Summary Card
Overview
Breast ptosis refers to the downward displacement of the nipple-areola complex (NAC) below the inframammary fold (IMF), commonly due to aging, pregnancy, weight fluctuations, and genetics.
Aetiology
Caused by loss of skin elasticity, stretching of Cooper’s ligaments, parenchymal involution, and genetic factors. Lifestyle factors like smoking and poor bra support exacerbate ptosis.
Classification
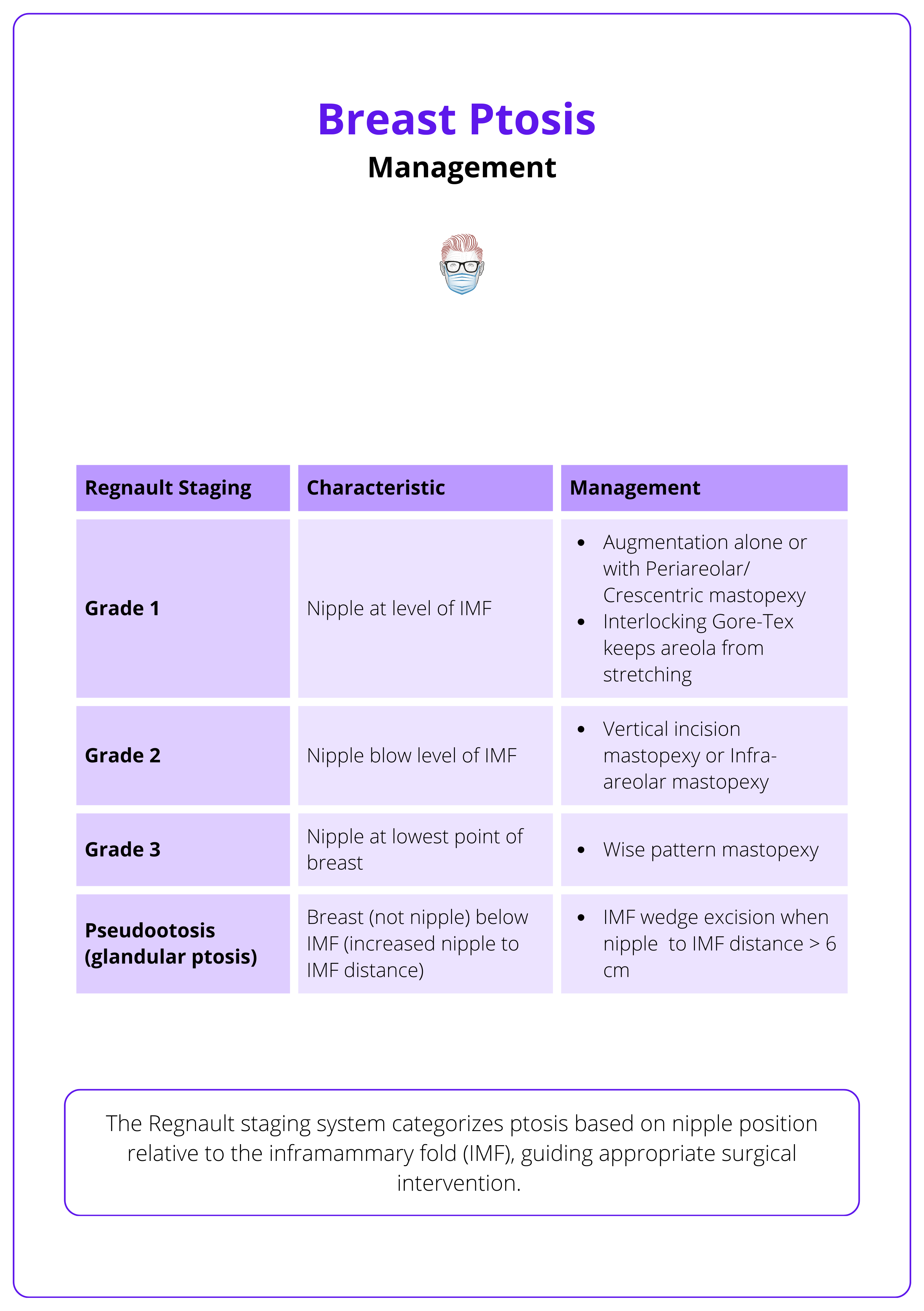
The Regnault classification categorizes ptosis into Grades 1–3 based on nipple position relative to the IMF. Pseudoptosis refers to the sagging of breast tissue with the nipple at or above the IMF.
