Summary Card
Definition
A dermoid cyst is a benign congenital anomaly from ectodermal entrapment along embryonic closure lines, mainly in the head and neck region.
Pathology
Dermoid cysts arise from ectodermal entrapment during embryonic development. They are lined by keratinizing squamous epithelium and often contain sebaceous glands and hair.
Orbital Dermoid Cysts
More than 80% of congenital dermoid cysts occur in the upper outer quadrant of the orbital rim. These cysts typically present as painless, non-pulsatile, firm upper eyelid swellings fixed to the underlying bone.
Nasal Dermoid Cysts
Nasal dermoids, uncommon and comprising 4-12% of head and neck dermoid cysts, are the most frequent congenital midline nasal lesions, presenting as painless, noncompressible midline masses.
Complications
Dermoid cysts with intracranial or intraspinal extensions can lead to meningitis, cerebral abscesses, local mass effects, and additional complications.
Primary Contributor: Dr Kurt Lee Chircop, Educational Fellow.
Reviewer: Dr Waruguru Wanjau, Educational Fellow.
Definition of a Congenital Dermoid Cyst
A dermoid cyst is a benign, congenital skin anomaly from trapped ectodermal elements, often diagnosed in childhood and mainly found in the head and neck region.
A dermoid cyst is a benign skin anomaly arising from trapped ectodermal and mesodermal elements along embryonic lines. Typically congenital, these cysts are not always identified at birth:
- ~40% of dermoid cysts are identified at birth
- ~60% are diagnosed by the age of five.
- ~84% occurring in the head and neck region (Shareef, 2023).
A congenital dermoid cyst is illustrated in the image below.
Pathology of Congenital Dermoid Cysts
Dermoid cysts stem from abnormal fetal development and are commonly found in the supraorbital area, cranial sutures, and nose. It is composed of ectodermal and mesodermal elements.
Dermoid cysts are benign tumors formed from ectodermal and mesodermal cells trapped during the neural tube closure in the 5th and 6th weeks of embryonic development. (Cavazza, 2011).
