Bone Grafts
1. Bone grafts are autologous (humans) or alloplastic (engineered)
2. Autologous grafts are autografts (patient) or allografts (cadaver)
3. They are incorporated through osteoinduction, -conduction, -genesis
4. Cortical grafts support, and cancellous allow bone regrowth.
5. Graft survival depends on type of graft, fixation and patient factors.
Indications for bone grafts
There is a diverse array of bone grafting indications. Generally speaking, bone grafts and their substitutes are used for:
- Structural support by filling bone gaps secondary to trauma or resection
- Improve healing of fractures with delayed or non-unions.
- Assist in arthrodeses and spinal fusions
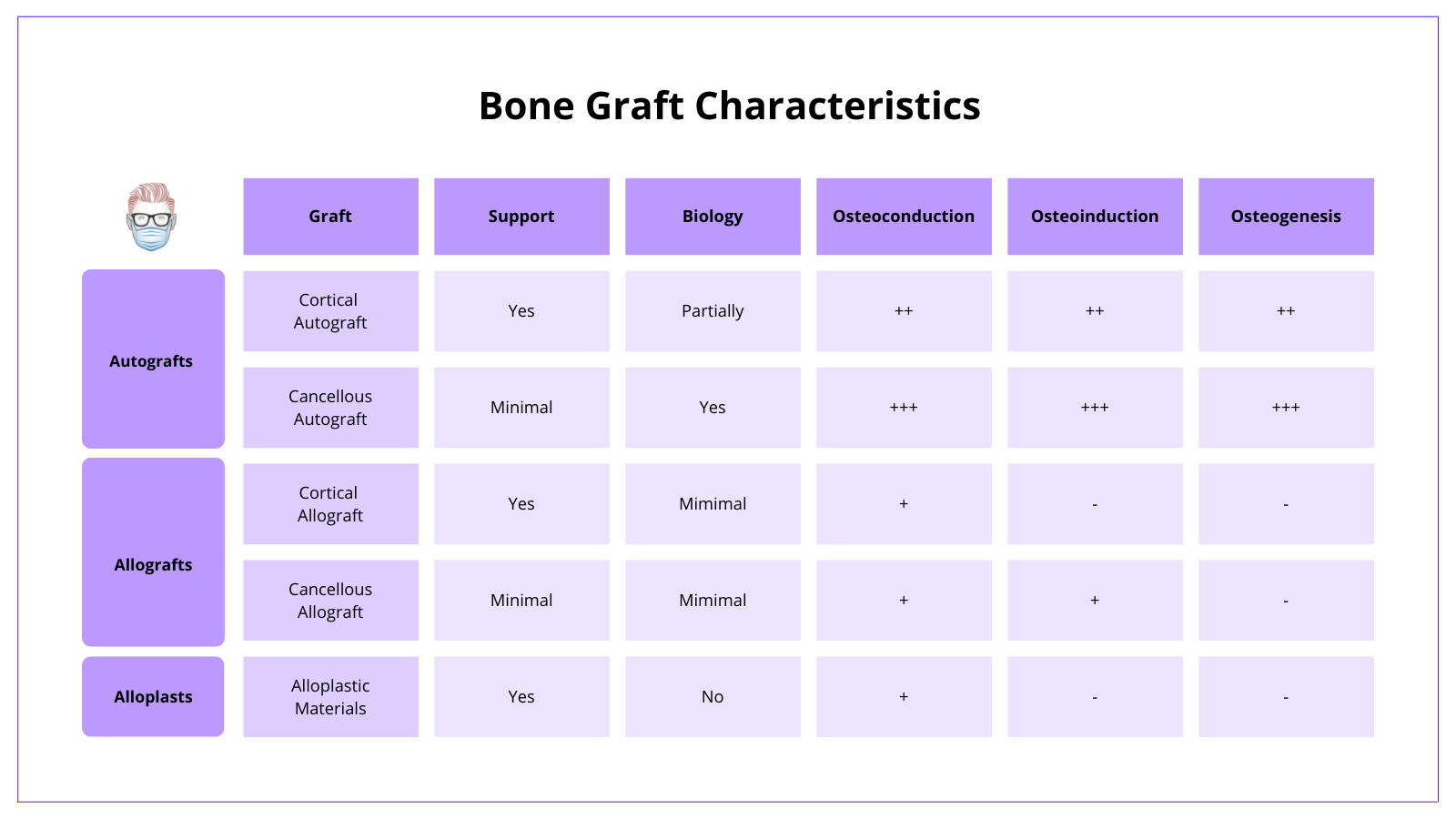
Bone Graft Properties
The biological property of bone focuses on 3 areas - osteoconduction, osteoinduction and osteogenesis. This can be visualised in the image below
Osteoconductive
- Osteoconductive material is a structural framework for bone growth.
