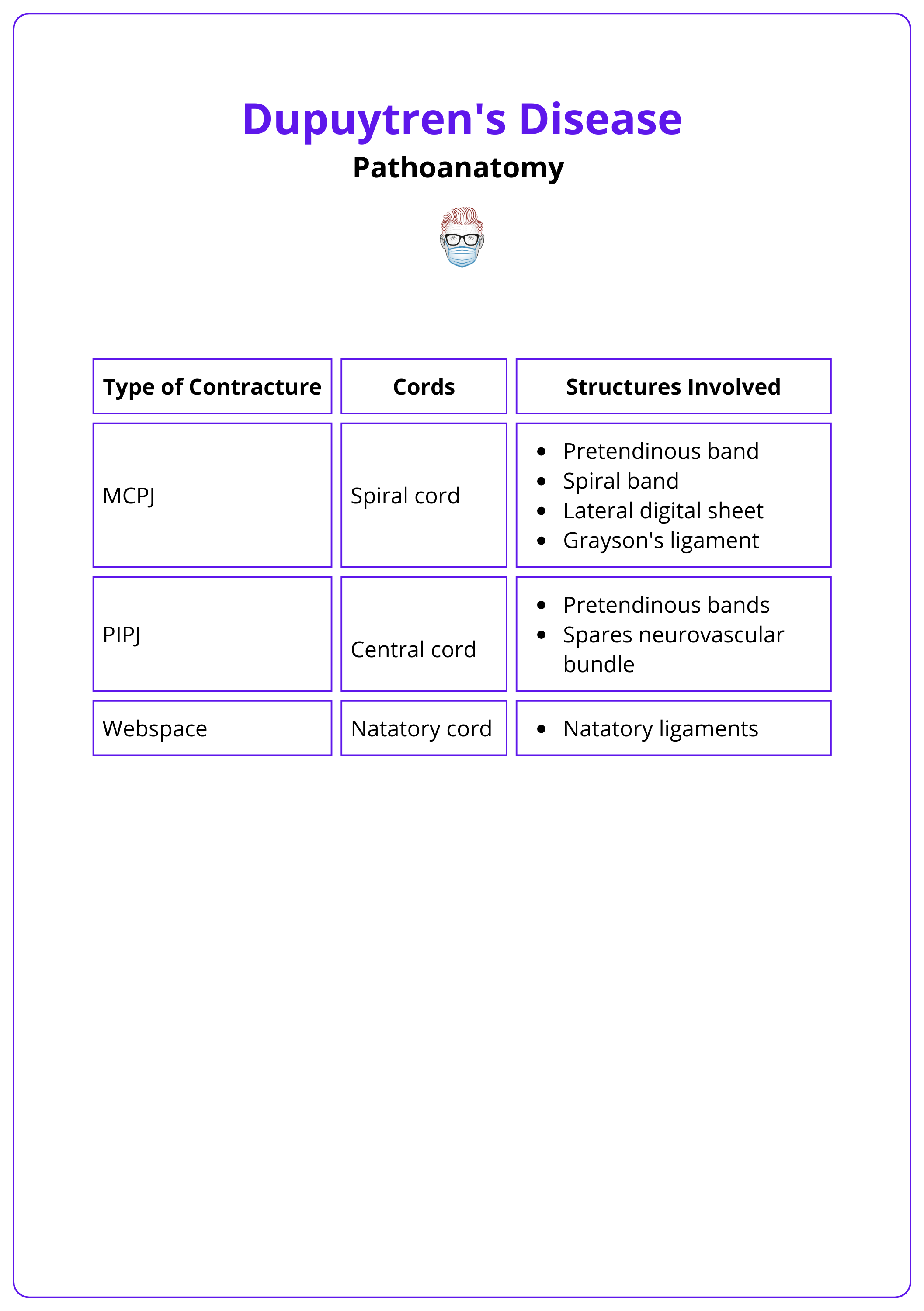
Cleland's ligament and the transverse ligament of the palmar aponeurosis are not involved in Dupuytren's disease (Leibovic, 2018).
