
Objectives
The following 20 oral questions will assess:
1. Clinical assessment of a cleft lip
2. Identify specific features of a cleft lip
3. Describe the aetiology and genetics of this condition
4. Differ microform, incomplete and Simonart bands
5. Describe the components of a cleft team
6. Pre-operative workup for a cleft patient
7. Surgical techniques and markings of cleft repairs
8. Correction of nasal deformities and alveolar gaps
Section 1
Clinical Assessment of a Cleft Lip
Describe what you see, please.
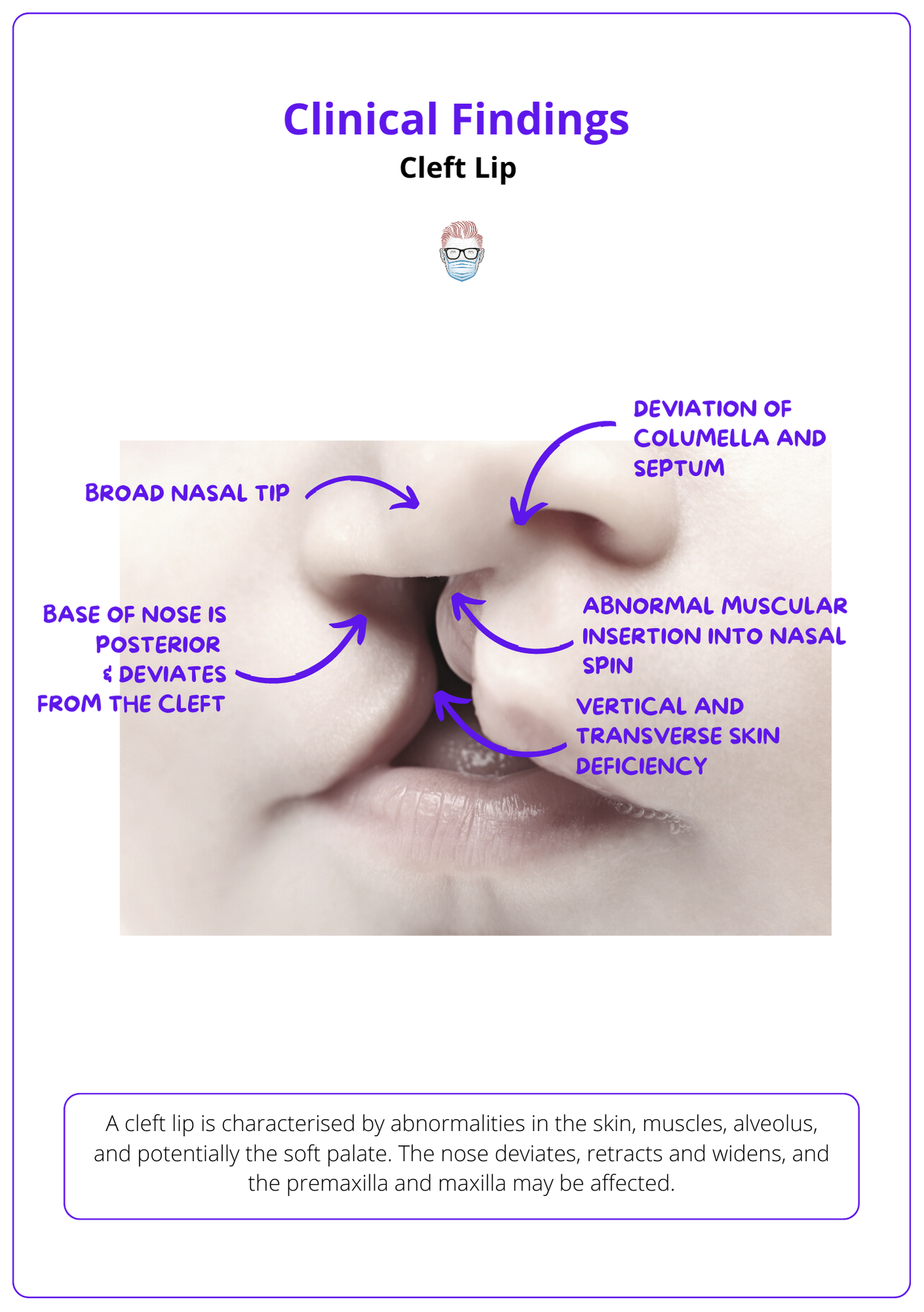
This is a clinical photograph of a complete right-sided cleft lip, alveolus and associated nasal deformity.