The typical structure of a dermoid cyst is:
- Shape: Round or ovoid
- Lining: skin-like epithelium, dermal layer with sebaceous glands & appendages.
- Contents: hair, nails ± dental or bone-like structures (depends on location)
The most common location of a dermoid cyst is the periorbital lateral eyebrow (external angular dermoid). Other common locations include:
- Supraorbital area: Above the eye socket.
- Cranial sutures: Along the skull bone joints.
- Nose: Especially near the nasal root.
Less common locations include midline neck, Forehead, scalp, behind the ear (posterior auricular or mastoid)
Orbital Dermoid Cysts
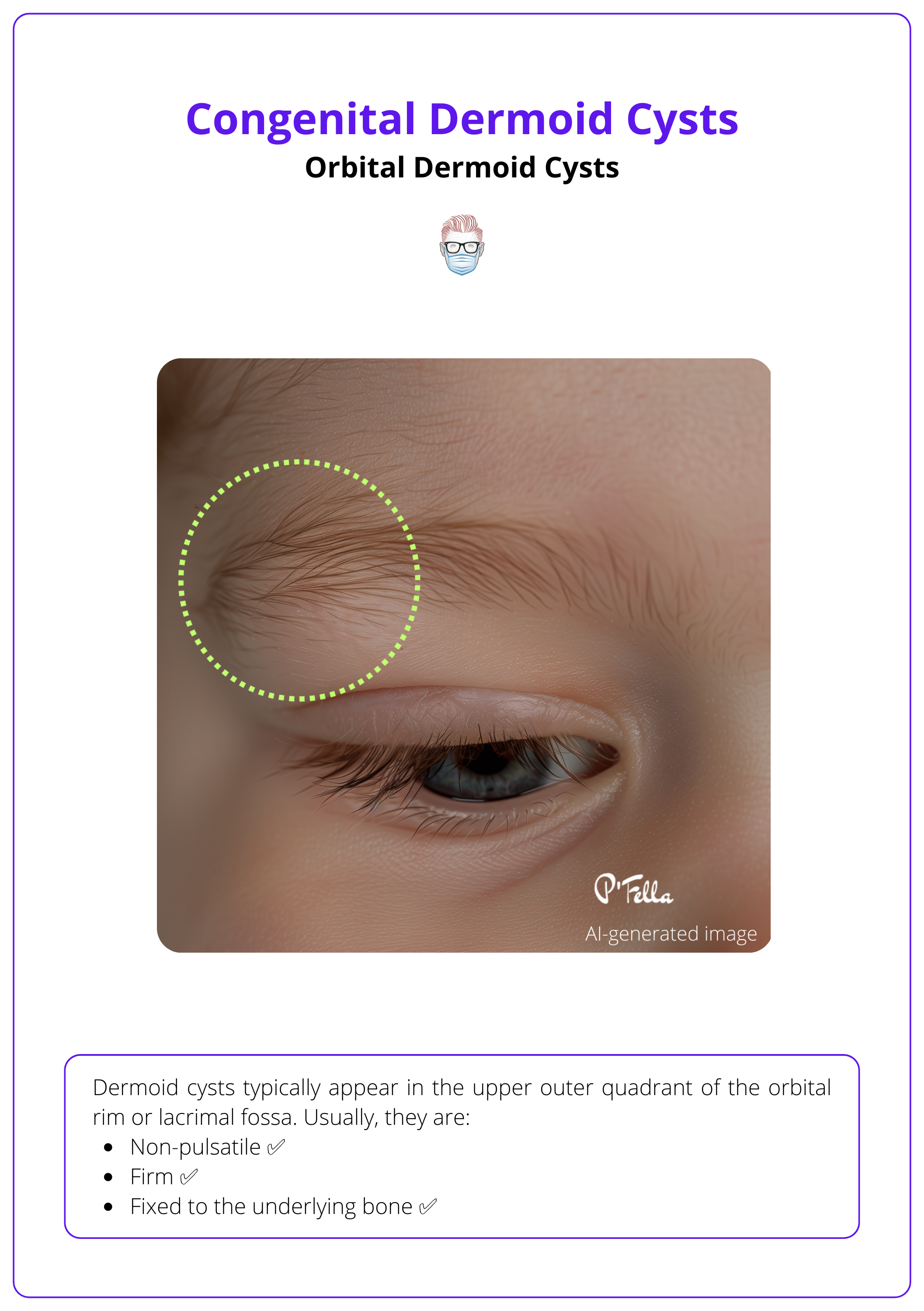
Dermoid cysts typically appear in the upper outer quadrant of the orbital rim or lacrimal fossa. They are usually painless, firm, and fixed to the bone, without pulsation.
Orbital Dermoid Cysts, the most common congenital type, typically occur in the upper outer quadrant of the orbital rim or lacrimal fossa - near the zygomaticofrontal suture (Eldesouky, 2016).
They can classified radiologically or anatomically:
- Radiology: superficial or deep based on their position relative to the interzygomatic line on CT or MRI (Eldesouky, 2016)
- Anatomically: juxtasutural, sutural, or soft tissue variants depending on their relation to the underlying bone (Shields, 2004).
Orbital Dermoid Cysts account for 3-9% of all periorbital tumours in the paediatric population (Dutton, 2011).
Clinical Features
Orbital dermoid cysts typically present as painless upper eyelid swellings without overlying cutaneous features. On palpation, these lesions are:
- Non-pulsatile
- Firm
- Fixed to the underlying bone
These characteristics of an orbital dermoid cyst are illustrated below.
An orbital dermoid cyst may leak into surrounding tissues, causing inflammation that mimics primary inflammation and leads to diagnostic uncertainty.
