Summary Card
Overview
The bilobed flap is a reliable reconstructive option for nasal and facial cutaneous defects, using a double transposition design to redirect tension and preserve aesthetic contours.
Indications
The bilobed flap is especially useful for small to moderate-sized nasal and facial defects, offering excellent colour/texture match, minimized tension, and improved aesthetic outcomes compared to simple grafts.
Flap Design
The bilobed flap is a double transposition design comprising two lobes rotating around a single pivot point, effectively distributing tension and preserving aesthetic contours for facial reconstruction.
Complications
Although bilobed flaps generally yield excellent reconstructive outcomes, complications often stem from poor planning, flap design errors, or surgical technique.
Updated by: Dr Kurt Lee Chircop, Educational Fellow.
Verified by thePlasticsFella ✅
Overview of Bilobed Flaps
The bilobed flap is a time-tested, reliable reconstructive option for nasal and facial cutaneous defects, using a double transposition design to redirect tension and preserve aesthetic contours.
The bilobed flap is a classic yet continually refined technique for closing cutaneous defects, especially on the nose. Its unique design permits redistribution of wound closure tension away from critical aesthetic landmarks, ensuring both functional and cosmetic success.
This flap combines principles of rotation and transposition to achieve tension-free closure using adjacent tissue.
- Double Transposition Design: The flap consists of two lobes rotating around a single pivot point. This design allows redistribution of tension vectors over a broader area, reducing stress on any single region (Grieco, 2018),
- Random Pattern Flap: It does not rely on a named vascular pedicle but rather uses the subdermal plexus for perfusion, increasing its versatility in different anatomical regions.
- Primary and Secondary Defect Closure: It simultaneously addresses the main defect and the donor site, reducing the need for distant grafts or flaps. The shared pivot point allows each lobe to recruit skin from regions with more laxity, optimizing flap mobility and minimizing dog-ears or buckling (Cook, 2006).
The flap has evolved from a simple concept to a precisely executed modern surgical tool.
- Esser (1918): First described the bilobed flap for nasal defects, focusing on using local tissue for facial reconstruction. This original design included two lobes of equal size, each rotating 90°.
- Zitelli (1989): Refined the design by modifying angles and dimensions, leading to improved contour and decreased distortion, particularly in the nasal tip and ala. First and second lobes rotate 45–50° each, for a total arc of 90–100°.
If designed correctly, the bilobed flap minimizes upward pull and prevents distortion of the alar margin — key for preserving the natural nasal contour.
Indications for Bilobed Flaps
The bilobed flap is especially useful for small to moderate-sized nasal and facial defects, offering excellent color/texture match, minimized tension, and improved aesthetic outcomes compared to simple grafts.
The bilobed flap is most commonly used in nasal reconstruction, particularly the distal nasal tip and ala, where aesthetics and contour preservation are critical.
- Size Suitability: Best for defects <1.5 cm on the nasal tip, where sebaceous skin thickness requires a robust, shape-preserving technique (Steiger, 2011).
- Avoidance of Graft Limitations: Provides superior contour and texture compared to skin grafts, which may contract or appear mismatched (Cook, 2000)
- Local Tissue Match: Uses adjacent, color- and texture-matched tissue for a natural appearance, essential in high-visibility regions (Salgarelli, 2010).