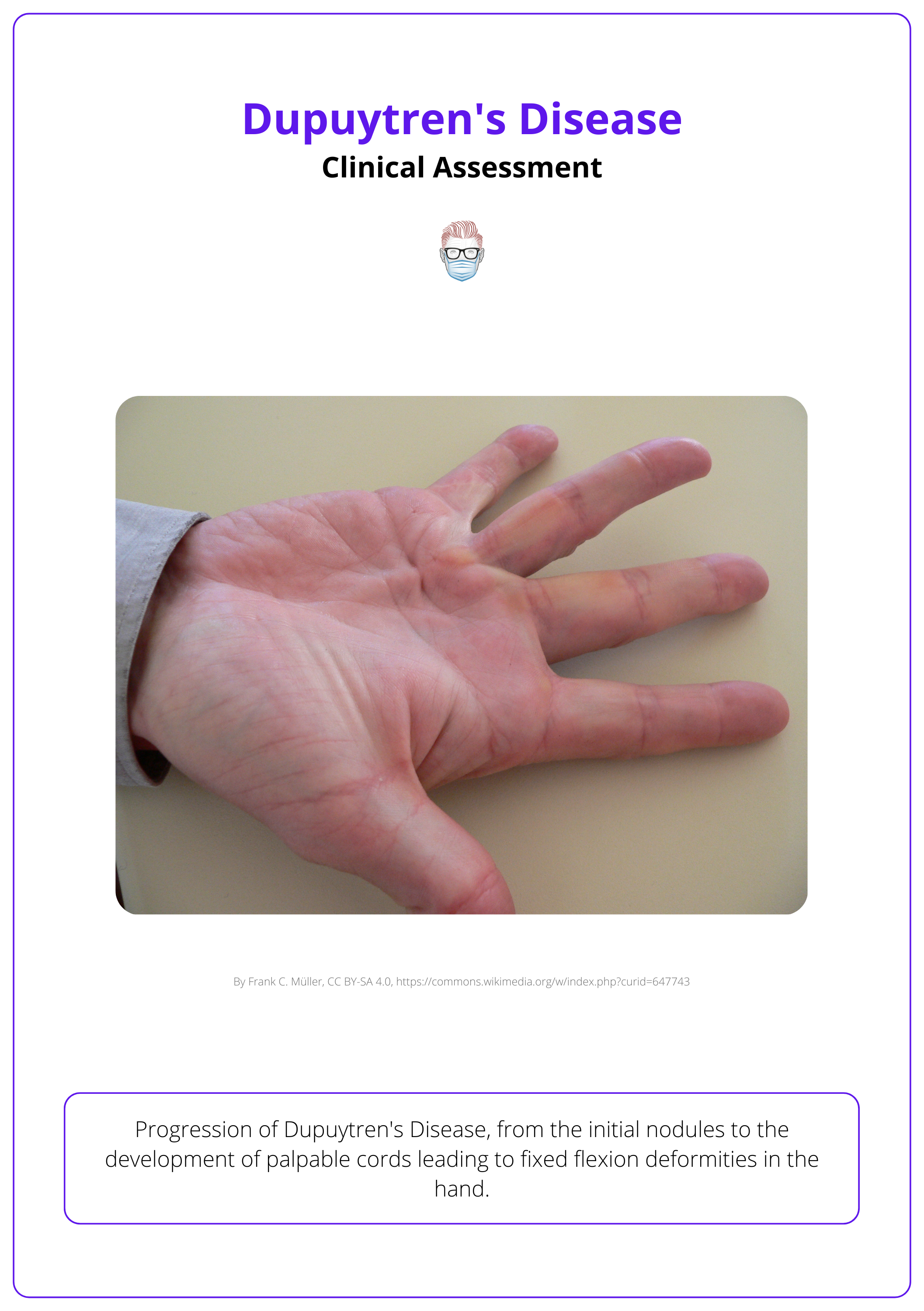
Clinical Assessment of Dupuytren's Disease
A history of progression from nodules to cord development, with clinically evident fixed flexion deformity is the cornerstone of the diagnosis.
The diagnosis is clinical and based on a detailed history and examination findings.
History
- Palpable nodules start in the palm along the distal palmar crease.
- Nodules progress into palpable cords.
- Cords thicken & shorten, causing fixed flexion contractures MCPJ & PIPJ.
- Pain rarely presents symptoms.
- Decreased range of motion interferes with daily activities.
The image below shows the presentation of Dupuytren's disease.
Physical Exam
In relation to the hand examination:
- Non-tender nodule in the pretendinous bands of the palmar fascia.
- Garrod pads (knuckle pads over PIPJ) may be tender.
- Presence of pits and grooves in the palm.
- Blanching of the skin with finger extension.
- Hueston's Tabletop Test.