Diagnosis
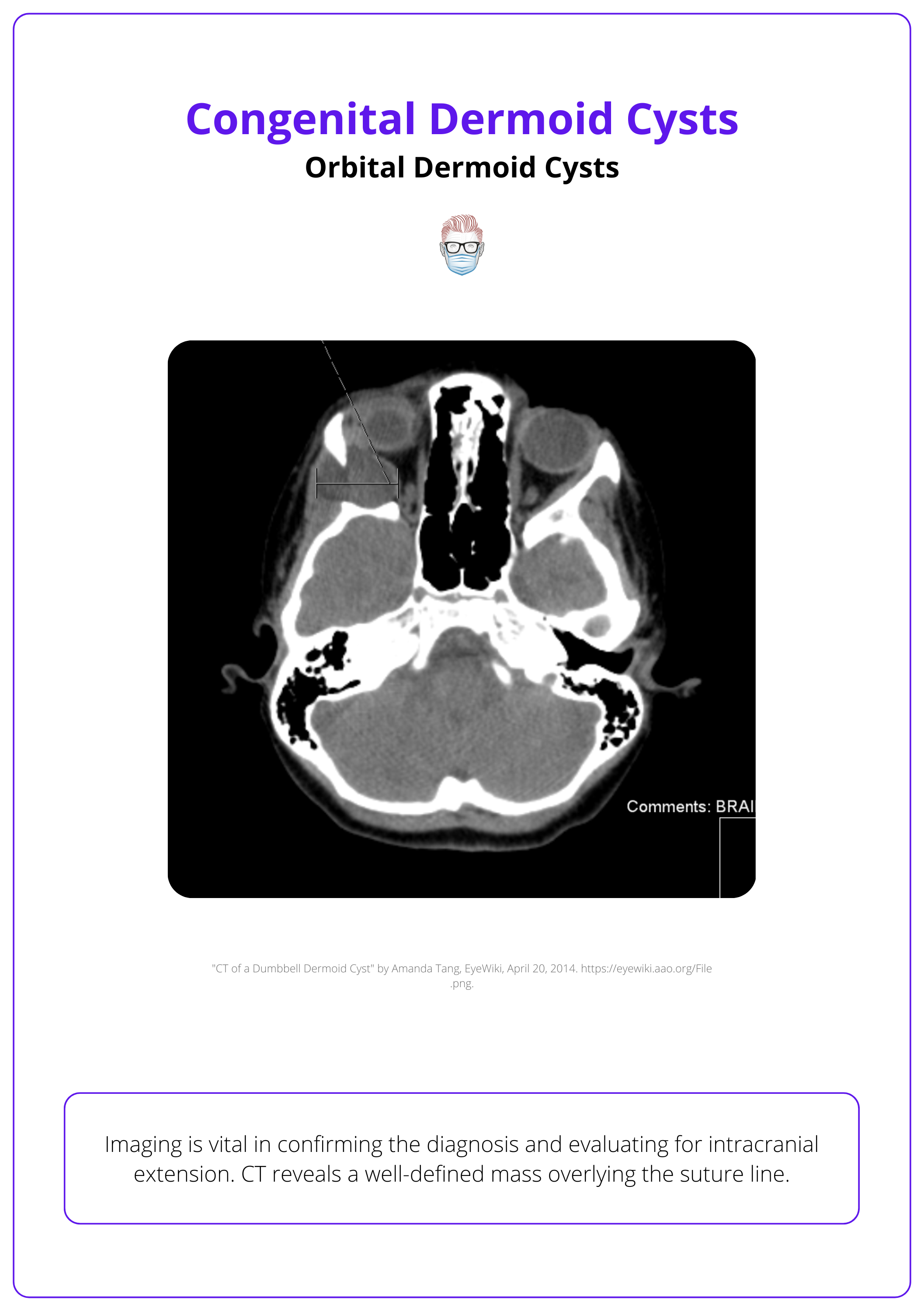
Imaging is vital in confirming the diagnosis and evaluating for intracranial extension:
- CT: Reveals a well-defined mass with an enhancing wall and non-enhancing lumen, luminal debris, and a bony fossa overlying the suture line.
- MRI: Shows a well-defined ovoid structure, hypointense on T1 and hyperintense on T2 relative to surrounding orbital fat, with no enhancement due to the lack of blood vessels within the cyst.
The image below illustrates the CT presentation of an orbital dermoid cyst.