Concerning the lip:
- Skin: discontinuity, vertical and transverse deficiency
- Muscle: abnormal insertions into the alar base and nasal spine
- Alveolus: gapping with a hard palate defect.
Concerning the nose:
- Columella, nasal spine and caudal septum deviate away and posterior from the cleft, resulting in dislocation from the vomer groove.
- Nasal tip is broad due to the separation of alar domes and sagging/kinking of the lateral crus on the cleft side.
- Classically on the cleft side, upper and lower lateral cartilages separate and nasal bones flatten.
I would like to conclude my examination by assessing
- Palate: confirm the defect anterior to incisive foramen and no involvement of the soft palate.
- Maxilla: rotated and prominent premaxilla, a retropositioned and hypoplastic lateral maxilla.
- Secondary features: such as lower lip pitting in van der Woude.
What are some key questions to ask in history?
- Obstetric History: antenatal diagnosis, type of delivery, neonatal care
- Risk Factors: Smoking, phenytoin, diabetes, retinoic acid, alcohol
- Family History: cleft lip/palate, syndromes (e.g. van der Woude).
- Social History: home support, employment and domestic issues
- Postnatal: feeding, thriving, airway and psychological concerns
- Knowledge: assessing parental knowledge and timeline of treatments.
What is a cleft lip?
A cleft lip is a congenital malformation of the primary palate (lip, alveolus and hard palate anterior to the incisive foramen). It may be complete or incomplete, bilateral or unilateral, syndromic and non-syndromic.
Why does a cleft lip occur?
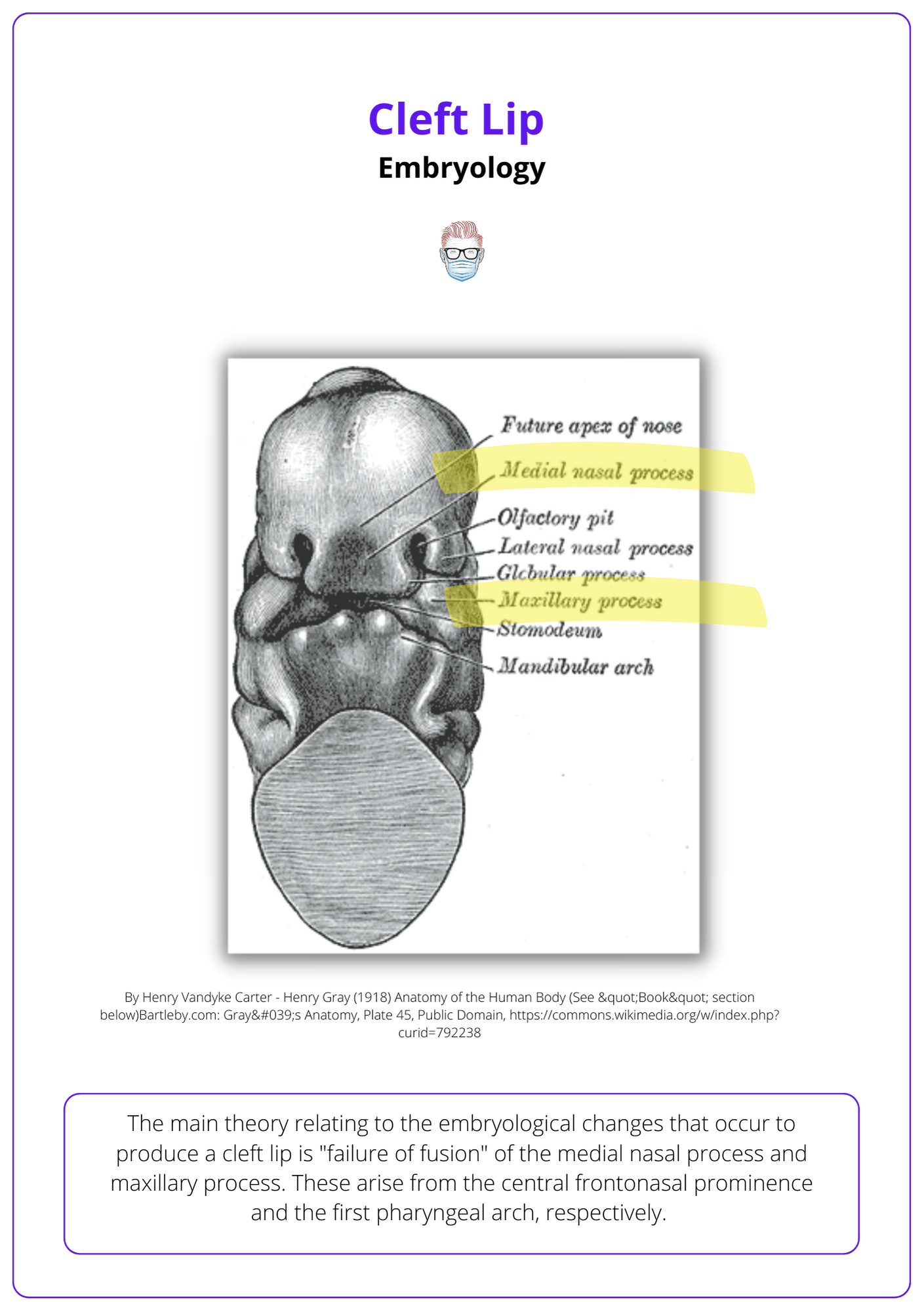
The main theory relating to the embryological changes that produce a cleft lip is "failure of fusion" of the medial nasal and maxillary processes. These arise from the central frontonasal prominence and the first pharyngeal arch.