Hueston's Tabletop Test is positive if the patient cannot lay their palm flat on a table with straightened fingers. (Fine, 2019).
In some patients, a total body examination may reveal (Karbowiak, 2021):
- Peyronie's disease: Dartos fascia of the penis
- Ledderhose disease: Plantar fascia
Differential Diagnosis
Dupuytren's disease is a relatively straightforward clinical diagnosis. However, it can occasionally be confused with,
- Trigger finger: usually associated with pain and no cords
- Volkmann’s ischemic contracture: history of trauma
- Ulnar claw hand: passively correctable
Management of Dupuytren's Disease
Treatment involves a multidisciplinary team of hand surgeons and therapists aiming to release contractures, reduce disease presence, and prevent progression.
Dupuytren's disease cannot be completely cured, and recurrence is common with any treatment. Goals should be individualized for each patient by an MDT. General considerations include:
- Resection of diseased tissue and release of contractures.
- Prevention of progression and reduction of recurrence risk.
- Maintenance of functional fingers and hand.
Indications for Treatment
Indications for treatment depend on disease progression, location, and patient factors. More specifically,
- History: rapid progression, occupational considerations.
- Contractures: PIPJ, or MCP joint > 30 degrees.
- Function: reduction function or hygiene.
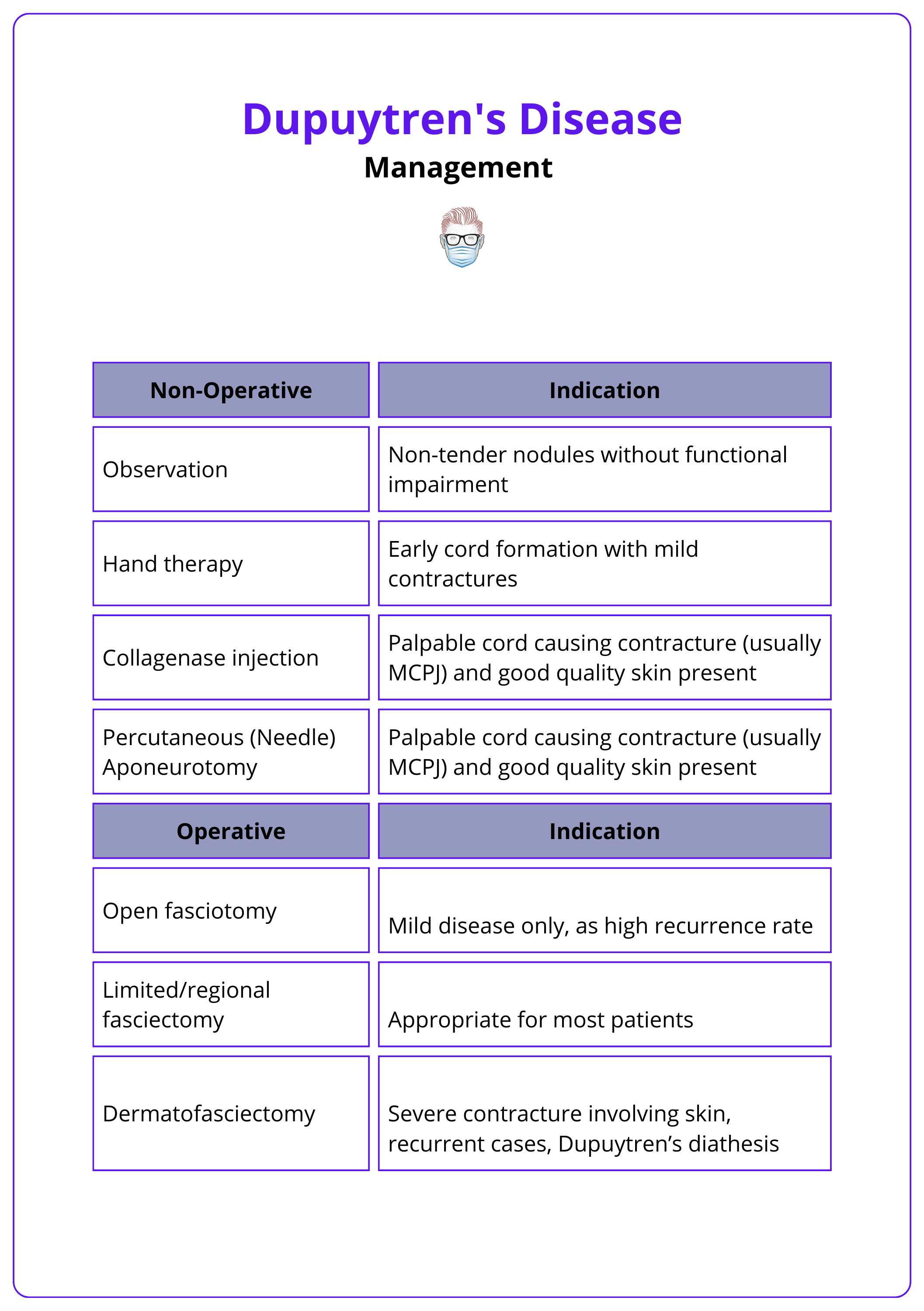
Treatment Options
Dupuytren's disease can be managed through non-operative or operative interventions (Desai, 2011), including:
- Non-operative: Conservative management and hand therapy
- Minimally invasive: Collagenase injections, needle aponeurotomy
- Surgery: Fasciectomy, dermofasciectomy
The specific indications for these treatment options are detailed below.
