Summary Card
Definition of a Congenital Melanocytic Naevus
A brown or black lesion is present at birth, which can be considered "giant" if >20cm.
Features of Congenital Melanocytic Naevus
A congenital lesion with pigmentation changes, risk of malignant transformation, and extracutaneous complications.
Management of Congenital Melanocytic Naevus
A multi-disciplinary team for active surveillance or surgical resection if indicated.
Definition of a Congenital Melanocytic Naevus
A congenital melanocytic lesion is a black or brown lesion present at birth. A “giant” congenital melanocytic nevus is >20 cm in adults or predicted to reach that size by adulthood (Bittencourt et al., 2000).
The image below illustrates the signs of Congenital Melanocytic Naevus.

Features of Congenital Melanocytic Naevus
A congenital melanocytic naevus is a pigmented lesion present at birth that has a risk of malignant transformation and extracutaneous deposition.
A congenital melanocytic naevus presents as a brown or black lesion at birth. It is most commonly found on the trunk and changes appearance over time with multiple satellite lesions.
Natural History
The natural history of giant congenital melanocytic nevi is one of expansion in proportion to the body’s growth.
- At birth: hairless, pale brown, flat lesion.
- Colour: hyperpigmentation and colour variegation, the surface pigment may fade.
- Texture: hypertrichosis, verrucous, nodularity (neurotisation of the lesion).
- Malignant Transformation: focal growths, ulceration, pruritus, pain, or bleeding.
The image below illustrates the natural growth of a congenital melanocytic naevus.

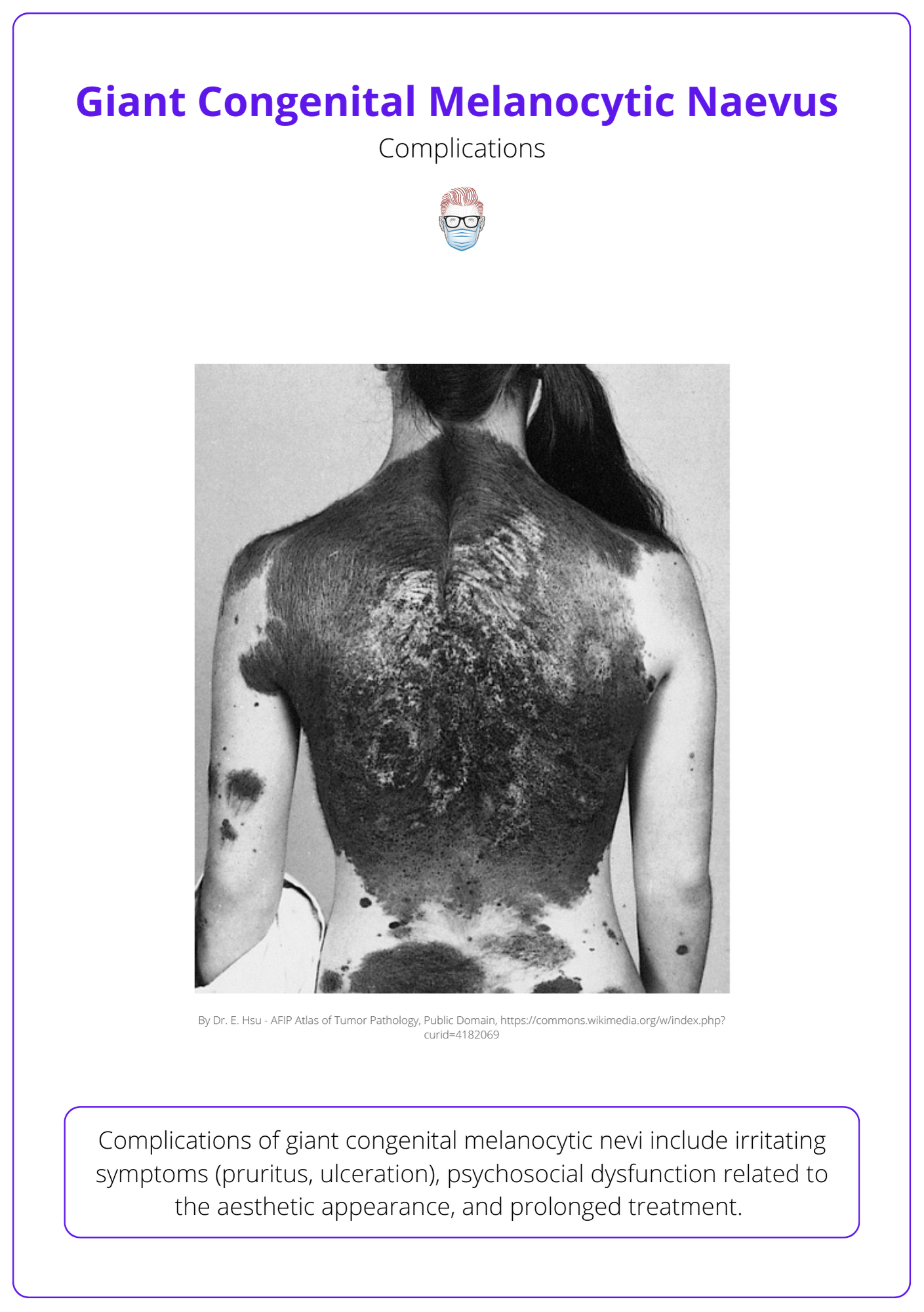
Complications
Complications of giant congenital melanocytic nevi include irritating symptoms (pruritus, ulceration), psychosocial dysfunction related to the aesthetic appearance, and prolonged treatment.
Less common complications include:
- Melanoma: malignant transformation is discussed more below.
- Extracutaneous deposits: mucosal, retroperitoneal, and leptomeningeal.
- Neurocutaneous melanosis: benign or malignant CNS proliferation in patients with giant CMN, multiple satellite lesions, and location of trunk or calvarium.