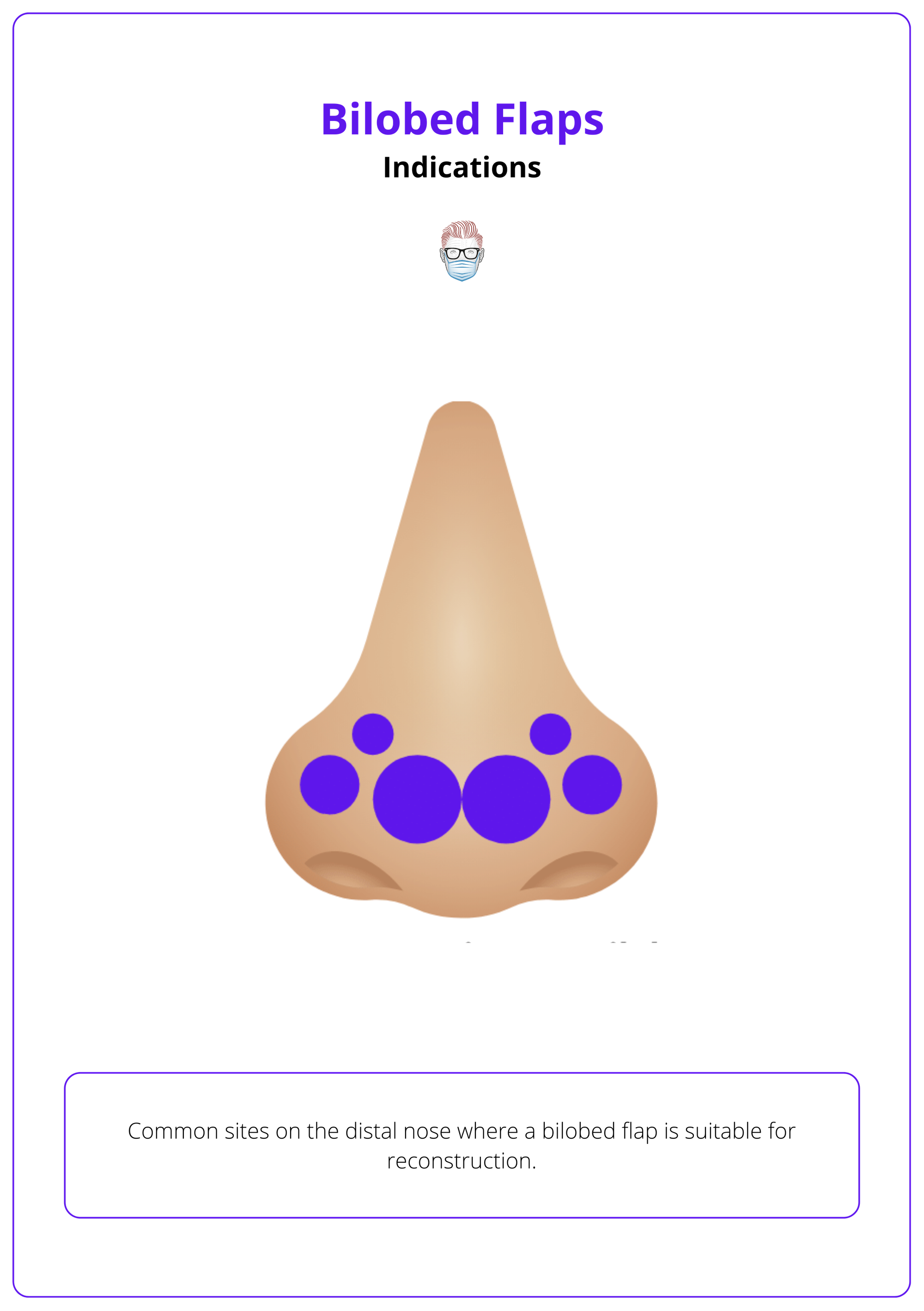
The illustration below shows common sites on the distal nose where a bilobed flap is suitable for reconstruction.
While classically nasal in application, bilobed flap principles have been successfully adapted to several other anatomical regions.
- Cheek, Periorbital, and Perioral Areas: Suitable for concave or mobile facial zones, offering predictable healing and contour adaptation.
- Temporal Forehead Defects: Allows large post-oncologic defects to be closed in one stage with excellent contour restoration using medially/laterally based bilobed designs (Sutton, 1992).
- Forearm Flap Donor Sites: A perforator-based bilobed flap (ulnar artery) allows primary closure of small to medium radial forearm flap donor sites, reducing morbidity and supporting early rehabilitation (Hsieh, 2004).
- DIP Joint (DIPJ) Wound Coverage: A refined bilobed flap technique provides aesthetic and functional coverage after mucous cyst excision at the distal interphalangeal joint (Jimenez, 2017).
Position alar defects at least 1 cm from the alar margin to prevent margin distortion and ensure a smooth, natural alar contour during healing.