A unilateral cleft lip occurs when the vomer remains attached to one palatal shelf.
What is the familial risk or incidence of cleft lip?
If there is no family history, the relative risk is 0.1%. This risk increases as the number of family members with cleft increases.
- 1 sibling: 4%
- 1 parent: 7%
- 2 siblings: 9%
- 1 parent and 1 sibling: 17%.
Describe a cleft lip classification system
My personal preference is to "describe what I see":
- Unilateral or bilateral
- Complete or incomplete
- Associated with a cleft palate or submucous cleft
- Syndromic or non-syndrome
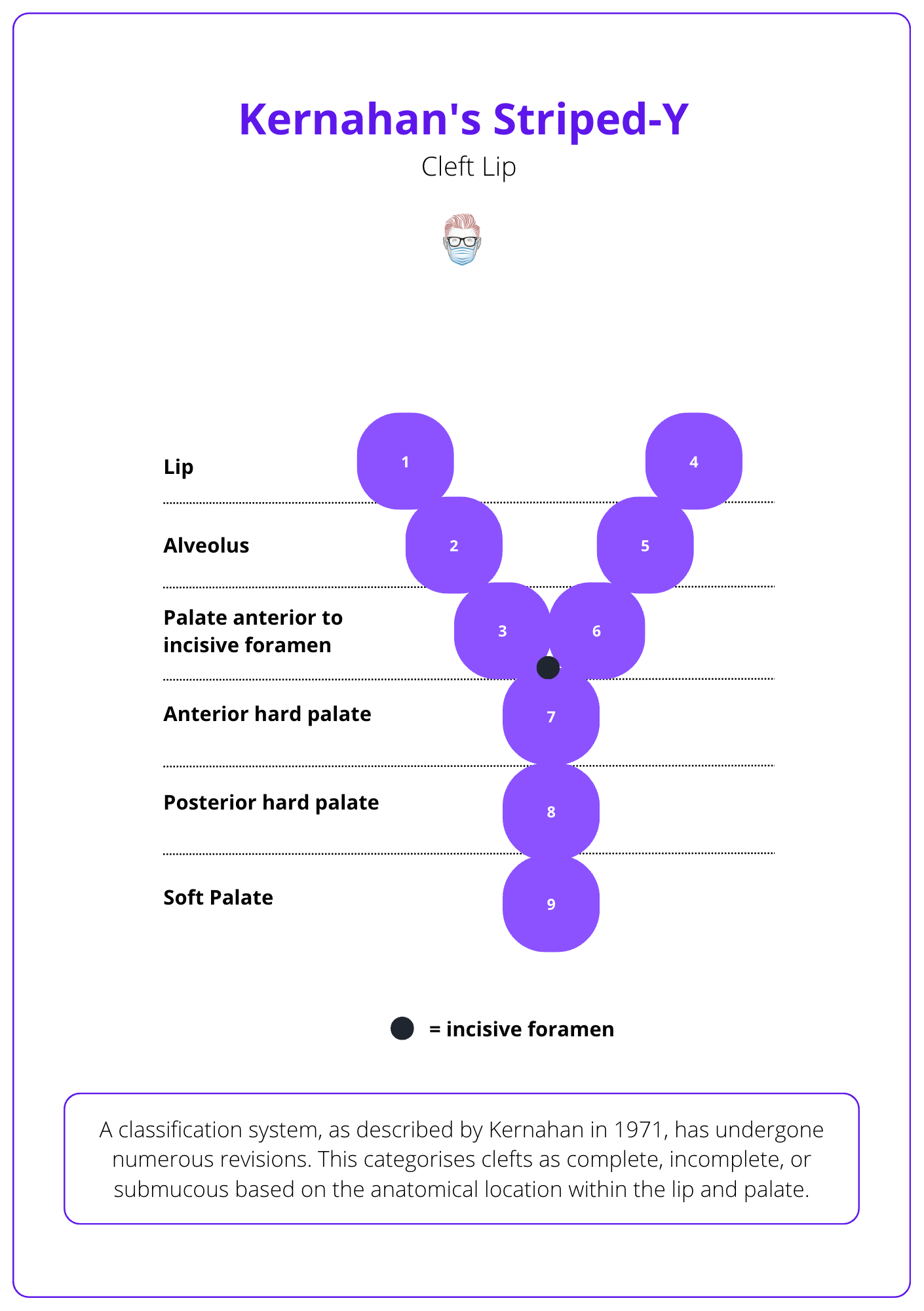
I know other classification systems such as the Veau, Kernahan or LAHSHAL.
- Veau describes cleft lip and palate as 4 groups (soft palate, hard and soft palate, palate through to alveolus, and complete bilateral clefts)
- LAHSHAL represents Lip, Alveolus, Hard Palate and Soft Palate from right to left.
- Kernahan Striped-Y is a graphical classification numbered 1-9. This is drawn below
What is an "incomplete" cleft lip?
A cleft lip with an intact nostril sill, so the full height of the lip is not involved. A mild form of the incomplete cleft is called "forme fruste" or microform, which has features of:
- A vermillion notch
- A nasal ala kink on the cleft side
- A vertical fibrous band from the red line to the nostril floor.

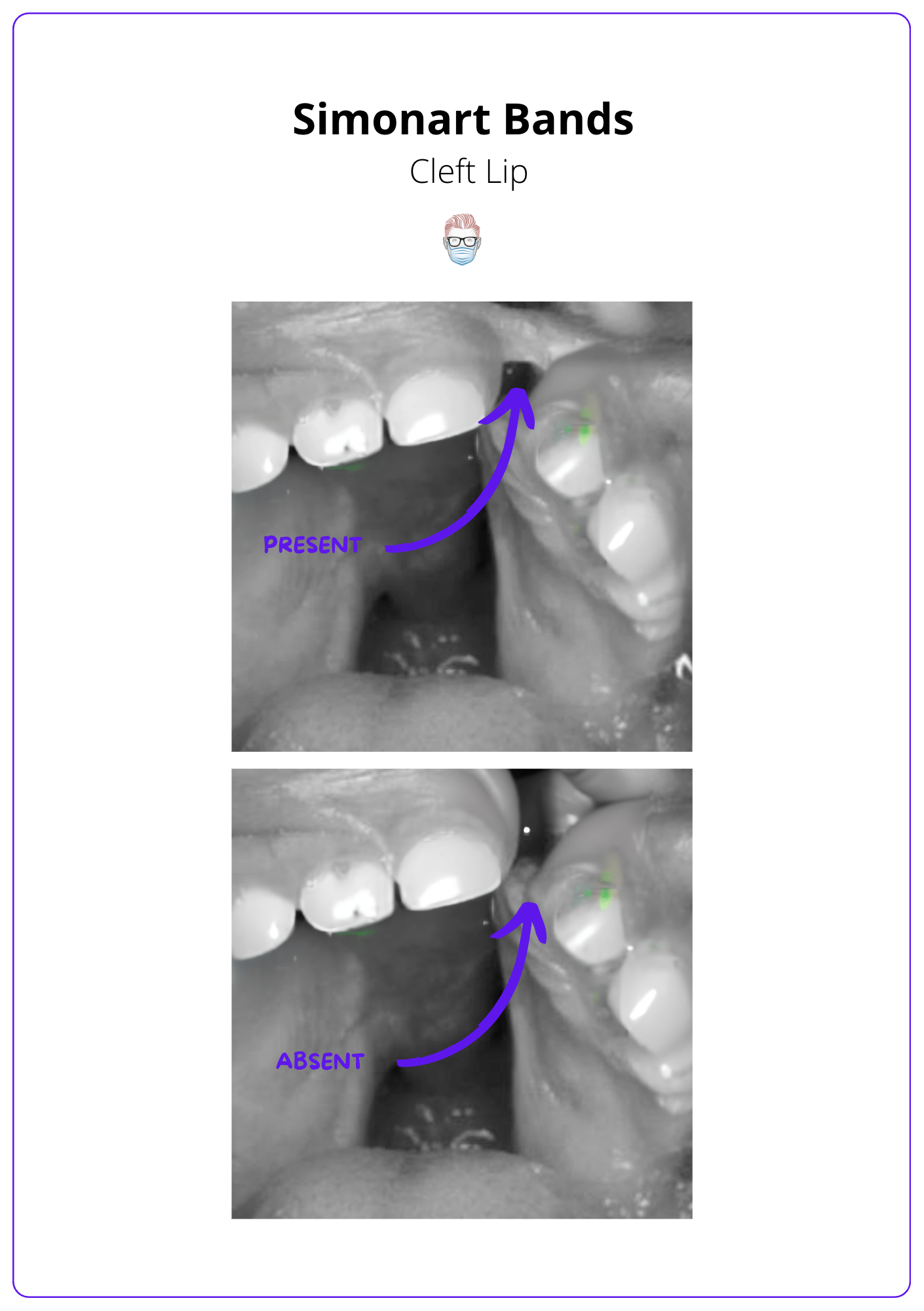
What is a Simonart Band?