- MSK associations: scoliosis, spinal dysraphism, limb abnormalities.
Melanoma Transformation
Malignant transformation in patients with giant congenital melanocytic nevi can result in cutaneous or noncutaneous melanoma.
The reported risk of melanoma in patients with giant congenital melanocytic nevi ranges from 3-9% (Watt et al., 2004) with a lifetime risk of approximately 6% (~ 17-fold increased risk of melanoma compared with the general population) (Rhodes et al., 1981).
In relation to the rate of malignant transformation (Trozak et al., 1975 & Kaplan, 1974):
- 50% by age 3
- 60% by childhood
- 70% by puberty
For this reason, surgical excision of high-risk cutaneous lesions is best performed in early childhood rather than delaying treatment until a later age.
Management of Congenital Melanocytic Naevus
A congenital melanocytic naevus is managed through a multi-disciplinary team. The majority of lesions are treated through active surveillance or surgical resection if indicated.
A multidisciplinary approach involving paediatricians, dermatologists, psychologists, plastic surgeons, neurologists, neurosurgeons, and radiologists.
Active Surveillance
- Regular examination with photography by a dermatologist and plastic surgeons.
- Patient education on the natural history and potential for pigment fading.
The image below illustrates the complications of giant congenital melanocytic naevus.
Surgical Excision
Indications for surgical excision of congenital melanocytic nevi include (Gosain et al. 2001 & Bauer et al., 2005):
- Melanoma transformation
- Symptom control
- Maintain function
- Aesthetic improvement
Surgical options include:
- Direct Excision: the most accepted treatment option.
- Serial excision: ideally, if amenable to an excision in three stages or less.
- Reconstruction: skin graft, expansion, skin substitutes, free tissue transfer.
After surgical treatment, regular follow-up for recurrence and monitoring of satellite lesions.
Timing of Surgery
Early surgery has not been shown to be advantageous and carries increased anaesthetic risk. Surgery can be considered in patients after 1 year when anaesthetic risks are lower.
