Summary Card
Overview
Complex Regional Pain Syndrome (CRPS) is a chronic neuropathic pain disorder that presents with pain disproportionate to the degree of tissue injury and lasts beyond the expected healing time.
Aetiology
The pathophysiology of CRPS is multifactorial, involving dysregulation of the central and peripheral nervous systems, with inflammatory and immunological components.
Clinical Features
Patients present with severe burning pain, often accompanied by sensory, motor, and autonomic disturbances.
Diagnosis
Diagnosis is clinical, using the Budapest Criteria. Adjunct investigations include thermography and bone scintigraphy.
Treatment
CRPS treatment is multidisciplinary, focusing on physical therapy, medications, and surgical options in refractory cases.
Primary Contributor: Dr Waruguru Wanjau, Educational Fellow.
Reviewer: Dr Suzanne Thomson, Educational Fellow.
Overview of CRPS
Complex Regional Pain Syndrome (CRPS) is a neuropathic pain disorder characterized by disproportionate, persistent pain that exceeds the expected time of healing, often accompanied by sensory, vasomotor, sudomotor, and trophic changes.
Complex Regional Pain Syndrome (CRPS) is a chronic condition where the pain experienced is disproportionate to the initial injury and persists far beyond the typical healing period:
It is often accompanied by:
- Allodynia: Pain from non-painful stimuli (e.g., light touch) (He, 2023).
- Hyperalgesia: Exaggerated pain response to painful stimuli.
- Sudomotor Dysfunction: Altered sweating (hyper- or hypohidrosis) (Cheshire, 2020)
- Vasomotor Changes: Skin temperature and color abnormalities.
- Trophic Changes: Alterations in skin, nails, or hair

Classification of CRPS
CRPS is classified by the presence of nerve injury (Type I or Type II) and sympathetic involvement (sympathetically-maintained or independent), with clinical presentations further described as warm (early inflammatory) or cold (chronic autonomic dysfunction).
CRPS is categorized into subtypes based on the presence of nerve damage, sympathetic involvement, and the stage of clinical presentation.
Presence of a Nerve Injury
CRPS is initially classified based on whether a nerve injury is present, which helps differentiate between the two primary subtypes. This is the most common method of CRPS classification.
- Type I (Reflex Sympathetic Dystrophy): no identifiable nerve damage.
- Type II (Causalgia): Associated with documented nerve injury.
Although the clinical presentations are similar, undiagnosed nerve injuries may blur the distinction between these subtypes (Dellon, 2009).
Sympathetic Involvement
Another important classification considers the role of the sympathetic nervous system in maintaining the pain:
- Sympathetically-Maintained Pain (SMP): Pain linked to abnormal sympathetic nervous system activity.
- Sympathetically-Independent Pain (SIP): Pain not related to sympathetic dysfunction.
Temperature
The clinical presentation of CRPS is often further described based on temperature-related characteristics, which indicate the stage of the condition:
- Warm CRPS: Early, inflammatory changes (e.g., warmth, redness).
- Cold CRPS: Chronic autonomic dysfunction with reduced limb temperature.
CRPS often develops within eight weeks of trauma, with some patients showing improvement within three months, while others show little to no improvement even after a year (Brunner, 2017).
Pathophysiology of CRPS
CRPS is triggered by trauma or surgical events, involving dysregulation of sympathetic and central nervous systems, with contributions from genetic, inflammatory, and psychological factors.
CRPS develops through complex interactions between the peripheral and central nervous systems, immune dysfunction, and autonomic dysregulation. These processes, often triggered by trauma or surgery within eight weeks, are influenced by genetic and psychological factors (Ferraro, 2024).
Peripheral Nervous System
Nerve damage or compression leads to heightened pain sensitivity due to nociceptive sensitization (Dellon, 2009)
- Pro-inflammatory mediators (e.g., TNF-α, prostaglandin E2): Lower nerve depolarization thresholds, causing hyperalgesia
- Neuroma formation or compression: Contributes to persistent pain.
Central Nervous System
Abnormal CNS excitability drives exaggerated pain responses.
- Dorsal horn neurons: Increased sensitivity to mechanical and thermal stimuli.
- Neuropeptides (e.g., glutamate, substance P): Lead to hyperpathia (heightened pain perception) and allodynia (pain from non-painful stimuli).
Autonomic Dysregulation
Disruption of the autonomic system intensifies pain by altering adrenergic-nociceptive interactions.