Fasciotomy divides the fascia to relieve tension, with less surgical morbidity but higher recurrence rates, suitable for minor contractures. Fasciectomy excises pathological fascia.
Surgical Technique
Different approaches have been described for treating Dupuytren's disease. Here is the general approach:
- Prepare: Assemble the hand set, hand table, lead hand, and loupes.
- Design: Use Brunner incisions or the Skoog approach, followed by Z-plasties.
- Dissect: Raise adequate flaps before excising all diseased fascia, preserving the neurovascular bundle.
- Close: Close without tension using interrupted sutures and splint the hand with fingers in extension. Z-plasties may be needed.
- Post-Op: Initiate early rehabilitation according to local protocols.
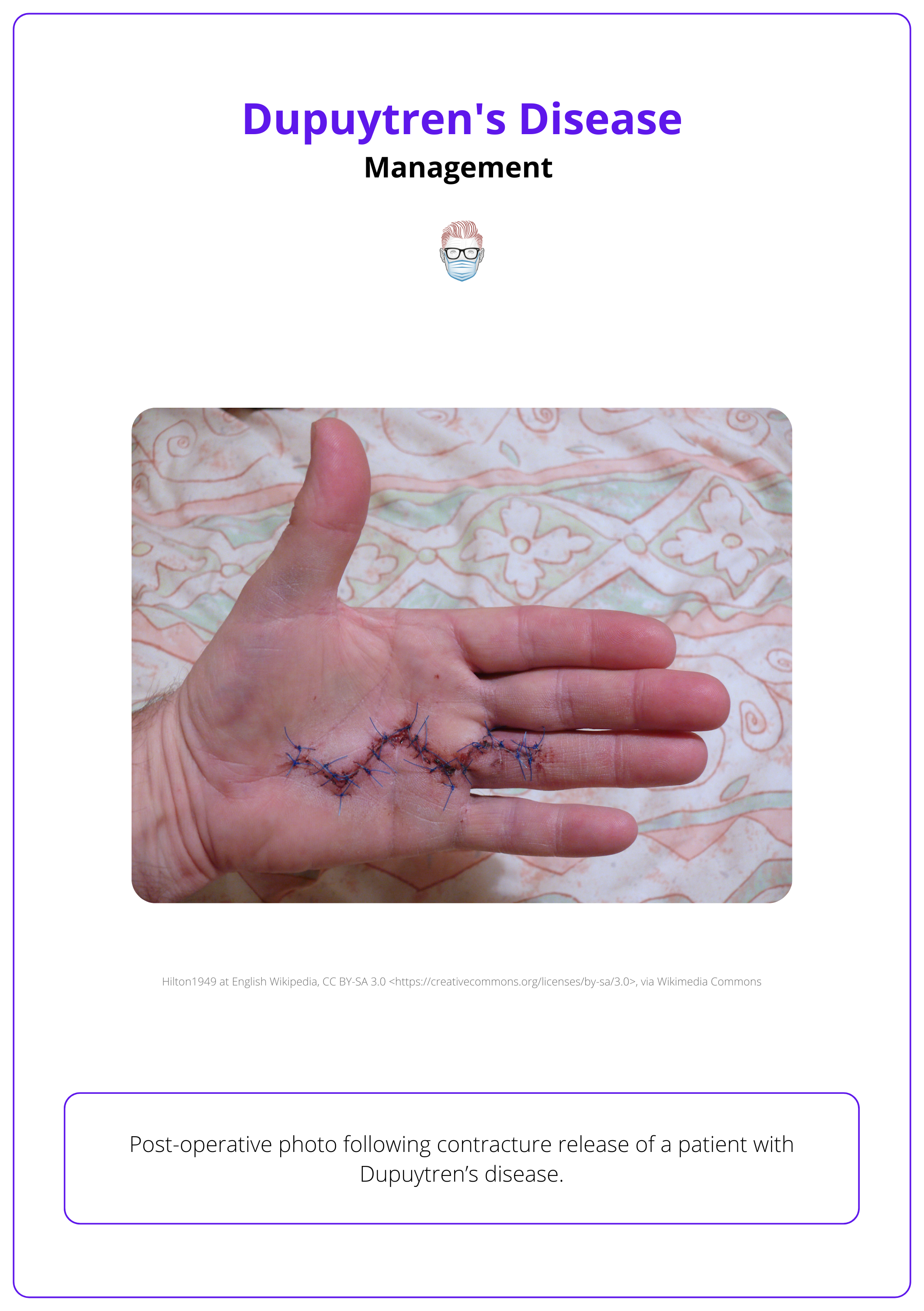
The image below illustrates the post-operative view of Dupuytren's disease resected via Brunner incisions.