Traditionally, it was thought that early surgery for CMNs was preferable. This was based on the theory that pigment deepens after birth (‘Abtropfung’) (Unna, 1893). This has now been refuted, and the current theory is that the depth of the naevus correlates best with its size (Worret et al., 1893 & Barnhill et al., 1995 & Cass et al., 1997).
Non-Surgical Options
Many nonsurgical options for the treatment of giant congenital melanocytic nevi have been described, including dermabrasion, laser ablation, curettage, and chemical peel.
Limitations with these treatments include:
- Decrease the burden of nevus cells but do not result in complete cell removal.
- No histologic diagnosis.
- Difficult postoperative monitoring.
Conclusion
1. Basics of Congenital Melanocytic Naevus: Gained a comprehensive understanding of what a congenital melanocytic naevus is, including the differentiation between common and giant types based on size criteria.
2. Features and Complications: Learned about the distinct features of congenital melanocytic naevi, such as pigmentation changes, and the risk factors associated with malignant transformation and extracutaneous manifestations.
3. Management Strategies: Explored the various management strategies for congenital melanocytic naevi, including the roles of active surveillance and surgical resection.
4. Treatment Options: Familiarized yourself with the specific treatment options available for congenital melanocytic naevi, from non-surgical approaches like dermabrasion and laser therapy to surgical interventions such as excision and reconstructive techniques.
5. Preventive and Monitoring Measures: Understood regular monitoring and patient education in managing congenital melanocytic naevi to monitor for signs of malignant transformation and to manage cosmetic concerns.
6. Potential for Malignant Transformation: Developed an awareness of the potential for malignant transformation within these naevi and the implications this has for long-term patient management and surveillance protocols.
References
- Bittencourt, F. V., Marghoob, A. A., Kopf, A. W., et al. Large congenital melanocytic nevi and the risk for development of malignant melanoma and neurocutaneous melanocytosis. Pediatrics 106: 736, 2000.
- Watt, A. J., Kotsis, S. V., and Chung, K. C. Risk of melanoma arising in large congenital melanocytic nevi: A systematic review. Plast. Reconstr. Surg. 113: 1968, 2004.
- Rhodes, A.R., Wood, W.C., Sober, A.J.et al. Nonepidermal origin of malignant melanoma associated with a giant congenital nevocellular nevus. Plast. Reconstr. Surg. 67: 782, 1981.
- Trozak, D. J., Rowland, W. R., and Hu, F. Metastatic malignant melanoma in prepubertal children. Pediatrics 55: 191, 1975.
- Kaplan, E. N. The risk of malignancy in large congenital nevi. Plast. Reconstr. Surg. 53: 421, 1974.
- Gosain, A. K., Santoro, T. D., Larson, D. L., et al. Giant congenital nevi: A 20-year experience and an algorithm fortheir management. Plast. Reconstr. Surg. 108: 622, 2001.
- Bauer, B. S., and Corcoran, J. Treatment of large and giant nevi. Clin. Plast. Surg. 32: 11, 2005.
- Unna PG. Naevi und Naevocarcinome. Berl Klin Wochenschr 1893;30:14e6.
- Worret WI, Burgdorf WH. Which direction do nevus cells move?Abtropfung reexamined. Am J Dermatopathol 1998;20:135e9
- Barnhill RL, Fleischli M. Histological features of congenital melanocytic nevi in infants one year of age or younger. J Am AcadDermatol 1981;33:780e5.
- Cass DL, Bullard KM, Sylvester KG, et al. Wound size and gestational age modulate scar formation in fetal wound repair. J Pediatr Surg 1997;32:411e5.
- Kinsler, V., & Bulstrode, N. (2009). The role of surgery in the management of congenital melanocytic naevi in children: a perspective from Great Ormond Street Hospital. Journal of Plastic, Reconstructive & Aesthetic Surgery, 62(5), 595–601.doi:10.1016/j.bjps.2008.12.016 10.1016/j.bjps.2008.12.016