Clinical Assessment
Evaluation includes key measurements (nipple-to-IMF distance), breast symmetry, skin quality, and imaging (mammography or MRI) in high-risk patients.
Investigations
Preoperative imaging and documentation ensure comprehensive evaluation, especially in high-risk patients.
Treatment Algorithm
Surgical correction of breast ptosis restores shape, symmetry, and proportion via mastopexy, augmentation, or a combination of techniques.
Mastopexy
Mastopexy corrects breast ptosis by repositioning the NAC, reshaping the breast, and removing excess skin, with incision techniques tailored to ptosis severity and patient goals.
Augmentation Mastopexy
Augmentation mastopexy corrects volume loss and ptosis, requiring decisions on surgical staging and procedural sequencing based on ptosis severity and tissue quality.
Complications
Mastopexy and augmentation mastopexy achieve high patient satisfaction. Complications include hematoma, infection, nipple necrosis, capsular contracture, and implant malposition.
Primary Contributor: Hatan Mortada, Educational Fellow
Verified by thePlasticsFella ✅
Overview of Breast Ptosis
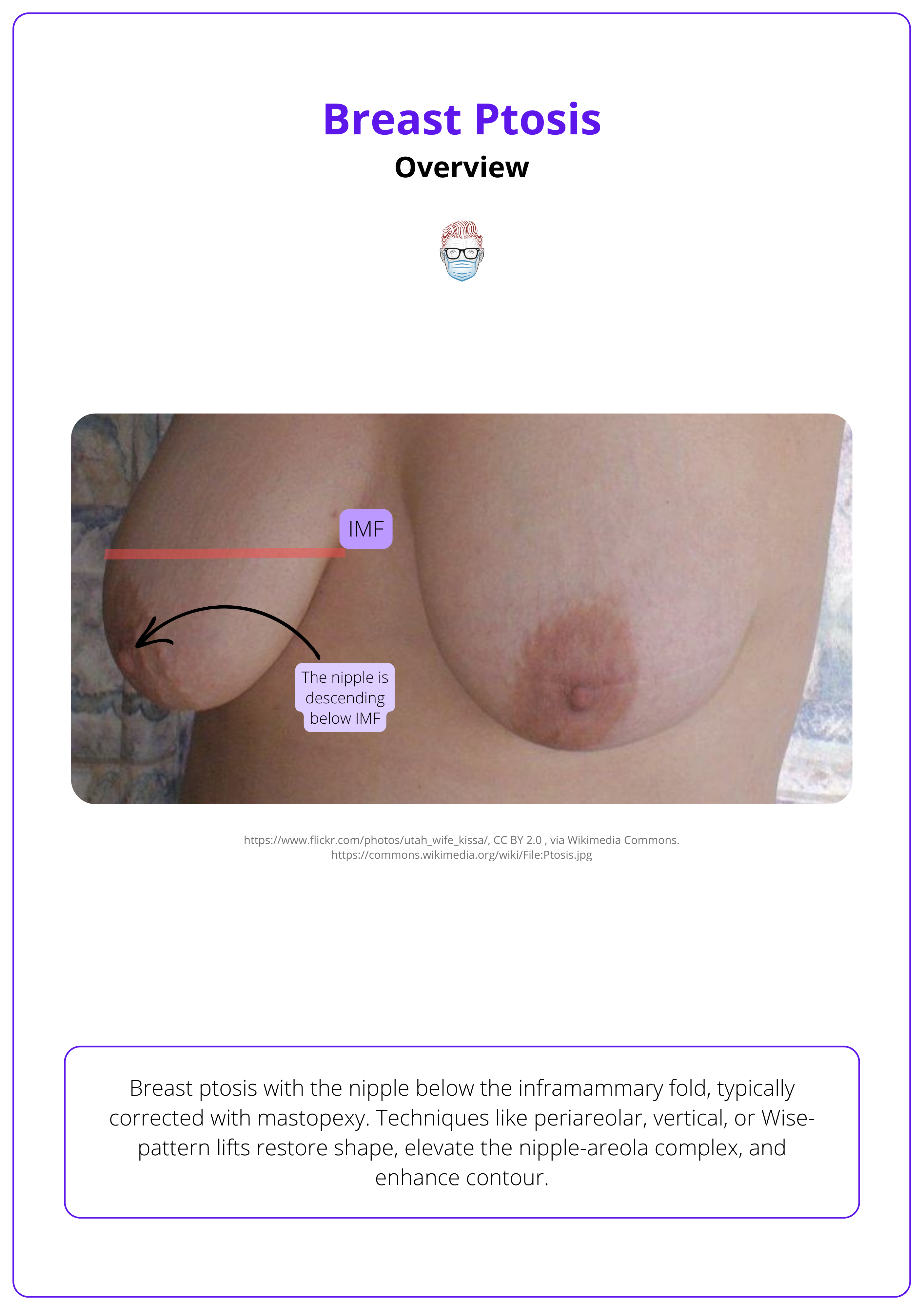
Breast ptosis refers to the descent of the nipple-areola complex (NAC) below the inframammary fold (IMF). It is classified based on severity and often corrected through mastopexy or augmentation.
Breast ptosis is defined as the downward displacement of the nipple-areola complex (NAC) relative to the inframammary fold (IMF). Often accompanied by redundant lower pole skin, ptosis results from the gradual loss of skin firmness, weakening of pectoralis muscles, and stretching of Cooper’s ligaments.
This condition is progressive:
- Early Stages: Uniform descent of both the NAC and glandular tissue. Accompanied by glandular volume loss.
- Advanced Stages: Disproportionate descent of the NAC compared to the gland. Marked asymmetry and sagging.
The image below illustrates breast ptosis.
The word "ptosis" originates from the Greek word "ptōsis," meaning "falling," which describes the downward displacement of the breast.
Aetiology of Breast Ptosis
Breast ptosis results from aging, weight fluctuations, pregnancy, genetics, and lifestyle factors that weaken breast support structures.
Breast ptosis arises from a combination of intrinsic and extrinsic factors that weaken the support structures of the breast.
Intrinsic Factors
- Genetics: Influences breast size, shape, skin quality, and collagen integrity.
- Aging: Causes skin laxity, glandular atrophy, and increased adipose tissue.
- Hormonal Changes: Fluctuations (e.g., estrogen decrease) lead to skin thinning and ligament laxity (Saadat & Kaviani, 2018).
Extrinsic Factors
- Weight Fluctuations: Repeated cycles can stretch Cooper’s ligaments (Rinker, 2010).
- Pregnancy: Hormonal shifts and postpartum volume loss contribute to ptosis (note: breastfeeding is not a direct cause) (Rinker, 2008).
- Lifestyle Factors: Smoking, sun exposure, and inadequate bra support further accelerate the process.
The colloquial term “Cooper's droop” refers to the stretching of Cooper’s ligaments, the natural suspensory elements of the breast.
Classification of Breast Ptosis
The Regnault classification is the most widely used system for assessing breast ptosis, categorizing severity based on the nipple’s position relative to the inframammary fold (IMF).
