
Objectives
1. Clinical diagnosis of a central longitudinal deficiency
2. Classify and stage the congenital malformation
3. Describe the aetiology of this condition
5. Order and report on relevant investigations
6. Develop a treatment timeline
7. Describe soft tissue and bony reconstruction options
Section 1
Clinical Assessment
Describe what you see in this clinical photograph.
This patient has clinical features consistent with a left cleft hand. Examining this hand from radial to ulnar
- Thumb is present; it does not appear hypoplastic
- 1st webspace is mildly narrowed
- Central cleft result in divergence of the index and ring finger
- The little finger is unremarkable on inspection
- There is no secondary malformation, such as syndactyly.
To conclude the exam
- Compared to the right hand
- Examine the wrist, elbows, shoulders
- Assess for secondary associations (e.g. EEC - ectrodactyly, ectodermal dysplasia, facial clefts).
- Formal hand assessment to assess movement, prehension and grip.
- Take a detailed history.
So, in summary, this 3-month-old baby has a left-side cleft hand. I would support these clinical findings by following up with relevant investigations.
How do you classify the degree of first webspace narrowing?
This patient has a mildly narrow first webspace. Therefore, it is an IIA as per the Manske and Haliki classification. The grades of this classification are as follows:
- Type I: normal first webspace
- Type II: narrowed (A: mildly, B: severely)
- Type III: thumb-index syndactyly
- Type IV: Index ray suppressed, first web space merged with cleft
- Type V: thumb suppressed, absent first webspace.
What is the classfication of cleft hand?
This patient has a central longitudinal deficiency. The Swanson classification describes this as a failure of formation, and OMT classifies this condition as a malformation.
Explain the core concepts of upper limb embryology
The upper limb develops during weeks 4-8 from 3 axes with specific signalling centres and proteins.
More specifically:
- AP axis "ulnarises" the limb via zone of polarising activity, and sonic hedgehog protein
- PA axes "distalises" the limb via apical ectodermal ridge, and FGFR proteins
- DV axes "dorsalises" the limb via dorsal ectoderm and WNT7A.
You can read more about embryology.
Section 2
Investigations
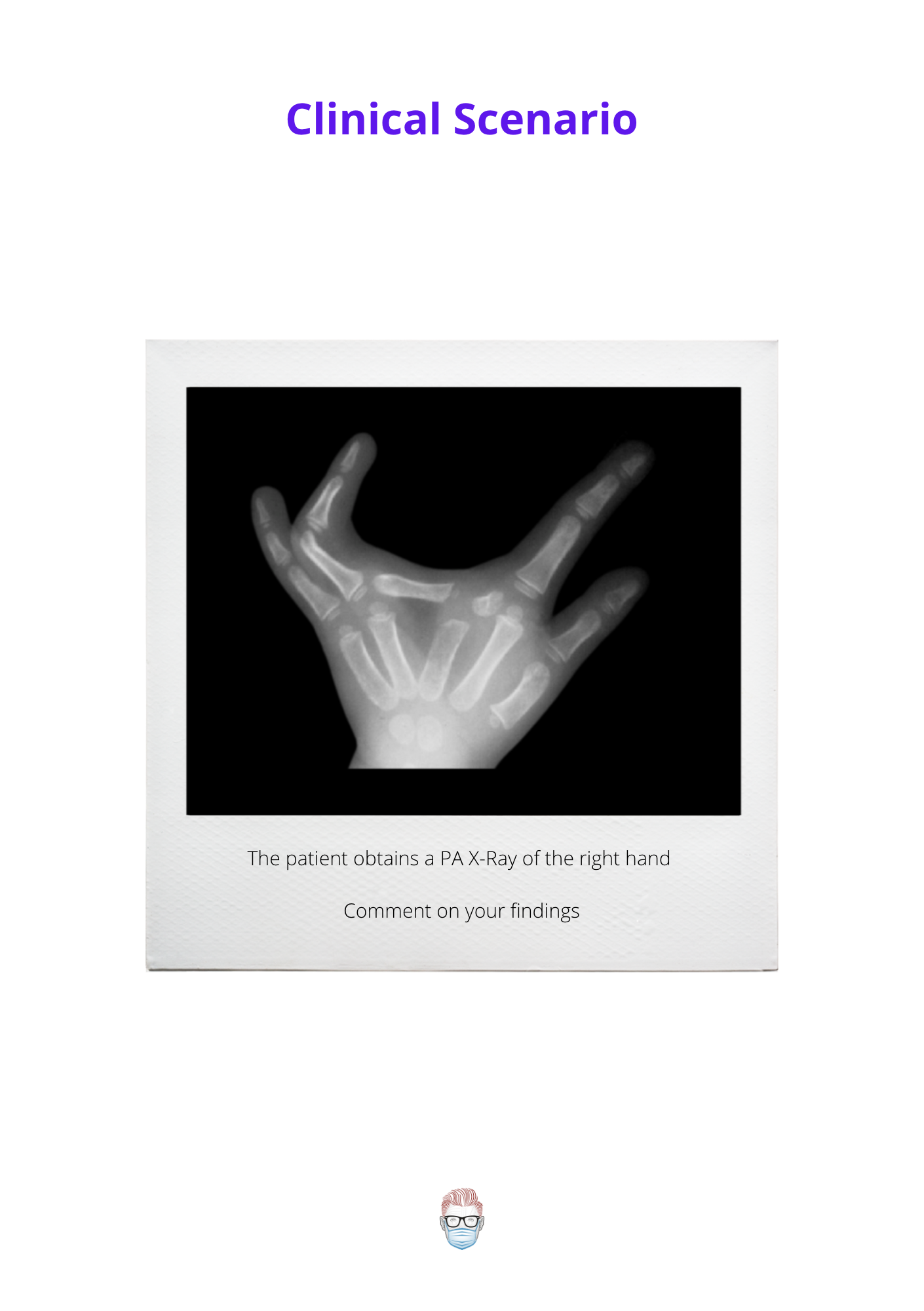
Report the X-Ray above.
This is a PA x-ray of the 3-month-old baby's left hand. It supports the clinical diagnosis of a cleft hand.
Important features to note include:
- The thumb is well formed and not syndactylised to the index
- Transverse bone in the central cleft area. This will only increase the width of the cleft over time.
- The ring and little finger are radiologically normal.
Section 4
Management of Cleft Hand
What are your treatment principles for achieving a cleft hand?
The goals are guided by the patient's clinical and radiological findings. These can include:
- Syndactyly release
- Removal of transverse bones
- First web space reconstruction
- Pollicisation if an absent thumb or free toe transfer
- Correct feet deformity
- Closure of the cleft using the Snow-Littler technique
Would you operate on all patients?
It's important to individualise patient care. During my initial assessment, there are some specific markers I look out for. These include:
- Prehension
- Dexterity
- Impact of QOL/ADLs
- Delayed presentation
If the patient is coping well and has minimal psychosocial issues or impact on quality of life, I would be unlikely to operate.
What is your technique for cleft closure?
I use the Snow-Littler technique for soft tissue and a 2nd-3rd metacarpal transfer for bone reconstruction.
In terms of the Snow-Littler Technique
- Palmar-based flap transposed to the first webspace
- Random-pattern flap that can be axial if volar vessel identified
- The donor site closed primarily with a Barksy flap for the commissure
In terms of bony reconstruction:
- Transfer 2nd metacarpal to the 3rd metacarpal base
- Secured with K-wire.