Bilobed Flap Design
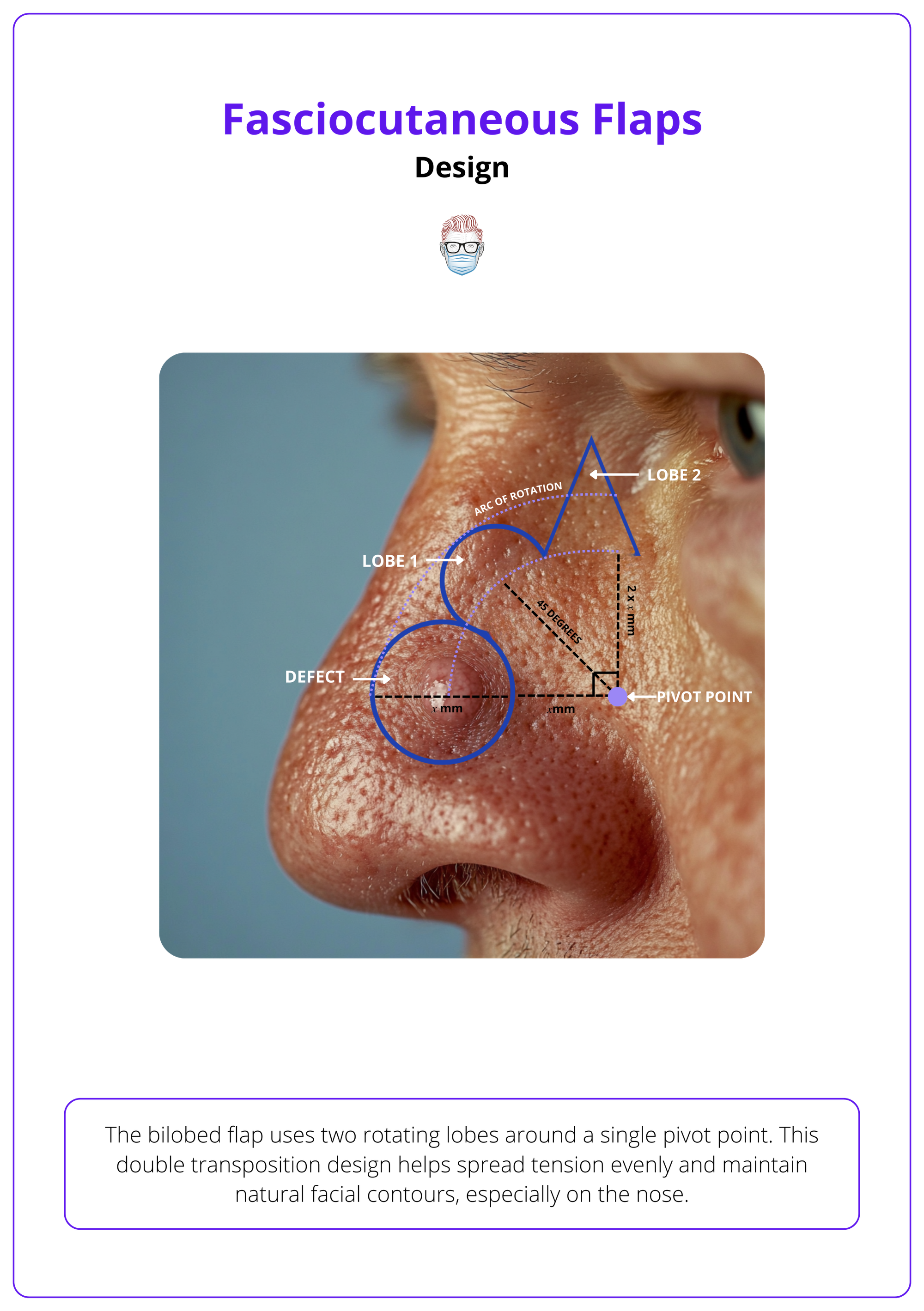
The bilobed flap uses two rotating lobes around a single pivot point. This double transposition design helps spread tension evenly and maintain natural facial contours, especially on the nose.