Breast Ptosis has several classification systems (See, 2023). A standardized classification is essential for accurate assessment and surgical planning.
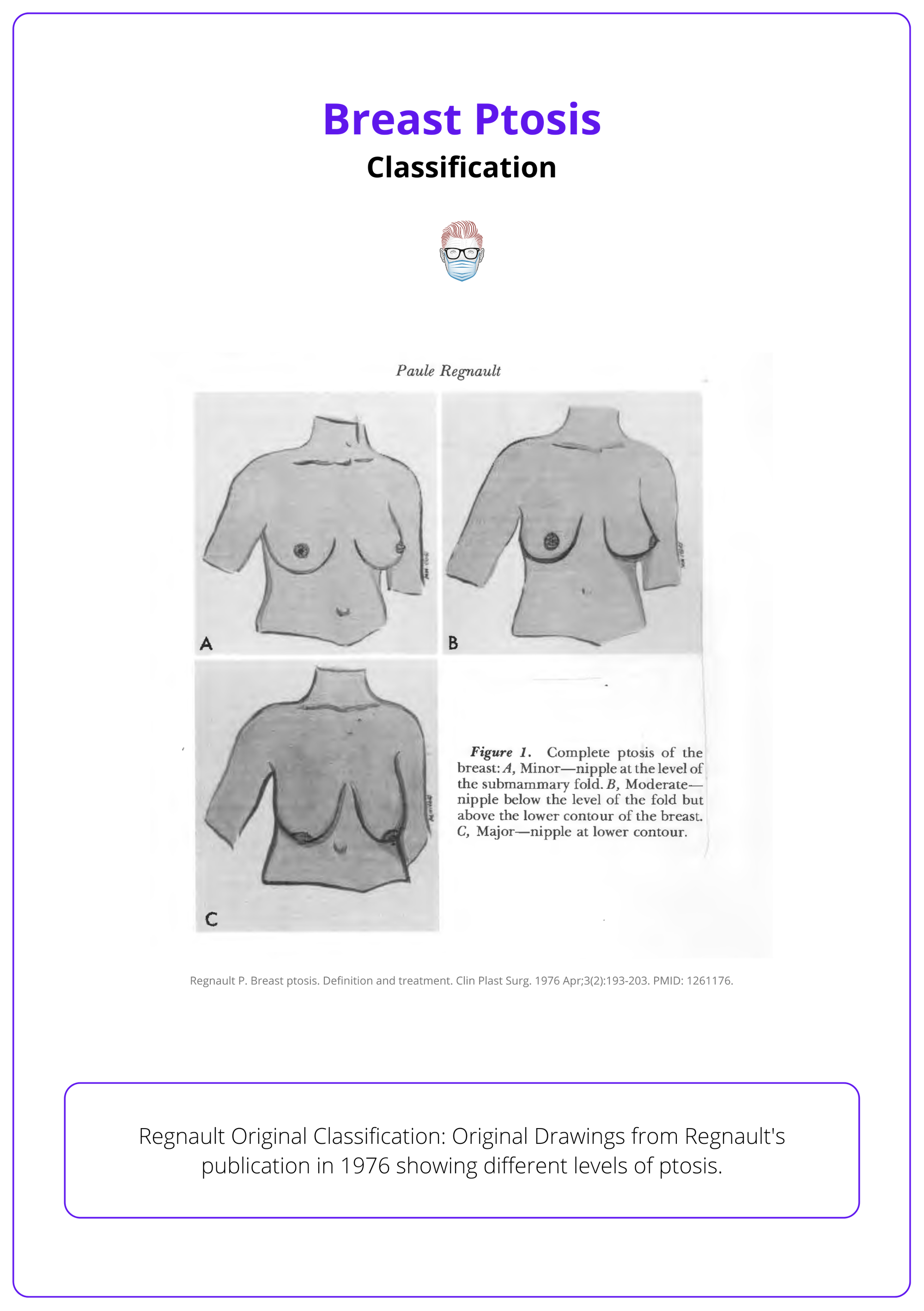
Regnault Classification
The Regnault classification describes breast ptosis in 4 grades. It focuses on the position of the nipple in relation to the IMF.