- Sympathetic dysfunction: Pain worsens during or after sympathetic stimulation.
- Temperature changes: Extremities may alternate between warmth (early stages) and coldness (chronic stages).
Immunologic and Inflammatory Factors
Inflammation plays a central role in CRPS onset and persistence (Dey, 2023)
- Elevated mediators: Substance P, CGRP, TNF-α, IL-1β, IL-6, NGF increase peripheral sensitization.
- Autoantibodies: Target adrenergic and muscarinic receptors, suggesting an autoimmune component .
- Inflammatory signs: Redness, swelling, pain, and heat linked to cytokines in serum and cerebrospinal fluid.
Genetic Factors
Genetic predisposition heightens susceptibility to CRPS after injury.
- HLA variations: Increase risk.
- TNF-α polymorphisms: Linked to heightened inflammatory responses (Ferraro, 2024).
Psychological Factors
Emotional stress during or after the injury exacerbates CRPS.
- Stress and distress: Intensify symptoms and complicate management.
- Prognosis: Psychological factors significantly influence recovery outcomes (Dey, 2023).
Stress experienced during injury can amplify symptoms and influence long-term recovery. (Dey, 2023).
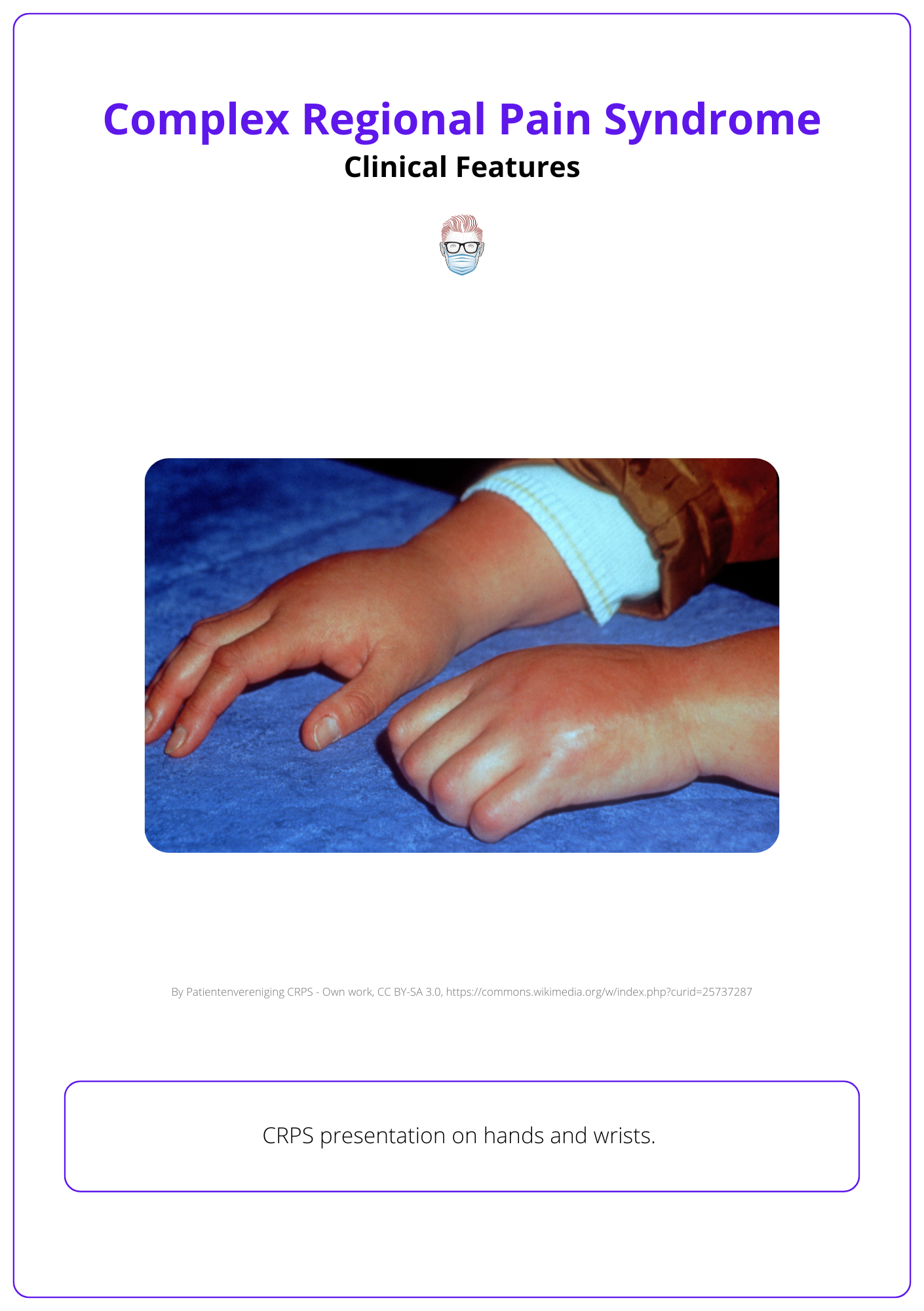
Clinical Features of CRPS
CRPS is characterized by disproportionate pain accompanied by sensory, motor, and autonomic abnormalities, significantly impairing daily function and quality of life.