A soft tissue bridge that traverses a complete cleft lip. It does not contain any muscle and does not convert a complete into an incomplete cleft lip.
Pictured below.
Explain the cleft diagnosis to the parents
- Congratulate new parents
- Explain cleft lip as a birth defect
- Emphasize multifactorial causes, no specific fault
- Discuss the risks of further siblings if appropriate
- Mention treatable with surgery
- Explain the expected treatment timeline.
- Remind of ongoing support from a specialist MDT.
Section 2
Management of a Cleft Lip
Who is part of a "cleft team"?
- Core Group: Cleft coordinator, patient and their family.
- Surgeons: Plastics, Maxillofacial, ENT, Orthodontist, Dentist,
- Medical: Paediatrician, Neonatologists, Geneticist
- Additional: SLT, psychologist, audiologist, photographer
All team members play important roles in caring for patients with cleft conditions and work together to provide best possible treatment and support
How would you repair this cleft lip?
I will repair the lip and hard anterior palate at 6 months. My department's anaesthetic colleagues prefer a 6-month timeline to reduce anaesthetic risk.
I prefer a Fisher repair and a vomer flap.. I do not routinely use pre-surgical orthodontics or lip adhesion. If there is any remaining cleft in the secondary palate, I will repair this at 12 months.
Do you use pre-surgical orthodontics?
I do not use this technique in my department because of the low level of high-quality evidence to support its use and the significant burden of care. I am aware of its key points, and these include:
- Application of passive or dynamic appliances to narrow the cleft deformity, align the alveolar process and mould the nasal deformity.
- The idea is to make surgical repair easier and improve outcomes
- Evidence does suggest it may have an inhibitory effect on growth.
Would you perform a lip adhesion?
In this patient, I would not perform lip adhesion. I generally reserve this operating for:
- Wide clefts can be converted into less difficult incomplete clefts.
- Bilateral clefts with a protruding maxillary segment
- In patients that can wait 3 months more for definitive lip repair.
I know the technique involving the skin and mucosal flaps designed within future discarded tissue.
Consent the parents for a cleft lip repair
There are intra-operative and post-operative risks that can relate to surgery and the anaesthetic. Specific to a cleft lip repair
- Wound: dehiscence, infection, bleeding, fistula
- Scar: multiple scars that may widen or contract
- Anaesthetic: airway, allergies and barotrauma.
- Multiple surgeries: bleeding or revisions further down the line
As a side note, I often try to highlight the change in facial features early. This often can be an initial shock or surprise to the parents.