Key Principles
The bilobed flap uses geometric planning and tissue movement to achieve reliable, aesthetic reconstruction. Its success depends on maintaining key proportions:
- Lobe Sizes: The first lobe should match the width of the defect. The second lobe should be slightly smaller to minimize tension and avoid dog-ear formation.
- Angles: The first lobe is set at a 45° angle from the defect, and the second lobe at 90° from the pivot point.
- Pivot Point: Located one defect-width away from the edge of the original defect.
Originally developed by Esser in 1918, the first bilobed flap used two equal-sized lobes, each rotating 90°. This created a 180° arc. Zitelli later refined the design, reducing the rotation to 45–50° per lobe. This is visualised in the image below.

Steps to Bilobed Flap
Understanding the geometry of each element ensures successful planning, rotation, and inset of the flap. The key steps are as follows.
Flap Design
- Measure the Defect: Use the diameter as your base for all further measurements.
- Mark the Pivot Point: Place it one defect-width away from the defect's edge.
- Draw Lobe A (Primary): At a 45° angle from the pivot point, matching the defect’s width.
- Draw Lobe B (Secondary): At a 90° angle, slightly smaller and often triangular (Steiger, 2011).
- Excise a Standing Cutaneous Defect (SCD): Remove a small triangle of tissue between the defect and pivot to allow flap rotation without bunching.
The 3-2-1 mnemonic simplifies geometric flap planning with 1 pivot point (one defect away), 2 lobes angled at 45°, and 3 incisions (defect, primary, and secondary lobes).
Flap Raising
- Dissection Plane: Can be subcutaneous, submuscular, or periosteal—depending on the defect depth.
- Undermining: Widely undermine to allow smooth rotation and reduce tension.
- Instruments: Use skin hooks, not forceps, to avoid trauma.
- Thinning: Carefully thin the flap to match nasal contour, but preserve subdermal vascularity
Suturing
- Tension Check: Ensure the flap rotates freely before suturing.
- Step 1: Close Lobule B donor site first to anchor the flap.
- Step 2: Rotate the primary lobe into the defect.
- Step 3: Use layered closure with deep sutures to minimize dead space and avoid pincushioning.
- Step 4: Complete with fine skin sutures, respecting skin tension lines (Wang, 2014). (Wang, 2014).
Superiorly based bilobed flaps reduce nasal tip distortion more effectively than lateral flaps. They are especially useful for larger or cephalic defects, offering better contour control and lower complication rates (Kelly-sell, 2018).
Complications of Bilobed Flaps
While bilobed flaps are highly effective for facial reconstruction, complications typically arise from poor planning, incorrect flap dimensions, or suboptimal surgical technique.
Advantages of Bilobed Flaps
Bilobed flaps are designed as random pattern flaps, meaning they rely on the subdermal plexus for blood supply. This gives them several advantages over other local flaps:
- Strong Vascularity: Excellent perfusion reduces the risk of flap loss (Cook, 2000).
- Tension Redistribution: Using two lobes spreads tension more evenly than a single flap, reducing stress on any one point (Steiger, 2011).
- Extended Reach: They allow movement of more skin over a greater distance than single transposition flaps like the rhomboid flap.
- One-Stage Repair: Enables reconstruction using local tissue with matching texture and color (Salgarelli, 2010).
Despite these strengths, outcomes depend heavily on meticulous design and execution.
Complications of Bilobed Flaps
- Alar Retraction: The alar rim pulls upward or distorts, affecting nasal contour. Commonly due to undersized primary lobes or improper placement of the secondary defect. Reported in up to 5% of cases (Cho, 2006). Minimisation strategy should include:
- Standing Cone and Dog-Ears: Raised puckers of skin at closure points, or tissue bunching at lobe junctions. Often from failing to account for excess skin or improper arc design. Minimisation strategy should include:
- Excise a triangular wedge (standing cutaneous deformity) between the defect and pivot point to create space for flap rotation.
- Properly size the second lobe — slightly smaller than the first — to reduce redundancy.