CRPS encompasses diverse clinical manifestations that evolve over time, making diagnosis and management challenging. It disproportionately affects females and is more prevalent in the upper extremities, occurring in approximately 7% of patients after fractures, surgeries, or limb trauma (Bruhel, 2015).
A Triggering Event
CRPS typically arises following trauma or surgical events (Dey, 2023)
- Fractures: commonest cause - especially high-energy, intra-articular injuries.
- Surgical procedures: Particularly nerve surgery or prolonged anesthesia.
- Sprains, contusions, and crush injuries.
- Minor interventions: Even IV line placements have been associated with CRPS onset (de Mos, 2007).
Surgical interventions, especially those involving prolonged anaesthesia or complex operations, are linked to increased nerve sensitivity, heightening CRPS risk (Dey, 2023; Shin, 2007).
Risk factors for CRPS include asthma, menopause, rheumatoid arthritis, osteoporosis, smoking, and ACE inhibitor use (de Mos, 2007)
Progression
The clinical features of CRPS evolve through distinct stages:
- Early: Increased skin temperature, erythema, swelling, nail & hair growth.
- Later: Decreased hair growth, brittle nails, muscle weakness, pallid, cool skin.
- Chronic: Irreversible muscle atrophy, contractures, intractable pain (Shim, 2019)
CRPS often transitions from warm CRPS (inflammatory changes like redness and warmth) to cold CRPS (autonomic dysfunction with reduced limb temperature) over time (Bruhel, 2015).
Symptoms
CRPS presents with a range of symptoms that overlap and progress over time:
Pain:
- Disproportionate pain exceeding the expected severity of the initial injury.
- Spread: Begins at trauma site & extends without a dermatomal pattern.
- Progressive: Pain increases over time, regardless of the original injury.
Sensory Symptoms:
- Allodynia: Pain triggered by non-painful stimuli like light touch.
- Hyperalgesia: Exaggerated pain response to typically painful stimuli.
Autonomic Symptoms:
- Skin color changes: Redness or pallor.
- Temperature fluctuations: Due to vasomotor dysfunction.
- Sweating: Excessive (hyperhidrosis) or reduced (hypohidrosis) sweating.
- Swelling: Oedema, accompanied by skin color & temperature changes.
Motor Symptoms:
- Weakness: Reduced strength in the affected limb.
- Restricted range of motion: Stiffness and impaired movement.
- Tremors and dystonia: Involuntary contractions
Vasomotor symptoms, including swelling, temperature fluctuations, and skin color changes, are among the most commonly reported features in CRPS (Moss, 2007).
Differential Diagnosis
CRPS shares overlapping features with other conditions, necessitating careful exclusion of:
- Neurological disorders: Guillain-Barré syndrome, multiple sclerosis, poliomyelitis, tabes dorsalis.
- Vascular conditions: Arterial insufficiency, peripheral atherosclerotic disease, phlebothrombosis.
- Other rare causes: Monometric amyotrophy, porphyria.
Diagnosis of CRPS
CRPS is primarily diagnosed clinically using the Budapest Criteria, with imaging and other tools reserved for atypical or unclear cases.
CRPS is a clinical diagnosis guided by the Budapest Criteria, a standardized framework ensuring accuracy in identifying the condition. The diagnosis requires persistent disproportionate pain to the inciting event, along with specific signs and symptoms across sensory, vasomotor, sudomotor, motor & trophic categories (Urits, 2018).