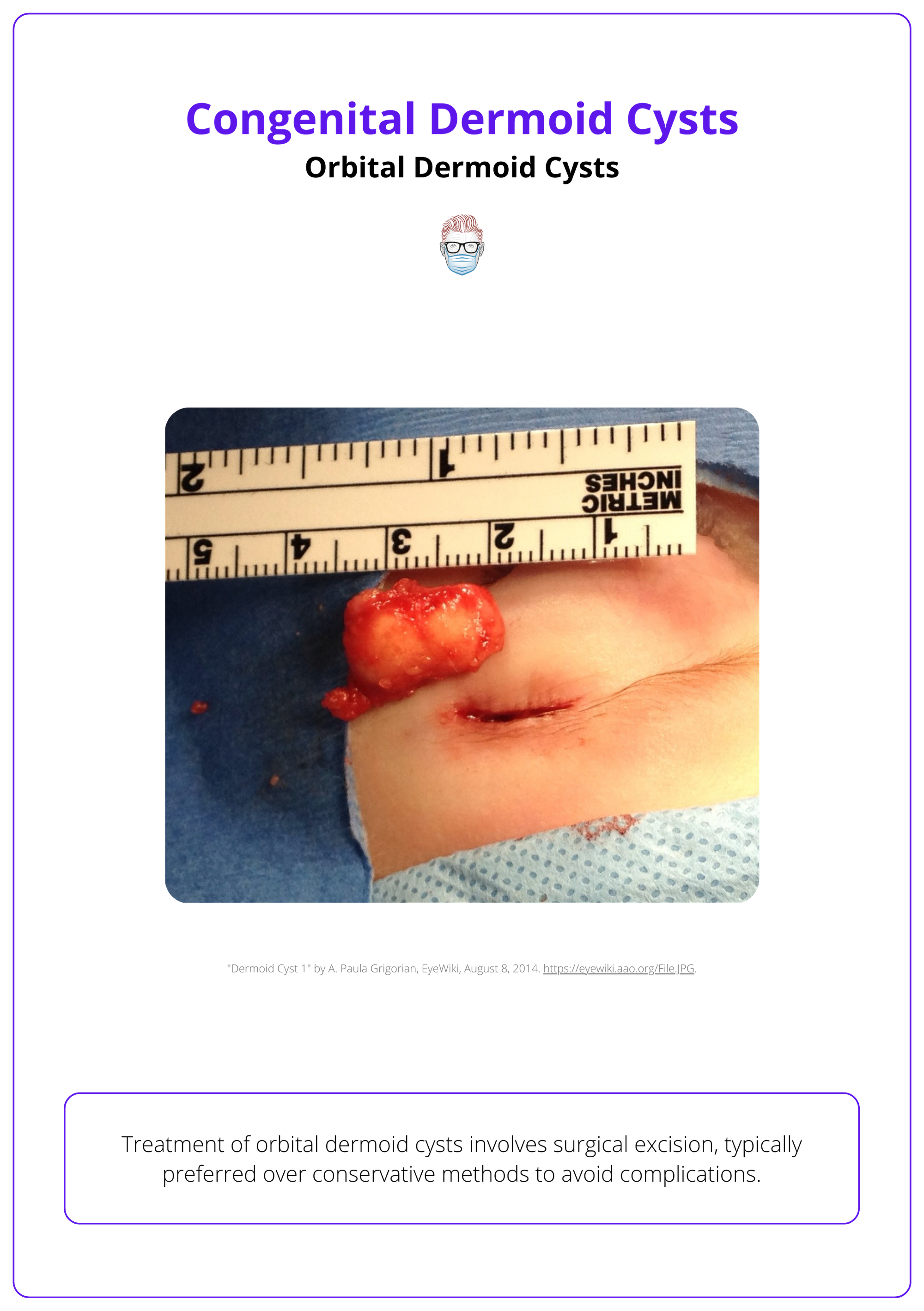
Treatment
Treatment involves surgical excision, typically preferred over conservative methods to avoid complications. Key steps in the supratarsal approach include:
- Incision: Made at the upper eyelid crease for optimal access.