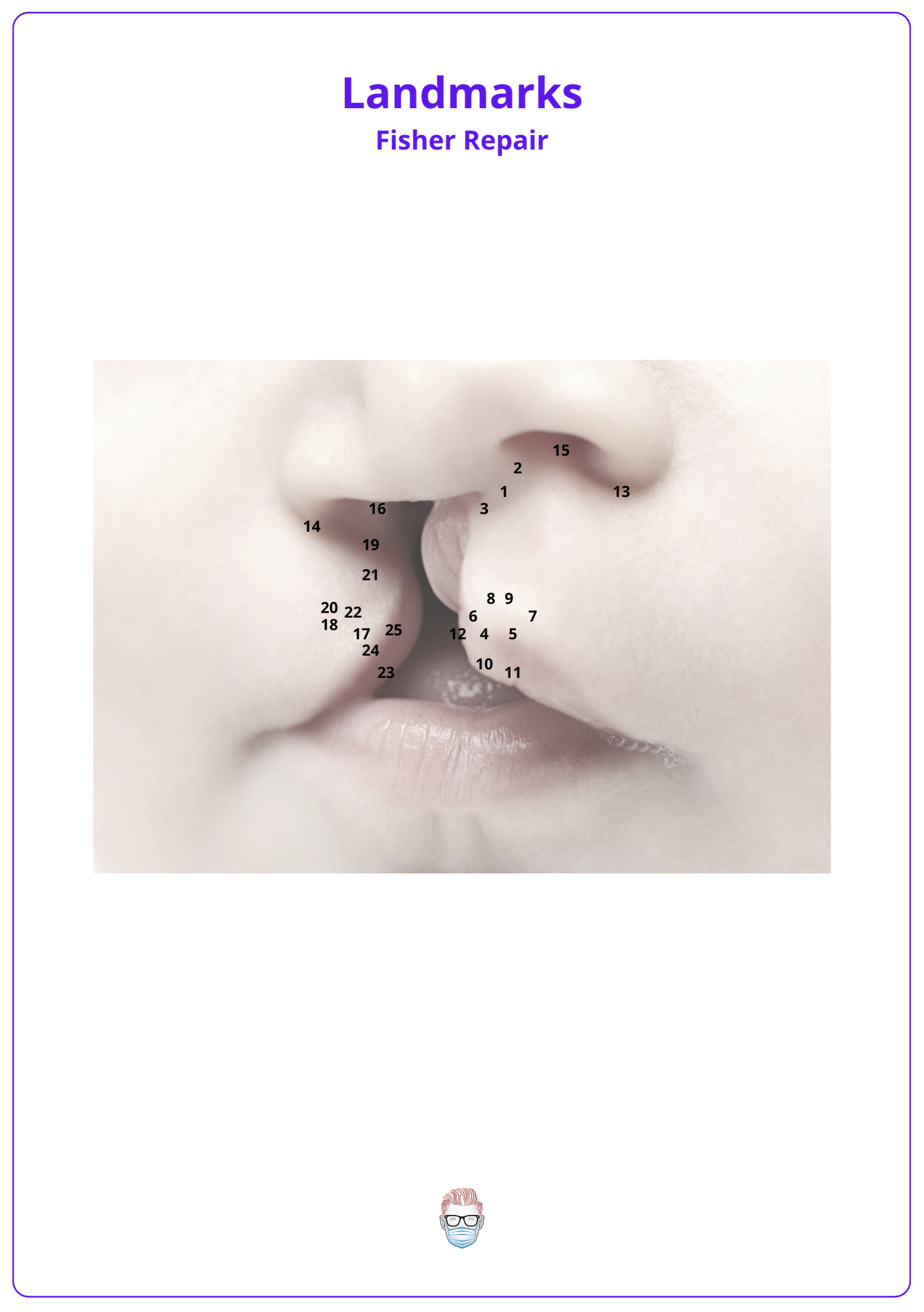
Describe the landmarks in Fisher's unilateral cleft lip repair
25 points can be marked using callipers on the medial lip, nasal floor and lateral lip, as outlined in the initial PRS publication in 2005.
- Point 1: the midline of the philtrum at the columellar base.
- Point 2: height of the non-cleft side philtrum column (mirrors point 3).
- Point 3: height of the cleft-side philtrum column (mirrors point
- Points 4: upper lip midline (the trough of cupids bow)
- Points 5, 6: peaks of Cupid's bow at the vermilion-cutaneous junction.
- Points 7, 8: white-roll cutaneous junctions at each cupid bow peak.
- Point 9: midline of the philtrum (inferior)
- Points 10: at the midline and wet-dry mucosa.
