Summary Card
Definition
Capsular contracture is the thickening and hardening of the capsule formed around breast implants, leading to breast shape changes, tenderness, and pain.
Aetiology
This is caused by subclinical infection, foreign body reactions, and bacterial seeding. Risk factors include smooth implants, subglandular positioning, periareolar incisions, etc.
Risk Factors
Capsular contracture risk is heightened by factors such as smooth implants, subglandular placement, periareolar incisions, radiotherapy, and biological factors like pregnancy and infection.
Clinical Assessment
A comprehensive triple assessment is required for diagnosis, including a full breast examination, imaging, and a biopsy of any suspicious lesions.
Classification
This presents with breast pain and deformity, graded by Baker's classification from soft (I) to hard and painful (IV). Diagnosis involves a breast exam, MRI, and biopsy of suspicious lesions.
Management
Capsular contracture management depends on severity. Grades 1 and 2 are managed conservatively; grades 3 and 4 require surgery like capsulotomy or capsulectomy.
Primary Contributor: Dr Kurt Lee Chircop, Educational Fellow.
Reviewer: Dr Suzanne Thomson, Educational Fellow.
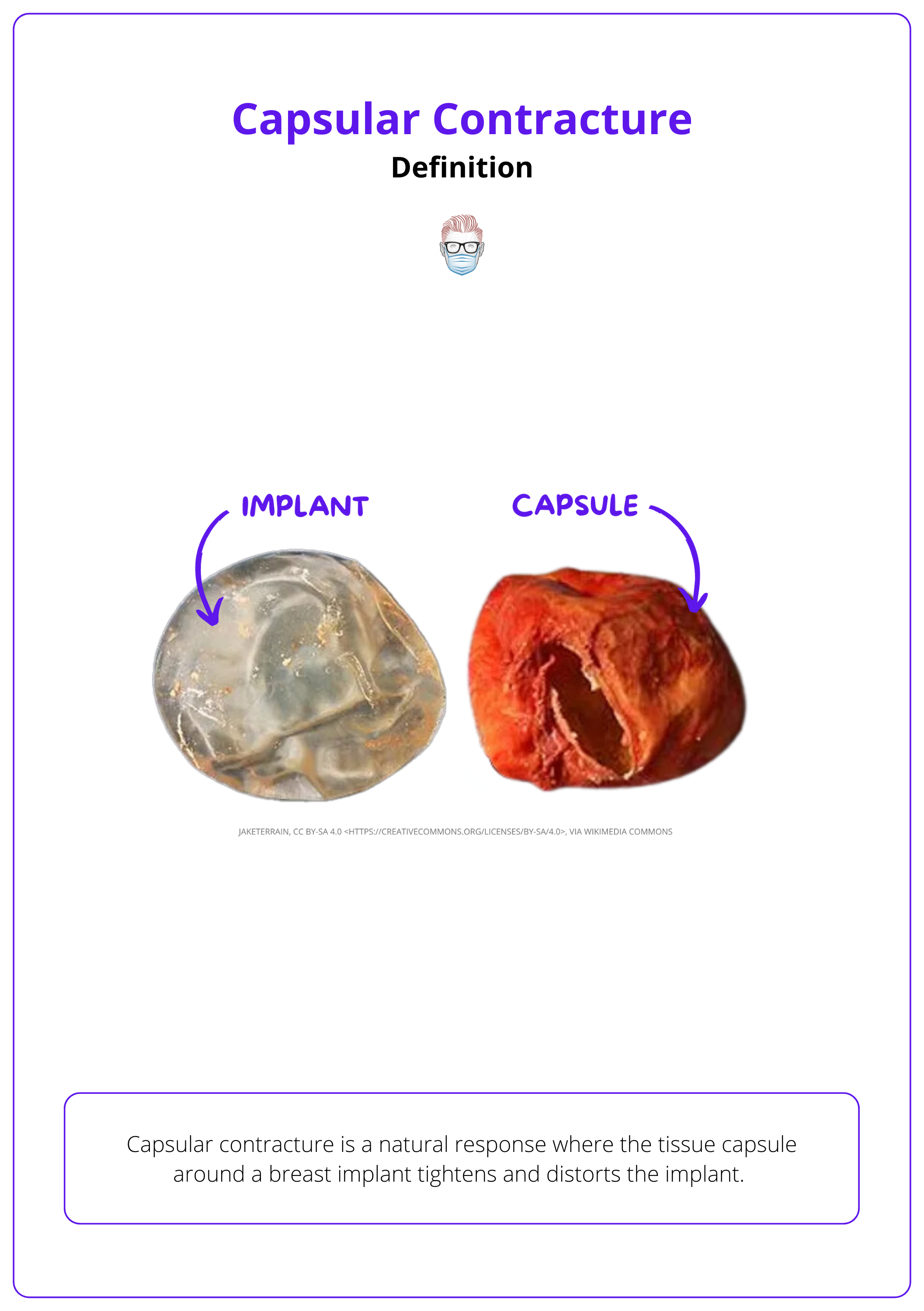
Definition of Capsular Contracture
Capsular contracture is the tightening of a previously normal implant capsule, causing implant distortion.
Capsular contracture is a natural response where the tissue capsule around a breast implant tightens and distorts the implant. The progression typically follows these steps:
- Formation: The capsule forms as a thin and soft layer, initially having minimal impact on the breast's appearance.
- Progresson: Over time, the capsule progressively thickens, hardens, and begins to contract.
- Symptom: As the capsule constricts, it alters the contours of the breast and can lead to symptoms ranging from mild tenderness to severe pain, significantly affecting the appearance and comfort of the breast (Headon, 2015).
The image below illustrates the implant and capsule which can cause capsular contracture.
Aetiology of Capsular Contracture
Capsular contracture's causes include subclinical infections and inflammatory pathways. Higher risks are linked to smooth implants, subglandular positioning, and periareolar incisions.