- Dissection: The orbicularis oculi muscle is dissected to locate the cyst in the subperiosteal plane.
- Excision: Complete removal of the cyst without rupturing its wall is crucial.
If the cyst wall ruptures, thorough irrigation is required to remove all remnants and prevent recurrence, as incomplete removal can necessitate more complex repeat surgeries.
The image below illustrates the surgical treatment of an orbital dermoid cyst.
An orbital dermoid cyst may form a dumbbell shape across the zygomaticofrontal suture, causing pulsating proptosis during mastication, a distinct sign of this condition (Kerdoud, 2021).
Nasal Dermoid Cysts
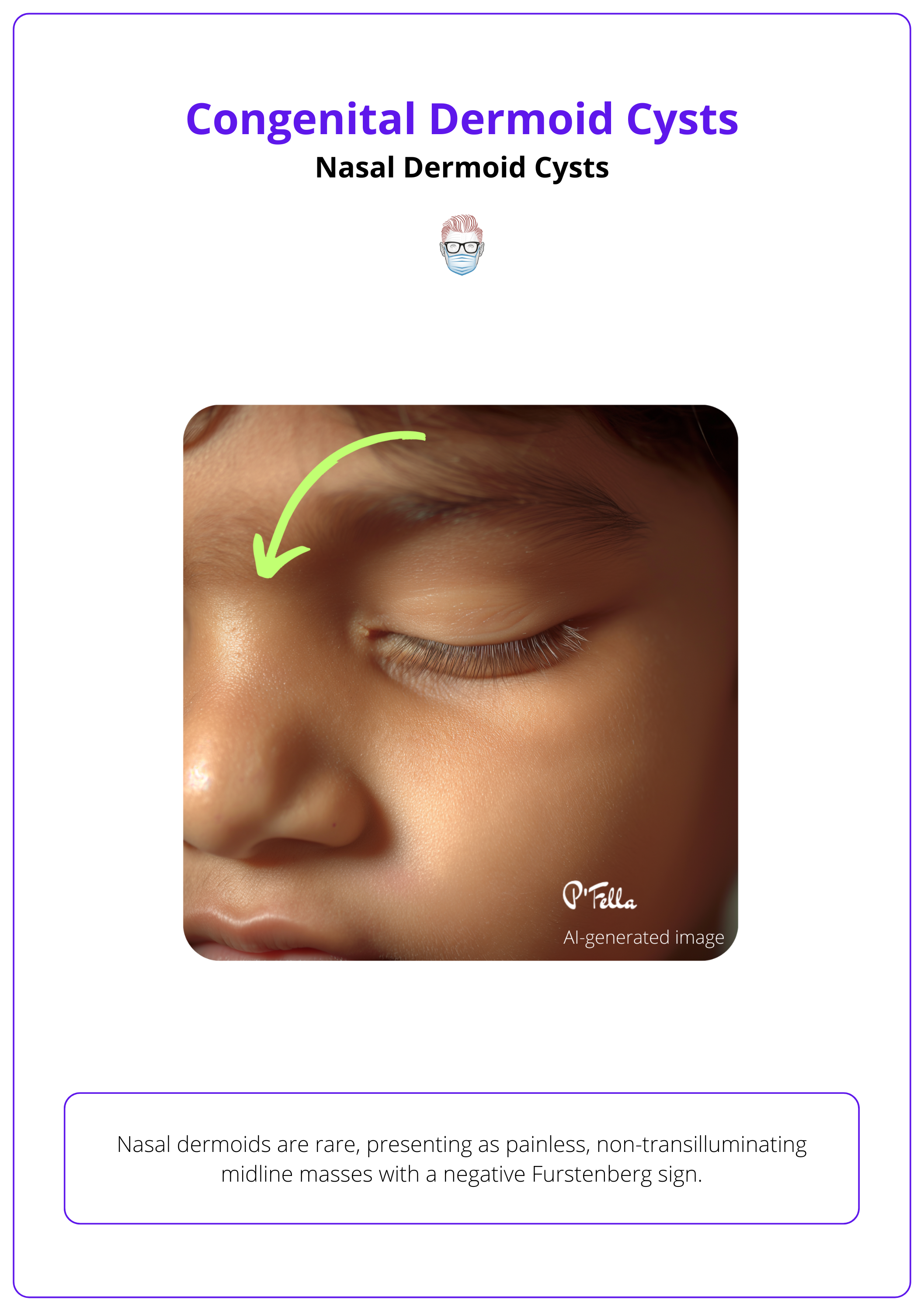
Nasal dermoids are rare, presenting as painless, non-transilluminating midline masses with a negative Furstenberg sign. They require imaging and complete surgical removal for management.