- For example, demineralized bone matrices (DBMs)
- More apparent in cancellous bone grafts.
Osteoinductive
- Osteoinductive material stimulates osteogenesis and induces stem cells
- For example, bone morphogenetic protein (BMP) arises from the TGF-B family.
Osteogenic
- Osteogenic material provides bone-producing cells (mesenchymal stem cells, osteoblasts, and osteocytes) to produce more bone.
- For example, an autologous bone graft is the only bone graft that contains live mesenchymal precursor cells
Classification of Bone Grafts
There are several different ways to classify the different types of bone grafts. This image below provides a comprehensive review.
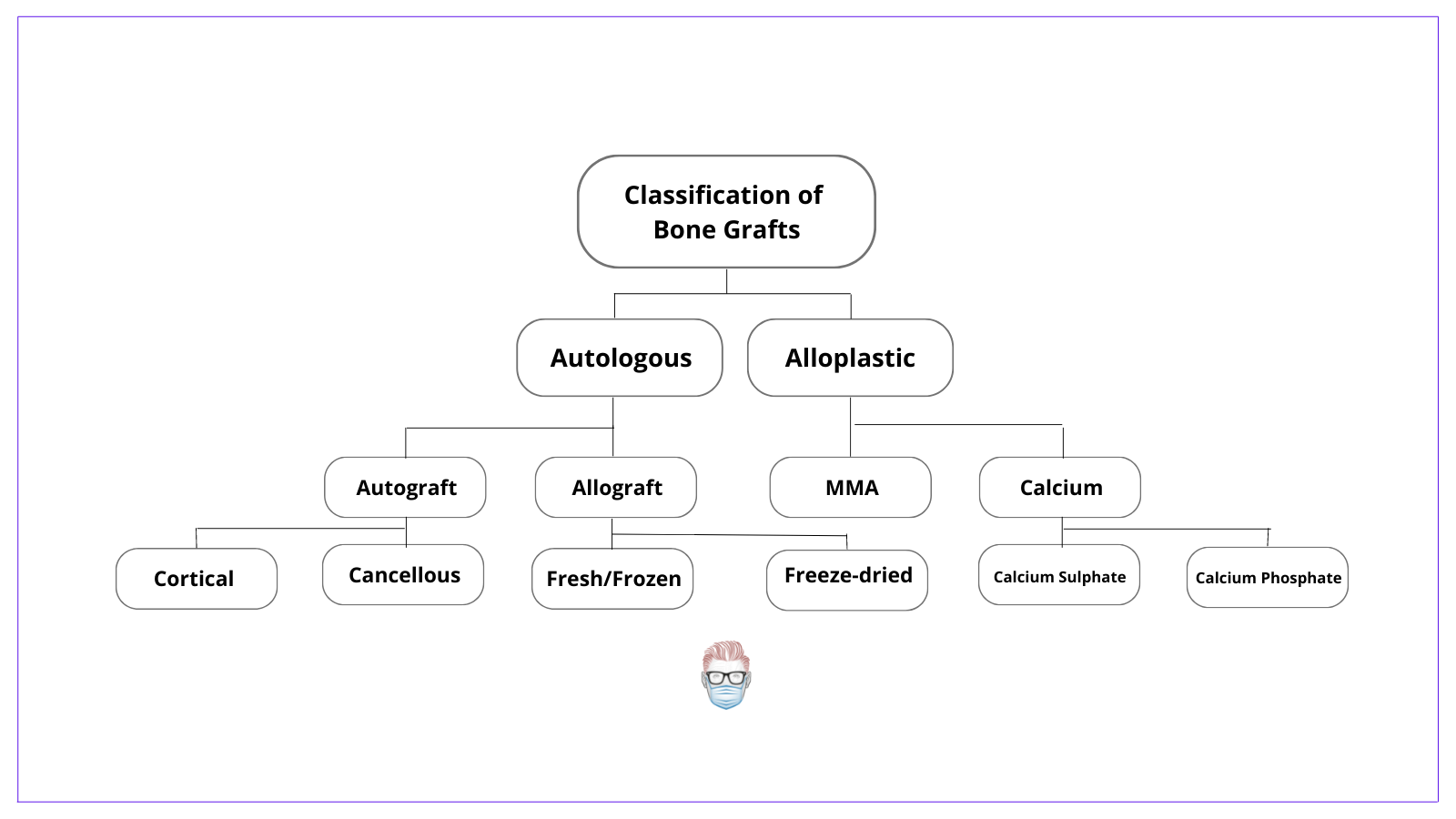
Autologous Bone Autografts
Indications
Bone Autografts are indicated in bone defects <6cm and:
- Well-vascularized bed
- Adequate soft tissue cover
- Absence of infection
Biological Properties
Bone Autografts are considered the "gold standard" because of their biological properties:
- Osteogenic and osteoinductive and osteoconductive properties.