The pathology of capsular contracture remains uncertain, but multiple aetiological factors have been described. The two most popular ones are:
Subclinical Infective Process
- Correlation is well established, but causation remains uncertain.
- Staphylococcus epidermidis is the most common, though various other bacteria are involved (Dobke, 1995).
Hypertrophic Ccar/Inflammatory Process Hypothesis
- Talc and fibres from operative towels have been found in capsule histologic studies (Chandler, 1999).
- Foreign body reaction is considered a possible cause.
Most early contractures occur within 2 years, with late presentations attributed to systemic bacterial seeding or capsular maturation.
Risk Factors for Capsular Contracture
Capsular contracture risk is heightened by factors such as smooth implants, subglandular placement, periareolar incisions, radiotherapy, and biological factors like pregnancy and infection.
Capsular contracture can be influenced by several factors related to the implant's characteristics and the surgical approach:
Implant Characteristics:
- Surface Type: Smooth implants have shown higher contracture rates compared to textured varieties (Wong, 2006).
- Placement: Implants positioned under the glandular tissue (subglandular) are more prone to contracture than those placed under the muscle.
- Incision Site: Periareolar incisions, which are near the nipple, may introduce bacteria from the breast ducts, increasing the risk of contracture.
Treatment Pathway
- Surgical: Contractures occur more frequently following breast reconstruction than cosmetic augmentation, with a reported incidence of 10.4% at about three years post-surgery.
- Radiotherapy: Exposure to radiation, either before or after surgery, heightens the risk of complications, including contracture, infection, and implant rupture.
While spontaneous swelling is the most common presentation, lumps in the breast or armpit can also indicate BIA-ALCL and should be considered in the differential diagnosis for changes in heavily textured implants (Mercer, 2023).
Chemotherapy does not increase immediate wound complications after implant reconstruction, but its long-term effects on contracture remain unclear (Araco, 2009).