Complications
Treatment for Dupuytren's disease can lead to several complications, including:
- Neurovascular injury
- Hematoma
- Dupuytren’s flare response
- Skin flap necrosis
- Recurrence, with rates after surgery being highly variable (Eberlin, 2018).
Finger ischemia from vessel spasm and shortening may occur on full extension. Flexion often restores circulation. Splint the finger slightly flexed, gradually increasing extension in future visits (Black, 2011).
Conclusion
1. Understanding Dupuytren’s Disease: Dupuytren's disease is a benign fibroproliferative disorder primarily affecting the fascia of the palm and fingers, leading to progressive hand deformity.
2. Epidemiology: Dupuytren’s disease predominantly affects older men of Northern European descent and is associated with factors such as family history, alcoholism, diabetes, and manual labor.
3. Pathoanatomy: You understand the transformation of normal fascial anatomy into diseased cords and nodules, leading to contractures, specifically affecting the ulnar side of the hand.
4. Clinical Assessment: You can identify Dupuytren's disease through its clinical presentation, which includes nodules and cords leading to fixed flexion deformities.
5. Management Strategies: You're informed about the various treatment options ranging from non-operative methods such as collagenase injections and needle aponeurotomy to surgical interventions like fasciotomy and fasciectomy.
6. Potential Complications: You are prepared to manage and anticipate potential complications arising from the treatment of Dupuytren’s disease, such as neurovascular injury, hematoma, or recurrence of the disease.
Further Reading
- Ruettermann M, Hermann RM, Khatib-Chahidi K, Werker PMN. Dupuytren's Disease-Etiology and Treatment. Dtsch Arztebl Int. 2021 Nov 19;118(46):781-788. doi: 10.3238/arztebl.m2021.0325.PMID: 34702442; PMCID: PMC8864671.
- Karbowiak, Marta, et al. "Dupuytren’s disease." bmj 373 (2021).
- Leibovic, Stephen J. "Normal and Pathologic Anatomy of Dupuytren Disease." Hand Clinics 34.3 (2018): 315-329.
- Eberlin, Kyle R., and Chaitanya S. Mudgal. "Complications of treatment for Dupuytren disease." Hand Clinics 34.3 (2018): 387-394.
- Hindocha, Sandip. "Risk factors, disease associations, and Dupuytren diathesis." Hand Clinics 34.3 (2018): 307-314.
- Fine, Nicola F., and Nadia Sciberras. "Examination of the hand for MRCS." Surgery (Oxford) 37.5 (2019): 265-269.
- Desai, Shaunak S., and Vincent R. Hentz. "The treatment of Dupuytren disease." The Journal of hand surgery 36.5 (2011): 936-942.
- Rodrigues, J. N., et al. "Functional outcome and complications following surgery for Dupuytren’s disease: a multi-centre cross-sectional study." Journal of Hand Surgery (European Volume) 42.1 (2017): 7-17
- Black, Eric M., and Philip E. Blazar. "Dupuytren disease: an evolving understanding of an age-old disease." JAAOS-Journal of the American Academy of Orthopaedic Surgeons 19.12 (2011): 746-757.