- Mild: Nipple is at the level of the IMF
- Moderate: Nipple lies below the IMF but remains above the lower breast contour.
- Severe: Nipple is positioned below both the IMF and the lower contour.
- Pseudoptosis: nipple above IMF, but loose skin creates a ptotic appearance.
Severe ptosis is often associated with glandular tissue loss, deflation, and lateral/axillary fullness. Pseudoptosis typically results from hypoplasia due to weight loss or pregnancy
The image below illustrates the original drawings from Regnault's publication in 1976 showing different levels of ptosis.
Other Classifications
- Vandenbussche (1992): Categorizes ptosis based on etiology.
- Velasco (2004): Focuses on postpartum ptosis, classifying it into four stages.
- Kirwan (2002): Uses a 1-cm staging system (A–F), where Stage A represents a nipple 2 cm above the IMF, and Stage F indicates >2 cm below the IMF.
In pseudoptosis, the nipple-to-IMF distance increases while the sternal notch-to-nipple distance remains stable.
Clinical Assessment of Breast Ptosis
A comprehensive assessment of breast ptosis includes a detailed history, physical examination, and key measurements to guide surgical planning and optimize patient outcomes.
A thorough clinical assessment evaluates breast ptosis, asymmetries, and surgical risks. Identifying factors like smoking, high BMI, and prior surgeries helps reduce complications and improve outcomes.
History & Patient Goals
- Expectations: Understand the desired aesthetic outcome.
- Changes Over Time: Consider postpartum changes, weight fluctuations, and menopausal effects.
- Family and Surgical History: Assess for breast cancer risk and previous surgeries that may affect vascularity.
- Risk Factors: Smoking, high BMI, prior surgeries, and chronic conditions (e.g., diabetes) can increase postoperative complications.
Physical Examination
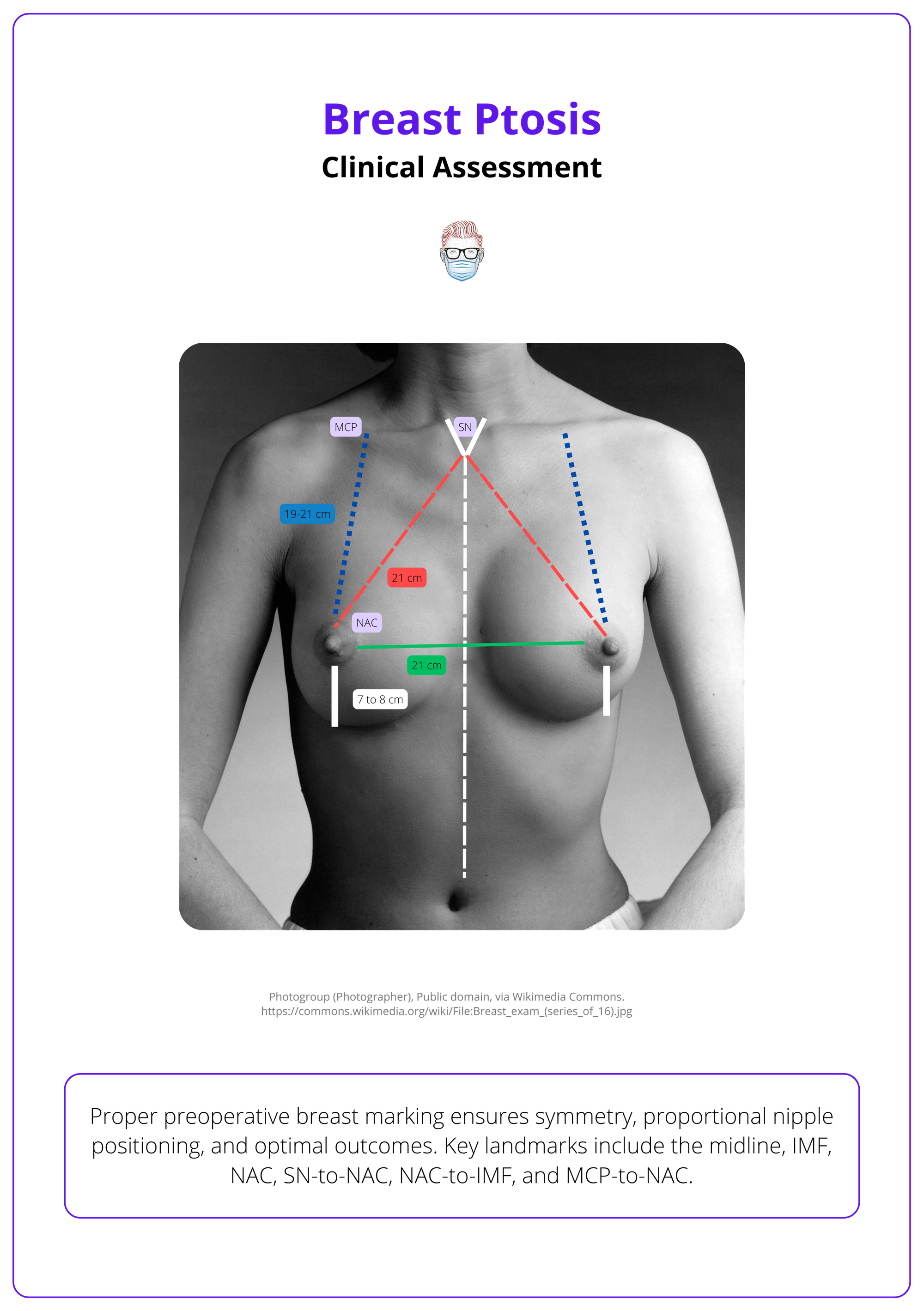
Evaluate for asymmetries, volume deficits, and skin redundancy. Assess tissue elasticity and dermal integrity. Key measurements on examination include:
- Nipple-to-IMF: Assesses ptosis severity.
- Suprasternal Notch-to-Nipple: Evaluates breast position on the chest.
- Breast Width: Useful for determining implant size in augmentation cases.
Always measure nipple-to-IMF distance in an upright, neutral position to ensure accuracy and consistency in surgical planning.
The image below shows preoperative marking and key landmarks.
Inter-observer reliability of clinical measurements has been found to be good, though slight variability exists (Hansson, 2014).
Investigations for Breast Ptosis
Preoperative imaging and documentation are essential for comprehensive evaluation, particularly in high-risk patients.
Investigations assess breast anatomy, ptosis severity, and risks. Imaging, photography, and measurements guide surgical planning, patient education, and postoperative comparison.
- Imaging: Screening mammography or breast MRI as indicated for cancer risk assessment.
- Clinical Photography: Document preoperative findings for patient education and legal records.
- Anthropometric and Advanced Measurements: Emerging methods like 3D stereophotogrammetry provide accurate breast volume and ptosis assessment (Huang, 2017).
For patients under 40, use ultrasound for preoperative imaging. For those over 40 or high-risk patients, opt for MRI or mammography to screen for malignancies before mastopexy.
Treatment Algorithm for Breast Ptosis
Surgical correction of breast ptosis restores shape, symmetry, and proportion via mastopexy, augmentation, or a combination of techniques.
The management of breast ptosis involves mastopexy, augmentation, or a combination of both. This can be performed in a single-stage or a two-stage approach, depending on tissue quality, implant size, and procedural complexity.
Treatment of breast ptosis is tailored to ptosis severity, patient goals, and long-term outcomes. A general guide is as follows.
- Mild: Grade I ptosis: Augmentation or periareolar mastopexy.