Budapest Criteria for CRPS Diagnosis
The Budapest Criteria classify CRPS based on four distinct categories of symptoms and signs. Diagnosis requires continuing pain disproportionate to the inciting event and fulfillment of specific criteria across these categories.
- Continuing pain disproportionate to the injury or event.
- At least 1 symptom in 3 of 4 categories:
- Sensory: Hyperalgesia or allodynia.
- Vasomotor: Temperature asymmetry or skin color changes.
- Sudomotor/Edema: Sweating asymmetry or edema.
- Motor/Trophic: Decreased range of motion, motor dysfunction (e.g., tremor, dystonia), or trophic changes (skin, hair, nails).
- At least 1 sign in 2 or more categories
- Sensory: Hyperalgesia (pinprick) or allodynia (light touch).
- Vasomotor: Temperature asymmetry or skin color changes.
- Sudomotor/Edema: Sweating asymmetry or edema.
- Motor/Trophic: Reduced range of motion, motor dysfunction, or trophic changes.
- No other diagnosis better explains the signs and symptoms
Diagnostic Adjuncts
When clinical findings are inconclusive, these tools may support the diagnosis:
- Thermography: Detects temperature asymmetry from vasomotor dysfunction.
- Bone Scintigraphy: Identifies altered bone metabolism characteristic of CRPS.
- Electromyography (EMG): Evaluates muscle dysfunction and nerve involvement.
- Musculoskeletal Ultrasonography (MSK US): Assesses structural changes in muscles impacted by CRPS.
Although pain is usually triggered mechanically, both thermal stimuli and psychological stress can exacerbate CRPS symptoms.
Treatment of CRPS
CRPS management combines physical therapy, psychological interventions, medications, and interventional procedures, with surgical options reserved for select cases.
Effective treatment for CRPS requires a multidisciplinary approach to manage symptoms, restore function, and prevent progression. Combining physical rehabilitation, medication, and psychosocial support is critical to improving patient outcomes. In more severe or refractory cases, interventional procedures and surgery may be considered (Ferraro, 2024).
Conservative Management
- Physical Therapy: Maintains range of motion, prevents muscle atrophy, and reduces joint stiffness.
- Occupational Therapy: Helps patients perform daily activities despite physical limitations.
- Psychological Therapy: Cognitive-behavioral therapy (CBT) and other interventions address the emotional toll of chronic pain and improve coping strategies
Medications
Medications are used to manage symptoms and modulate neuropathic pain:
- Anti-Inflammatory Medications: NSAIDs to reduce inflammation and provide pain relief.
- Bisphosphonates: Target bone pain and prevent bone loss.
- Anticonvulsants and Antidepressants: Drugs like gabapentin and amitriptyline help modulate pain pathways.
- NMDA Antagonists: Ketamine reduces pain by targeting central sensitization mechanisms.
- Opioids: Reserved for severe cases where other treatments fail, though long-term use is discouraged due to potential side effects.
Interventional Procedures
For refractory cases, interventional techniques can provide symptom relief:
- Sympathetic Blocks: Injections targeting the sympathetic nervous system to alleviate pain.
- Spinal Cord Stimulation: Devices deliver electrical impulses to the spinal cord, modulating pain signals.
- Dorsal Root Ganglion Stimulation: Targets specific nerve roots for more localized pain control.
Surgical Intervention
Surgery is rarely indicated and is reserved for cases involving nerve injury or compression:
- Surgical Sympathectomy: Cutting part of the sympathetic nervous system may relieve pain in select cases, though outcomes vary (Happak, 2012)
- Nerve Surgery: For neuromas or nerve entrapments contributing to CRPS (Dellon, 2010)
Prognosis
CRPS outcomes vary widely, with most cases resolving within a year. However, some patients develop chronic symptoms, including intractable pain and disability, requiring intensive interventions. Early and aggressive treatment improves the likelihood of recovery (Bruhel, 2015). Long-standing CRPS can by complicated by:
- Dystonia
- Cognitive dysfunction
- Adrenal insufficiency
- Gastroparesis
- Irritable bowel syndrome
The UK Royal College of Physicians, with contributions from the BSSH, provides specific guidelines emphasizing early intervention and multidisciplinary care for CRPS
Conclusion
1. Definition and Types: CRPS is a chronic neuropathic disorder characterized by pain disproportionate to the tissue injury, lasting beyond expected healing. It's categorized into Type I and Type II.
2. Epidemiology: CRPS primarily affects females and is more common in upper extremities. Key risk factors include asthma, menopause, and osteoporosis.