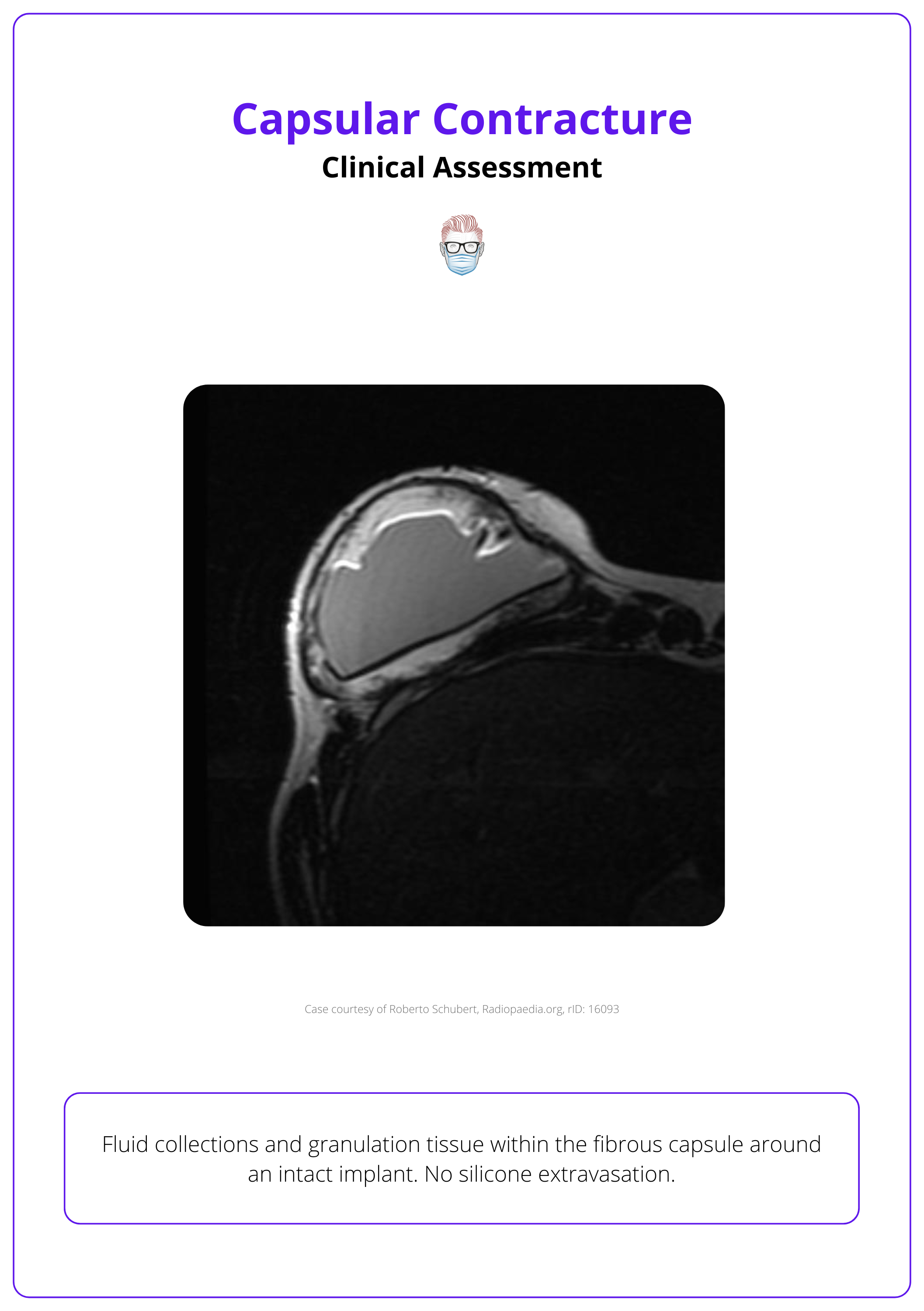
Clinical Assessment of Capsular Contracture
Females present with symptoms such as breast pain or abnormal breast shape. A comprehensive triple assessment is required for diagnosis, including a full breast examination, imaging, and a biopsy of any suspicious lesions.