Nasal dermoids, which make up 4-12% of dermoid cysts in the head and neck region, are less common than their orbital counterparts and typically manifest as the predominant congenital midline nasal lesions with a slight male bias (Van Wyhe, 2016).
These cysts develop from the incomplete regression of the neuroectodermal tract during the eighth week of embryogenesis, potentially extending intracranially through the foramen cecum (Zapata, 2006).
Clinical Features
Nasal dermoids typically appear as painless midline masses located anywhere from the base of the columella to the nasoglabellar region. Hair protruding from a nasal punctum is pathognomonic for nasal dermoids.
Other typical features include:
- Noncompressible
- Does not transilluminate
- Negative Furstenberg sign
- ± sinus with intermittent discharge
The image below illustrates the presentation of a nasal dermoid cyst.
The Furstenberg sign tests if head masses swell with increased intracranial pressure. Positive results indicate brain connections (e.g., encephaloceles); negative results occur in conditions like nasal dermoids. (Van Wyhe, 2016)
Investigations
Imaging is vital for diagnosing nasal dermoids, with MRI and CT scans as the gold standard, particularly important given that up to 45% of these cases may have intracranial extensions. Key Indicators of Intracranial Extension:
- Enlarged foramen cecum
- Bifid crista galli
These imaging findings help rule out other potential diagnoses:
- Brain-related conditions: Encephaloceles, Gliomas
- Soft tissue conditions: Epidermal inclusion cysts, Lipomas, Hemangiomas, Teratomas, Neurofibromas, Lymphangiomas
Management
Effective management of nasal dermoids requires a multidisciplinary team (MDT) including plastic surgeons and neurosurgeons. The primary goal is the complete surgical excision of the cysts and any associated sinus tracts to prevent recurrence, which can occur in 50-100% of cases if any dermal components are left behind (Bloom, 2002).
Surgical Approaches:
- Midline Vertical Incision: Provides adequate exposure for excising both intracranial and extracranial components in a single stage.
- Open Rhinoplasty Approach: Allows thorough access to the skull base for complete removal.
- Bicoronal Craniotomy: Necessary for cases with extensive intracranial extension.
Complete excision is essential for a cure, with the chosen surgical approach tailored to the extent of the cyst and its intracranial involvement (Miller, 2019)
Epidermal inclusion cysts lack skin adnexal structures and contain a friable keratin core. In contrast, nasal dermoids are well-defined cysts lined with keratinizing squamous epithelium and mesodermal adnexal structures.
Complications of Congenital Dermoid Cysts
Dermoid cysts without intracranial or intraspinal extension do not usually cause complications.
Dermoid cysts without intracranial or intraspinal extension typically do not cause complications. However, those with such extensions can lead to:
- Meningitis
- Cerebral abscesses
- Local mass effects
Additional complications of orbital dermoid cysts include bony erosions, eyelid displacement, and proptosis. Nasal dermoid cysts may present with persistent discharge or infection, including osteomyelitis (Blake, 2006).
Rupture of dermoid cysts can result in localized inflammation and infection, making complete surgical removal more challenging. Malignant transformation to squamous cell carcinoma (SCC) is a rare but possible complication in long-standing dermoid cysts (Shareef, 2023).
Conclusion
1. Understanding Dermoid Cysts: Acquired a comprehensive understanding of dermoid cysts, including their congenital origin, common locations, and how they develop from ectodermal entrapment.