- Moderate: Grade II ptosis: Vertical or infra-areolar mastopexy.
- Severe : Grade III ptosis: Wise pattern mastopexy.
This treatment algorithm for breast ptosis is illustrated below.
Mastopexy for Breast Ptosis
Mastopexy corrects breast ptosis by repositioning the NAC, reshaping the breast, and removing excess skin, with incision techniques tailored to ptosis severity and patient goals.
Mastopexy remains the cornerstone of surgical correction for breast ptosis. The technique and incision pattern are tailored to ptosis severity, skin quality, and patient goals. The goals of this procedure are:
- Reposition the nipple-areola complex (NAC) for natural projection.
- Reshape and symmetrize the breast to enhance contour.
- Remove excess skin to restore firmness and improve aesthetics.
Incision Techniques
The choice of incision depends on breast anatomy, patient preferences, and the extent of correction needed.
- Wise-pattern: Severe ptosis, allows maximum lift and skin removal.
- Vertical (Lollipop): Moderate ptosis, providing lift with fewer scars.
- Periareolar: Mild ptosis, often combined with augmentation.
For optimal outcomes, aim for a sternal notch-to-nipple (SSN-N) distance of 21–23 cm and an inferior limb of 5–7 cm. Positioning the nipple at Pitanguy’s point along the breast meridian yields a natural appearance
Augmentation-Mastopexy for Breast Ptosis
Augmentation mastopexy corrects volume loss and ptosis, requiring decisions on surgical staging and procedural sequencing based on ptosis severity and tissue quality.
Augmentation mastopexy combines breast implants and a mastopexy to correct both volume loss and ptosis. Two important decisions should be made based on ptosis severity, skin quality, implant size, and patient goals.
- Single-stage or two-stage procedure
- Mastopexy first or augmentation first
Single-Stage vs. Two-Stage Approach
- Single-stage: Suitable for mild ptosis with minimal volume loss. It increases the risk of complications in patients with compromised tissue quality or large implants but can be safely performed (Sanniec, 2019).
- Two-stage procedures: Recommended for significant ptosis or compromised skin quality to reduce risks of recurrent sagging and implant malposition. It allows greater control over nipple positioning, skin adaptation, and soft tissue. This has a lower revision/complication rate (Lindsay, 2010).
If ptosis is borderline, augmentation alone may provide sufficient lift. However, if the nipple remains low postoperatively, a secondary mastopexy will be required.
Mastopexy-First vs. Augment-First Approach
Mastopexy-First
This is best suited for moderate to severe ptosis with adequate native breast volume.
- Benefits: Ensures precise nipple-areola repositioning before adding volume. Allows tissue contraction and remodeling before placing an implant.
- Limitation: Requires a second procedure if implants are desired later.
Augmentation-First
This is suitable for mild ptosis with volume loss, where implants may provide adequate lift. This is ideal for patients with small breasts primarily seeking augmentation.
- Benefits: Potentially eliminating the need for mastopexy if the implant provides sufficient lift.
- Limitations: Risk of waterfall deformity if ptosis correction is insufficient.
Implant volume directly affects NAC positioning due to the lift effect from augmentation. More specifically,
- ≤225 cc: Approximate SSN-N distance of 21 cm.
- 250–325 cc: Approximate distance of 22 cm.
- ≥350 cc: Approximate distance of 23 cm
For mastopexy after implant removal, delay surgery at least 3 months if breast tissue is <4 cm or nipple elevation >4 cm is needed. This allows tissue remodeling and reduces NAC compromise risk.
Complications of Breast Ptosis Treatment
Mastopexy and augmentation mastopexy achieve high patient satisfaction. Complications include hematoma, infection, nipple necrosis, capsular contracture, and implant malposition.
While outcomes are generally favorable, awareness of potential complications is essential for risk management and patient counseling.
Early Complications
- Hematoma: May require prompt surgical evacuation.