Females typically present with breast pain or discomfort accompanied by an abnormal or distorted breast shape. These severity of the contracture can be classified as per Baker Classification, which is discussed in the next section.
All patients should undergo a comprehensive triple assessment before diagnosing capsular contracture. This includes:
- Full breast examination
- Imaging (preferably MRI)
- A biopsy of any suspicious lesions
The image below illustrates the fluid collection and granulation tissue within the capsule.
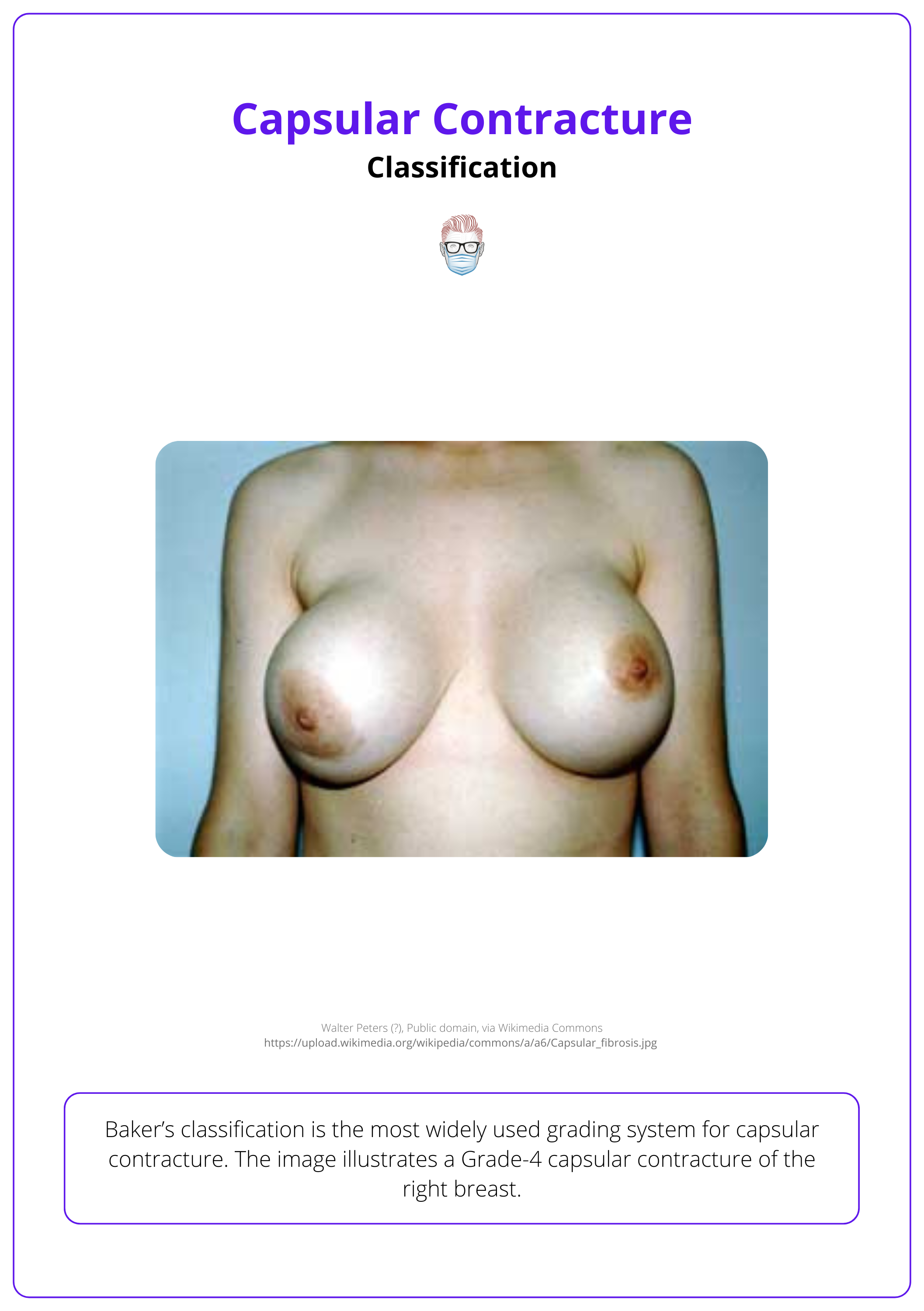
Baker Classification of Capsular Contracture
Capsular contracture is diagnosed using Baker's classification (I-IV), and requires triple assessment before definitive treatment.