- Trapdoor Effect (Pincushioning): The central area of the flap bulges above the skin surface. Due to excessive bulk or inadequate tissue thinning. Minimisation strategy should include:
- Carefully thin the lobes to match the surrounding nasal contour.
- Use layered suturing to flatten the flap and avoid central elevation (Cook, 2006).
- Flap Necrosis (Rare): Partial or full flap loss from poor blood flow caused by aggressive thinning or tension that compromises vascularity. Minimisation strategy should include:
- Avoid over-thinning, especially in distal lobe tips.
- Handle tissues gently — use skin hooks instead of forceps — and elevate flaps on a reliable vascular plane.
- Confirm tension-free rotation intraoperatively before suturing.
- Donor Site Scarring: Visible or asymmetric scars at the flap harvest site. Misaligned incisions or excessive tension during closure. Minimisation strategy should include:
- Align incisions with relaxed skin tension lines for better healing (Cook, 2000).
- Choose mobile, less sebaceous skin (like nasal dorsum or sidewall) for the second lobe to allow smoother closure.
Conclusion
1. Overview: The bilobed flap is a double transposition flap ideal for small to moderate nasal and facial cutaneous defects, redirecting tension to preserve contours.
2. Indications: It’s best used for nasal tip or ala defects <1.5 cm, offering excellent vascularity, contour match, and reduced distortion versus grafts.
4. Design: The Zitelli modification rotates two lobes 45–50° around a pivot, distributing tension and minimizing dog-ears or standing cones.
5. Flap Geometry: Use the “3-2-1” mnemonic: 3 radii, 2 angles (45°), 1 pivot point — key to consistent design and easy intraoperative planning.
6. Complications: Issues like alar retraction, dog-ears, trapdoor deformity, or necrosis stem from poor flap planning, tension, or excess thinning.
Further Reading
- Cook, Jonathan L. "Reconstructive utility of the bilobed flap: lessons from flap successes and failures." Dermatologic surgery 31 (2005): 1024-1033.
- Grieco MP, Bertozzi N, Grignaffini E, Raposio E. Nose defects reconstruction with the Zitelli bilobed flap. G Ital Dermatol Venereol. 2018 Apr;153(2):278-282.
- Cook, Jonathan L. "A review of the bilobed flap's design with particular emphasis on the minimization of alar displacement." Dermatologic surgery 26.4 (2000): 354-362.
- Salgarelli, Attilio Carlo, et al. "The bilobed flap in skin cancer of the face: our experience on 285 cases." Journal of Cranio-Maxillofacial Surgery 38.6 (2010): 460-464.
- Steiger, Jacob D. "Bilobed flaps in nasal reconstruction." Facial Plastic Surgery Clinics 19.1 (2011): 107-111.
- Zitelli, John A. "Design aspect of the bilobed flap." Archives of Facial Plastic Surgery (2008).
- Wang, Zhi-Guo, Xiu-Juan Chen, and Zhen-Yu Chen. "A modified bilobed flap design for nasal tip defects." Plastic and Aesthetic Research 1 (2014): 16-20.
- Kelly-Sell M, Hollmig ST, Cook J. The superiorly based bilobed flap for nasal reconstruction. J Am Acad Dermatol. 2018 Feb;78(2):370-376.
- Cho, Michael, and David W. Kim. "Modification of the Zitelli bilobed flap." Archives of Facial Plastic Surgery (2006).
- Sutton, Andrew E., and Vito C. Quatela. "Bilobed flap reconstruction of the temporal forehead." Archives of Otolaryngology–Head & Neck Surgery 118.9 (1992): 978-982.
- Hsieh, Ching-Hua, et al. "Primary closure of radial forearm flap donor defects with a bilobed flap based on the fasciocutaneous perforator of the ulnar artery." Plastic and reconstructive surgery 113.5 (2004): 1355-1360.
- Jiménez, Isidro, Pedro J. Delgado, and Ricardo Kaempf de Oliveira. "The Zitelli bilobed flap on skin coverage after mucous cyst excision: a retrospective cohort of 33 cases." The Journal of Hand Surgery 42.7 (2017): 506-510.