- Points 11, 12: below the peaks of Cupid's bow to form a "red-line"
- Points 13, 14: right and left alar base (inferior point of alar-lip junction)
- Point 15: convexity of sill at lip-columellar crease (symmetric with 16)
- Point 16: height of the lip at the proposed closure in the nostril sill.
- Point 17: cutaneous roll and red line converge medially at the vermilion-cutaneous junction, also known as Noordhoff's point
- Point 18: above the cutaneous roll, perpendicular to the vermilion-cutaneous junction.
- Point 19: the closure point in the nostril sill and is the same distance from point 14 as points 13 to 15 (non-cleft nasal floor width).
- Points 20: between points 18 and 19 (using calipers).
- Point 21: between 19- 20 so lines 19-21 equals 3-16, 20-21 equals 3-8.
- Point 22: forms an isosceles triangle with points 18 and 20. The base of the triangle is equal the required vermilion augmentation (lines 5-11 minus 6-12) and should fit the back cut.
- Point 23: the wet-dry border on the cleft side
- Point 24: along a line connecting points 17 and 23 equal to line 6-12
How do you prep and drape the patient in the theatre?
- General Anaesthetic with endotracheal tube secured to chin midline.
- Position: supine and slight neck extension using a shoulder roll and table at a slight reverse Trendelenburg position.
- Sterile: Prep and drape the face with sterile tapes over the closed eyelids
- Document presurgical photographs
- Markings tattooed with gentian violet dye and a 25-gauge needle.
- Local Anaesthetic: Bilateral infraorbital nerve blocks with infiltration of the cleft-side alar base, piriform rim, and inferior turbinate with 1% lidocaine with epinephrine 1:200,000 (maximum dose, 0.5 ml/kg). No infiltration of the lip is performed.
- Mouth pack inserted.
Describe the steps of medial lip dissection in Fisher's technique
- Incise above the cutaneous roll but not through muscle.
- Discard cleft marginal tissue
- Dissect muscle from overlying skin, vermilion and mucosa.
- Preserve philtral dimple by limiting skin-muscle dissection to 1mm from cut edge.
- Free orbicularis from its columellar base and alveolar cleft margin insertions.
- Position lip and columellar base to predict the final position, and an appropriate downward rotation of the cleft side peak of Cupid’s bow is verified.
- Lateral lip markings can then be altered if necessary.
What other techniques exist for cleft lip repair?
Cleft lip repair techniques can be classified by their movements.
The Millard Rotation Advancement
- Technique: Triangular flap from upper lip advanced into the rotated area of the medial segment.
- Benefits: recreates philtrum, allowing for adjustments to be made during the surgery, and making future revisions easier.
- Limitations: changes to the nose (such as a scar at the base of the nose or constriction of the nostrils) and the lip (such as a short lip or vertical deficiency)
Tennison-Randall Technique
- Technique: 10 markings involving a lower z-plasty
- Benefits: good tension at the alveolar ridge (normal pouting)
- Limitations: challenging to adjust intra-operatively, does not restore philtral column, creates a long lip or vertical excess.
Other techniques to consider include the Skoog, Trauner, Le Mesurier, Delaire, and Rose-Thompson straight-line repair.
How would you correct this patient's nasal deformity?
My preference is for a delayed secondary rhinoplasty. This is because releasing the orbicularis muscles and repairing the cleft will correct some nasal deformities. It also allows delayed correction after nasal and midfacial growth is complete in the patient's teenage years.
I only consider primary nasal surgery in patients with a wide cleft using a limited McComb technique. This involves shortening the nose on the cleft side by repositioning the caudally rotated lower lateral cartilage through percutaneous sutures. More specifically:
- Dorsal supra-cartilaginous dissection
- Separation of cleft alar cartilage from the piriform aperture
- Percutaneous sutures from the nasal lining to alar cartilage and bolsters to lift the cartilage into the correct position.
Other techniques include Anderl and Tajima techniques.
Would you do bone grafting at the time of lip repair?
In my department, I would not do this as the bone may resorb, and it may affect facial growth.
I prefer to perform this at a time of "mixed dentition", about 10 years of age. This is when the permanent canine is about to erupt and can be predicted by monitoring the contralateral canine or x-ray examination.
This is performed under a general anaesthetic and involves
- Preparing the recipient site: raise gingivoperiosteal flaps at the defect and close the nasal mucosa to separate it from the oral cavity.
- Harvest graft: cancellous bone from the iliac crest
- Inset graft: pack it into the defect and close the oral mucosa.