3. Pathophysiology: CRPS involves a complex interaction between the central and peripheral nervous systems, characterized by inflammatory and immune responses, leading to symptoms like allodynia and hyperalgesia.
4. Clinical Presentation: Symptoms include severe burning pain, sensory disturbances like allodynia, motor symptoms such as weakness, and autonomic dysfunctions such as changes in skin temperature and color.
5. Diagnosis: Diagnosis is based on the Budapest Criteria, which require disproportionate pain and specific sensory, vasomotor, sudomotor, and motor symptoms. Diagnostic aids include thermography and bone scintigraphy.
6. Treatment: Management is multidisciplinary; physical therapy, medications, and surgical interventions for refractory cases. Treatments aim to alleviate pain, improve function, and prevent progression.
Further Reading
- Dey S, Guthmiller KB, Varacallo M. Complex Regional Pain Syndrome. [Updated 2023 Aug 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430719/
- Brunner F, Bachmann LM, Perez RSGM, Marinus J, Wertli MM. Painful swelling after a noxious event and the development of complex regional pain syndrome 1: A one-year prospective study. Eur J Pain. 2017 Oct;21(9):1611-1617. doi: 10.1002/ejp.1064. Epub 2017 Jun 2. PMID: 28573699.
- Galer BS, Bruehl S, Harden RN. IASP diagnostic criteria for complex regional pain syndrome: a preliminary empirical validation study. International Association for the Study of Pain. Clin J Pain. 1998 Mar;14(1):48-54. doi: 10.1097/00002508-199803000-00007. PMID: 9535313.
- de Mos M, de Bruijn AG, Huygen FJ, Dieleman JP, Stricker BH, Sturkenboom MC. The incidence of complex regional pain syndrome: a population-based study. Pain. 2007 May;129(1-2):12-20. doi: 10.1016/j.pain.2006.09.008. Epub 2006 Nov 7. PMID: 17084977.
- He Y, Kim PY. Allodynia. [Updated 2023 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537129/
- Cheshire WP. Sudomotor Dysfunction. Semin Neurol. 2020 Oct;40(5):560-568. doi: 10.1055/s-0040-1713847. Epub 2020 Sep 9. PMID: 32906168.
- Bruehl S. Complex regional pain syndrome. BMJ. 2015 Jul 29;351:h2730. doi: 10.1136/bmj.h2730. PMID: 26224572.
- Urits I, Shen AH, Jones MR, Viswanath O, Kaye AD. Complex Regional Pain Syndrome, Current Concepts and Treatment Options. Curr Pain Headache Rep. 2018 Feb 5;22(2):10. doi: 10.1007/s11916-018-0667-7. PMID: 29404787.
- Dellon AL, Andonian E, Rosson GD. CRPS of the upper or lower extremity: surgical treatment outcomes. J Brachial Plex Peripher Nerve Inj. 2009 Feb 20;4:1. doi: 10.1186/1749-7221-4-1. PMID: 19232118; PMCID: PMC2649919.
- Ferraro MC, O'Connell NE, Sommer C, Goebel A, Bultitude JH, Cashin AG, Moseley GL, McAuley JH. Complex regional pain syndrome: advances in epidemiology, pathophysiology, diagnosis, and treatment. Lancet Neurol. 2024 May;23(5):522-533. doi: 10.1016/S1474-4422(24)00076-0. PMID: 38631768.
- Happak W, Sator-Katzenschlager S, Kriechbaumer LK. Surgical treatment of complex regional pain syndrome type II with regional subcutaneous venous sympathectomy. J Trauma Acute Care Surg. 2012 Jun;72(6):1647-53. doi: 10.1097/TA.0b013e318248bfc1. PMID: 22695435.
- Dellon L, Andonian E, Rosson GD. Lower extremity complex regional pain syndrome: long-term outcome after surgical treatment of peripheral pain generators. J Foot Ankle Surg. 2010 Jan-Feb;49(1):33-6. doi: 10.1053/j.jfas.2009.08.003. PMID: 20123284.
- Dellon AL. Surgical Treatment of Upper Extremity Pain. Hand Clin. 2016 Feb;32(1):71-80. doi: 10.1016/j.hcl.2015.08.008. PMID: 26611391.
- UK guideline for CRPS management https://www.rcp.ac.uk/policy-and-campaigns/policy-documents/ Accessed 9th October 2024.