- Infection: Particularly in augmentation-mastopexy; may necessitate antibiotics or implant removal.
- Nipple Necrosis: Higher risk in smokers or those with compromised vascularity.
- Fat Necrosis: Can lead to palpable nodules.
Long-Term Complications
- Capsular Contracture: Results in implant hardening or distortion.
- Implant Rippling: More common with subglandular placement or thin soft tissue.
- Areolar Spreading: Particularly with periareolar mastopexy.
- Nipple Malposition and Recurrent Ptosis: May require revision procedures.
- Implant Malposition: Can result from postoperative tissue stretch or imprecise pocket dissection.
The final postoperative breast shape evolves over 6–12 months as tissue relaxation occurs, often leading to a more natural contour.
Conclusion
1. Overview: Breast ptosis is the downward displacement of the nipple-areola complex (NAC) below the inframammary fold (IMF), commonly caused by aging, pregnancy, weight changes, and genetics.
2. Aetiology: Ptosis results from skin elasticity loss, Cooper’s ligament stretching, parenchymal involution, and lifestyle factors like smoking and poor bra support.
3. Classification & Assessment: The Regnault system grades ptosis (1–3) based on nipple position relative to the IMF. Assessment includes nipple-to-IMF measurements, skin quality, and imaging if high risk.
4. Management & Complications: Treatment involves mastopexy, augmentation mastopexy, or reduction mammoplasty, with complications including hematoma, infection, nipple necrosis, and capsular contracture.
Further Reading
- Hidalgo DA, Spector JA. Mastopexy. Plast Reconstr Surg. 2013;132(4):642e-656e. doi:10.1097/PRS.0b013e31829fe4b4
- See MH, Yip KC, Teh MS, et al. Classification and assessment techniques of breast ptosis: A systematic review. J Plast Reconstr Aesthet Surg. 2023;83:380-395. doi:10.1016/j.bjps.2023.04.003
- Martinez AA, Chung S. Breast Ptosis. [Updated 2023 Nov 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK567792/
- Kirwan L. A classification and algorithm for treatment of breast ptosis. Aesthet Surg J. 2002;22(4):355-363. doi:10.1067/maj.2002.126746
- Pferdehirt R, Nahabedian MY. Finesse in Mastopexy and Augmentation Mastopexy. Plast Reconstr Surg. 2021;148(3):451e-461e. doi:10.1097/PRS.0000000000008303
- Ali A Qureshi, Terence M Myckatyn, Marissa M Tenenbaum, Mastopexy and Mastopexy-Augmentation, Aesthetic Surgery Journal, Volume 38, Issue 4, April 2018, Pages 374–384, https://doi.org/10.1093/asj/sjx181
- Ramanadham SR, Rose Johnson A. Breast Lift with and without Implant: A Synopsis and Primer for the Plastic Surgeon. Plast Reconstr Surg Glob Open. 2020;8(10):e3057. Published 2020 Oct 28. doi:10.1097/GOX.0000000000003057
- Abdelkader R, Raafat S, Sakr W, Abdelaziz M, ElNoamany S. Augmentation Mastopexy: A Five-step Standardized Strategy Approach. Plast Reconstr Surg Glob Open. 2022;10(6):e4349. Published 2022 Jun 15. doi:10.1097/GOX.0000000000004349
- Payer J, Chalkidis N, Polackova P, Patzelt M. MAMAS (mastopexy-augmentation made applicable and safer): A standardized template of pre-operative marking and step-by-step surgical procedure. JPRAS Open. 2024;40:293-304. Published 2024 Mar 27. doi:10.1016/j.jpra.2024.03.007
- Marrella D, Tornambene R, Delia G, Stagno d'Alcontres F. Marking the nipple-areola complex in mastopexy and reduction mammoplasty: a geometrical method. Updates Surg. 2024;76(4):1553-1558. doi:10.1007/s13304-024-01765-y