- Less immunogenic than other options.
Types of Autografts
Autografts can be cortical, cancellous or a combination. Each option has its own limitations and advantages. Generally speaking, cortical is used when large defects require structural support.
Cortical Bone Grafts
- Less biologically active than cancellous
- More structural support than cancellous.
- Slower incorporation due to remodelling of Haversian canals (up to 2 months)
- Heals primarily by osteoconduction.
Cancellous Bone Grafts
- An osteoconductive 3D scaffold with minimal structural support
- A high number of osteoblasts and growth factors.
- Rapid incorporation via creeping substitution (within 2 weeks)
- Heals primarily by osteogenesis.
Donor Sites
Donor site options for autografts include:
- Iliac Crest - commonly used and can give cancellous and cortical bone
- Fibula - for a vascular autograft (example - fibula graft with peroneal artery)
- Ribs - for vascular autografts.
- Distal radius
- Bone marrow aspirate
Bone Allografts
Allografts are bone grafts from a (cadaver) donor that can be fresh, freshly frozen or freeze-dried bone derived from a donor.
Bone allografts are osteoconductive only due to a lack of viable cells. It is limited by its immunogenicity.
Alloplastic Bone Substitutes
Alloplastic bone substitutes have a primary role in support. They are primarily osteoconductive with little osteogenic or osteoconductive properties
Here are a few examples:
- Demineralised bone matrix has an osteoinductive and osteoinductive capacity without structural support. It contains collagen, bone morphogenetic proteins, transforming growth factor-beta, residual calcium but does not contain mesenchymal precursor cells.
- Calcium Hydroxyapatite: brittle but limited resorption.
- Methylmethacrylate (MMA): non-resorbable, high density, "bone cement", structural support with osteoconductive properties only.
- Bone morphogenetic proteins (BMP): osteoinductive only
Bone Graft Healing and Incorporation
After haematoma formation and an initial inflammatory period, in which necrotic debris stimulates chemotaxis, bone grafts become incorporated into their new bony surroundings. In a similar way, skin grafting becomes adherent to a wound bed. This is visualised in the image below.
It is different from the standard bone healing process.