2. Identifying Symptoms: Recognized the typical presentation of dermoid cysts in various anatomical locations, which can help in early detection.
3. Diagnostic Processes: Learned about the essential imaging techniques used for diagnosing dermoid cysts and distinguishing these from other similar lesions.
4. Treatment Options: Reviewed the primary treatment approach —surgical excision — and understood the importance of complete resection to prevent recurrence and manage potential complications.
5. Complications: Aware of the potential complications associated with dermoid cysts, especially those with intracranial or intraspinal extensions.
Further Reading
- Shareef, Shahjahan, and Leila Ettefagh. "Dermoid cyst." (2020).
- Blake WE, Chow CW, Holmes AD, Meara JG. Nasal dermoid sinus cysts: a retrospective review and discussion of investigation and management. Ann Plast Surg. 2006 Nov;57(5):535-40. doi: 10.1097/01.sap.0000229060.20055.07. PMID: 17060735.
- Cavazza, Stefano, et al. "Orbital dermoid cyst of childhood: clinical pathologic findings, classification and management." International ophthalmology 31 (2011): 93-97.
- Choi, June Seok, et al. "Dermoid cysts: epidemiology and diagnostic approach based on clinical experiences." Archives of Plastic Surgery 45.06 (2018): 512-516.
- Eldesouky, Mohammed Ashraf, and Molham Abdelhafez Elbakary. "Orbital dermoid cyst: classification and its impact on surgical management." Seminars in ophthalmology. Vol. 33. No. 2. Taylor & Francis, 2018.
- Dutton, Jonathan J., and George K. Escaravage. "Pediatric orbital tumors." Ophthalmic Oncology (2011): 23-59.
- Shields JA, Shields CL. Orbital cysts of childhood--classification, clinical features, and management. Surv Ophthalmol. 2004 May-Jun;49(3):281-99. doi: 10.1016/j.survophthal.2004.02.001. PMID: 15110666.
- Kerdoud, Ouassime, et al. "Dumbbell-shaped dermoid cyst of the orbit: Case report." Advances in Oral and Maxillofacial Surgery 3 (2021): 100135.
- Van Wyhe RD, Chamata ES, Hollier LH. Midline Craniofacial Masses in Children. Semin Plast Surg. 2016 Nov;30(4):176-180. doi: 10.1055/s-0036-1593482. PMID: 27895540; PMCID: PMC5115923.
- PRATT LW. MIDLINE CYSTS OF THE NASAL DORSUM: EMBRYOLOGIC ORIGIN AND TREATMENT. Laryngoscope. 1965 Jun;75:968-80. doi: 10.1288/00005537-196506000-0010. PMID: 14301067.
- Zapata S, Kearns DB. Nasal dermoids. Curr Opin Otolaryngol Head Neck Surg. 2006 Dec;14(6):406-11. doi: 10.1097/MOO.0b013e32801042db. PMID: 17099348.
- Pensler JM, Bauer BS, Naidich TP. Craniofacial dermoids. Plast Reconstr Surg. 1988 Dec;82(6):953-8. doi: 10.1097/00006534-198812000-00003. PMID: 3200958.
- Rahbar R, Shah P, Mulliken JB, Robson CD, Perez-Atayde AR, Proctor MR, Kenna MA, Scott MR, McGill TJ, Healy GB. The presentation and management of nasal dermoid: a 30-year experience. Arch Otolaryngol Head Neck Surg. 2003 Apr;129(4):464-71. doi: 10.1001/archotol.129.4.464. PMID: 12707196.
- Bloom DC, Carvalho DS, Dory C, Brewster DF, Wickersham JK, Kearns DB. Imaging and surgical approach of nasal dermoids. Int J Pediatr Otorhinolaryngol. 2002 Feb 1;62(2):111-22. doi: 10.1016/s0165-5876(01)00590-0. PMID: 11788143.
- Miller, Craig, Scott Manning, and Randall Bly. "Surgical management of nasal dermoid lesions." Operative Techniques in Otolaryngology-Head and Neck Surgery 30.1 (2019): 16-21.