Baker’s classification is the most widely used grading system for capsular contracture (Baker, 1995):
- I: Normal, soft, nonpalpable implant
- II: Palpable, minimally firm to touch, not visible
- III: Visible, easily palpated, and moderately firm
- IV: Painful, hard, and breast distorted
This classification system can help guid surgical interventions, which is discussed in the next section.
An example of a Grade IV capsular contracture is depicted in the image below.
Management of Capsular Contracture
Capsular contracture is managed conservatively for mild cases (grades 1 and 2) and surgically for severe cases (grades 3 and 4).
Capsular contracture management is guided by its severity, grading, and the patient's expectations. The condition is graded on a scale from 1 to 4:
Grades 1 and 2:
These milder forms are typically managed conservatively. Management strategies include regular follow-ups and patient counseling to monitor progression and address concerns.
Grades 3 and 4:
Severe capsular contracture requires surgical intervention. The choice between capsulotomy and capsulectomy depends on the contracture's severity, patient health, and surgical experience, with capsulectomy generally providing a more definitive solution (Susini, 2023).
- Implant Removal and Capsulotomy: An open capsulotomy involves multiple incisions to release the capsule's tension, allowing the implant to expand more naturally. This option has a higher rate of recurrence but lower morbidity compared to capsulectomy.
- Implant Removal and Capsulectomy: This procedure can be total—removing both anterior and posterior capsule walls—or partial, typically removing only the anterior wall. Capsulectomy is more definitive but also more invasive, presenting higher morbidity and a lower recurrence rate. It also involves technical challenges such as the potential thinning of anterior soft tissue coverage.
Intra-Op video of Capsular Contracture
Capsulectomy can prevent calcium accumulation in capsules, which can interfere with routine mammography (Araco, 2009).
Specific Considerations for Implant Placement:
- Subglandular Implants: A total capsulectomy is advised to minimize recurrence of contracture.
- Submuscular Implants: A partial capsulectomy is preferable due to the risk of pneumothorax from dissecting closely adhered posterior capsules. Instead, the posterior capsule is usually scored or curetted.
Emerging Treatments and Studies:
Recent retrospective studies suggest acellular dermal matrices may be promising in treating and potentially preventing capsular contracture, though more evidence is needed to confirm their efficacy (Hidalgo, 2020).
In submuscular implants, a partial capsulectomy is preferred to avoid the risk of pneumothorax from dissection near the chest wall. Typically, the posterior capsule is scored or curetted instead.
Conclusion
1. Basics of Capsular Contracture: Gained an understanding of capsular contracture, its definition, aetiology, and physiological processes.
2. Classification and Diagnosis: Learned about Baker's classification system for grading capsular contracture and the importance of a thorough triple assessment for accurate diagnosis.
3. Treatment Options: Explored various management strategies for different grades of capsular contracture, including conservative measures and surgical interventions such as capsulotomy and capsulectomy.
4. Preventative Measures: Reviewed the development of capsular contracture and discussed techniques that may help reduce its occurrence, such as the selection of implant types and surgical techniques.
5. Complications: Identified potential complications associated with capsular contracture and its treatment, and understood the importance of postoperative care to ensure the best outcomes.