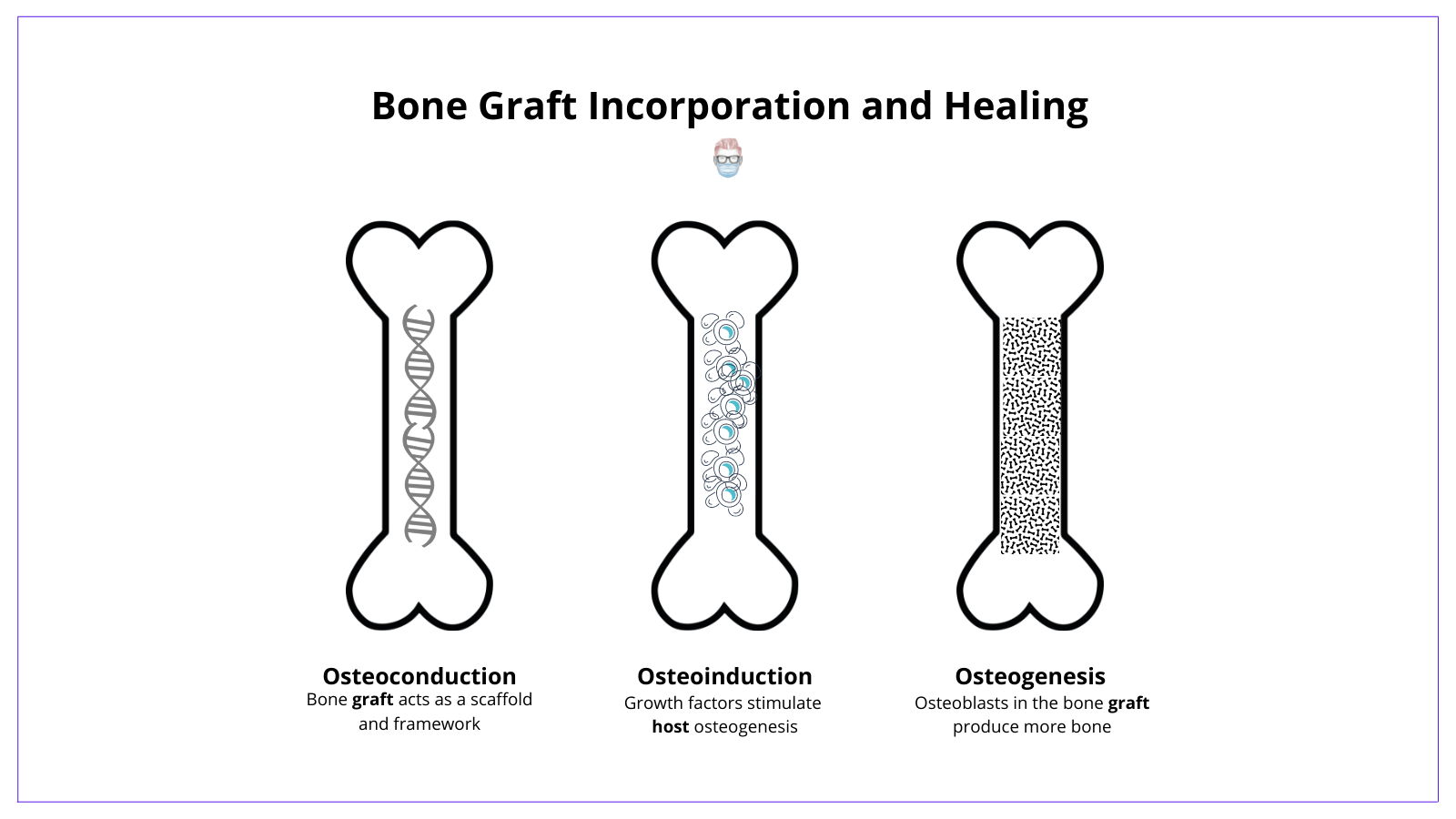
Osteoconduction
- The bone graft acts as a scaffold for bone growth via creeping substitution
- It provides a matrix for bone growth that enables a blood supply and osteoprogenitor cells to survive.
- Occurs in cortical bone, calcium hydroxyapatite, and less so in cancellous bone.
Osteoinduction
- Bone graft growth factors stimulate osteogenesis in the host tissue.
- Osteocytes are formed from the differentiation of the recipient site's mesenchymal cells
- Strongly influenced by BMPs.
- This process is seen in cancellous bone grafts and demineralised bone matrix
Osteogenesis
- Osteoblasts that survive in the bone graft directly produce new bone.
- A faster process in vascularized bone grafts as they do not undergo creeping substitution.
- Occurs primarily in vascularized bone grafts and cancellous bone.
Bone Graft Survival
Patient Factors
A medically optimised patient will always have a better outcome for their bone grafts. For example, diabetes control, smoking cessation and adjusting immunosuppression drugs.
Graft Factors
When it comes to the graft, there are so many variables that can have a positive and negative influence on its healing. Here are some key points:
- Type of Bone Graft
- Periosteum on bone grafts reduces the amount of resorption.
- Cancellous bone grafts are more readily revascularized than cortical.
2. Inset of Bone Graft
- Orthotopic: if the graft is placed in a normal bone location then there will be less bone resorption.
- Fixation: bone graft fixation improves survival.
- Quality of recipient: infection and radiotherapy reduce graft survival.
Flashcards
They are continually updated and are for thePlasticsPro users.
This is for thePlasticsPro
Join the Club to enjoy unlimited access to all of thePlasticsFella.
Join the Club