Further Reading
- Headon, Hannah, Adbul Kasem, and Kefah Mokbel. "Capsular contracture after breast augmentation: an update for clinical practice. Archives of plastic surgery 42.05 (2015): 532-543.
- Dobke, M. K., Svahn, J. K., Vastine, V. L., Landon, B. N., Stein, P. C., & Parsons, C. L. (1995). Characterization of microbial presence at the surface of silicone mammary implants. Annals of plastic surgery, 34(6), 563–571.
- Chandler P. J., Jr (1999). The deposition of talc in patients with silicone gel-filled breast implants. Plastic and reconstructive surgery, 104(3), 661–668.
- Dancey, Anne, Abdul Nassimizadeh, and Paul Levick. "Capsular contracture–what are the risk factors? A 14 year series of 1400 consecutive augmentations." Journal of plastic, reconstructive & aesthetic surgery 65.2 (2012): 213-218.
- Nichter, L. S., Hardesty, R. A., & Anigian, G. M. (2018). IDEAL IMPLANT Structured Breast Implants: Core Study Results at 6 Years. Plastic and reconstructive surgery, 142(1), 66–75.
- Stevens, W. G., Calobrace, M. B., Alizadeh, K., Zeidler, K. R., Harrington, J. L., & d'Incelli, R. C. (2018). Ten-year Core Study Data for Sientra's Food and Drug Administration-Approved Round and Shaped Breast Implants with Cohesive Silicone Gel. Plastic and reconstructive surgery, 141(4S Sientra Shaped and Round Cohesive Gel Implants), 7S–19S.
- Araco, Antonino, et al. "Capsular contractures: a systematic review." Plastic and reconstructive surgery 124.6 (2009): 1808-1819.
- Spear, Scott L. M.D.; Baker, James L. Jr. M.D.. Classification of Capsular Contracture after Prosthetic Breast Reconstruction. Plastic and Reconstructive Surgery 96(5):p 1119-1123, October 1995.
- Susini, Pietro MD; Nisi, Giuseppe MD; Pierazzi, Diletta Maria MD; Giardino, Francesco Ruben MD; Pozzi, Mirco MD; Grimaldi, Luca MD; Cuomo, Roberto MD. Advances on Capsular Contracture—Prevention and Management Strategies: A Narrative Review of the Literature. Plastic & Reconstructive Surgery-Global Open 11(6):p e5034, June 2023. | DOI: 10.1097/GOX.0000000000005034
- Hidalgo, David A., and Andrew L. Weinstein. "Surgical treatment for capsular contracture: a new paradigm and algorithm." Plastic and Reconstructive Surgery 146.3 (2020): 516-525.
- Dancey A, Nassimizadeh A, Levick P. Capsular contracture - What are the risk factors? A 14 year series of 1400 consecutive augmentations. J Plast Reconstr Aesthet Surg. 2012 Feb;65(2):213-8. doi: 10.1016/j.bjps.2011.09.011. Epub 2011 Sep 17. PMID: 21930448.
- Turton P, El-Sharkawi D, Lyburn I, Sharma B, Mahalingam P, Turner SD, MacNeill F, Johnson L, Hamilton S, Burton C, Mercer N. UK Guidelines on the Diagnosis and Treatment of Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL) on behalf of the Medicines and Healthcare products Regulatory Agency (MHRA) Plastic, Reconstructive and Aesthetic Surgery Expert Advisory Group (PRASEAG). J Plast Reconstr Aesthet Surg. 2021 Jan;74(1):13-29. doi: 10.1016/j.bjps.2020.10.064. Epub 2020 Nov 12. PMID: 33483089.
- Wong CH, Samuel M, Tan BK, Song C. Capsular contracture in subglandular breast augmentation with textured versus smooth breast implants: a systematic review. Plast Reconstr Surg. 2006 Oct;118(5):1224-1236. doi: 10.1097/01.prs.0000237013.50283.d2. PMID: 17016195.


